Clin Endosc.
2024 Mar;57(2):196-202. 10.5946/ce.2023.010.
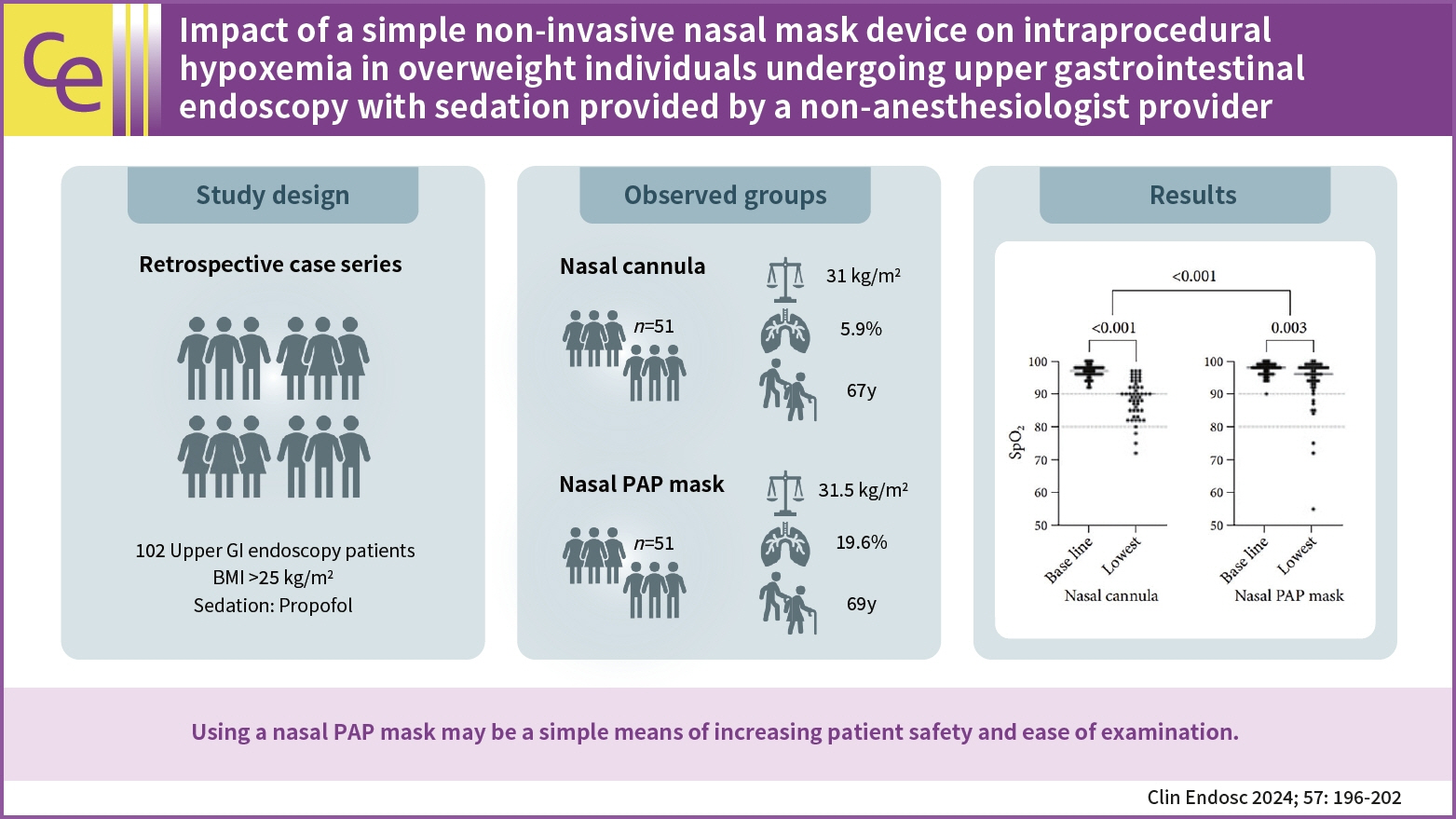
Impact of a simple non-invasive nasal mask device on intraprocedural hypoxemia in overweight individuals undergoing upper gastrointestinal endoscopy with sedation provided by a non-anesthesiologist provider
- Affiliations
-
- 1Department of Gastroenterology, Hepatology and Interventional Endoscopy, Asklepios Hospital Barmbek, Hamburg, Germany
- 2Semmelweis University of Medicine, Asklepios Campus Hamburg, Hamburg, Germany
- 3Asklepios Proresearch Research Institute, Hamburg, Germany
- 4Department of Anesthesiology and Surgical Critical Care, Asklepios Hospital Barmbek, Hamburg, Germany
- 5Department of Pneumology and Medical Critical Care, Asklepios Hospital Barmbek, Hamburg, Germany
- KMID: 2553756
- DOI: http://doi.org/10.5946/ce.2023.010
Abstract
- Background/Aims
Hypoxemia is a common side effect of propofol sedation during endoscopy. Applying mild positive airway pressure (PAP) using a nasal mask may offer a simple way to reduce such events and optimize the conditions for diagnostic and therapeutic upper gastrointestinal endoscopies.
Methods
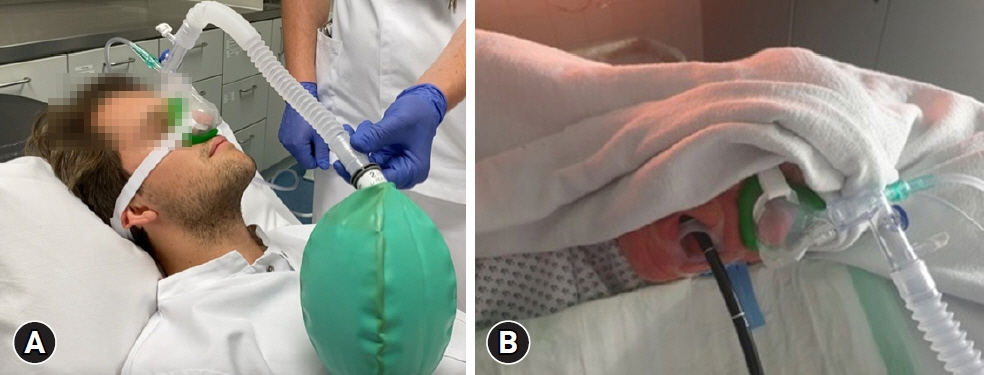
We compared overweight patients (body mass index >25 kg/m2) with a nasal PAP mask or standard nasal cannula undergoing upper gastrointestinal endoscopies by non-anesthesiologists who provided propofol sedation. Outcome parameters included the frequency and severity of hypoxemic episodes.
Results
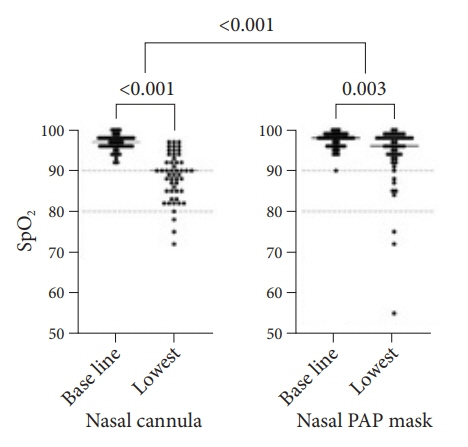
We analyzed 102 procedures in 51 patients with nasal PAP masks and 51 controls. Episodes of hypoxemia (oxygen saturation [SpO2] <90% at any time during sedation) occurred in 25 (49.0%) controls compared to 8 (15.7%) patients with nasal PAP masks (p<0.001). Severe hypoxemia (SpO2 <80%) occurred in three individuals (5.9%) in both groups. The mean delta between baseline SpO2 and the lowest SpO2 recorded was significantly decreased among patients with nasal PAP mask compared to controls (3.7 and 8.2 percentage points difference, respectively). There were significantly fewer airway interventions performed in the nasal PAP mask group (15.7% vs. 41.2%, p=0.008).
Conclusions
Using a nasal PAP mask may be a simple means of increasing patient safety and ease of examination.
Keyword
Figure
Reference
-
1. Riphaus A, Wehrmann T, Hausmann J, et al. [S3-guidelines "sedation in gastrointestinal endoscopy" 2014 (AWMF Register No. 021/014)]. Z Gastroenterol. 2015; 53:802–842.2. Dumonceau JM, Riphaus A, Schreiber F, et al. Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates guideline: updated June 2015. Endoscopy. 2015; 47:1175–1189.3. Singh H, Poluha W, Cheung M, et al. Propofol for sedation during colonoscopy. Cochrane Database Syst Rev. 2008; 2008:CD006268.4. Eastwood PR, Platt PR, Shepherd K, et al. Collapsibility of the upper airway at different concentrations of propofol anesthesia. Anesthesiology. 2005; 103:470–477.5. Nieuwenhuijs D, Sarton E, Teppema LJ, et al. Respiratory sites of action of propofol: absence of depression of peripheral chemoreflex loop by low-dose propofol. Anesthesiology. 2001; 95:889–895.6. de Paulo GA, Martins FP, Macedo EP, et al. Sedation in gastrointestinal endoscopy: a prospective study comparing nonanesthesiologist-administered propofol and monitored anesthesia care. Endosc Int Open. 2015; 3:E7–E13.7. Wani S, Azar R, Hovis CE, et al. Obesity as a risk factor for sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Gastrointest Endosc. 2011; 74:1238–1247.8. Dimou F, Huynh S, Dakin G, et al. Nasal positive pressure with the SuperNO2VA device decreases sedation-related hypoxemia during pre-bariatric surgery EGD. Surg Endosc. 2019; 33:3828–3832.9. Bai Y, Xu Z, Chandrashekar M, et al. Comparison of a simplified nasal continuous positive airways pressure device with nasal cannula in obese patients undergoing colonoscopy during deep sedation: a randomised clinical trial. Eur J Anaesthesiol. 2019; 36:633–640.10. McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc. 2008; 67:910–923.11. Peveling-Oberhag J, Michael F, Tal A, et al. Capnography monitoring of non-anesthesiologist provided sedation during percutaneous endoscopic gastrostomy placement: a prospective, controlled, randomized trial. J Gastroenterol Hepatol. 2020; 35:401–407.12. Beitz A, Riphaus A, Meining A, et al. Capnographic monitoring reduces the incidence of arterial oxygen desaturation and hypoxemia during propofol sedation for colonoscopy: a randomized, controlled study (ColoCap Study). Am J Gastroenterol. 2012; 107:1205–1212.13. Klare P, Reiter J, Meining A, et al. Capnographic monitoring of midazolam and propofol sedation during ERCP: a randomized controlled study (EndoBreath Study). Endoscopy. 2016; 48:42–50.14. Hung KC, Chang YJ, Chen IW, et al. Efficacy of high flow nasal oxygenation against hypoxemia in sedated patients receiving gastrointestinal endoscopic procedures: a systematic review and meta-analysis. J Clin Anesth. 2022; 77:110651.15. Horiuchi A, Graham DY. High-flow nasal cannula oxygen therapy obscures severe respiration depression, providing an illusion of safety. Gastrointest Endosc. 2020; 91:720–721.16. Goudra B, Gouda G, Singh PM. Recent developments in devices used for gastrointestinal endoscopy sedation. Clin Endosc. 2021; 54:182–192.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Developments in Devices Used for Gastrointestinal Endoscopy Sedation
- Anesthesia and Sedation
- Adverse events of conscious sedation using midazolam for gastrointestinal endoscopy
- Core curriculum for sedation in gastrointestinal endoscopy with a focus on practice: a proposal from the Korean Society of Gastrointestinal Endoscopy
- The Effect of Oxygen Asministration by Reservoir Tube During Immediate Postoperative Period