J Korean Med Sci.
2024 Mar;39(9):e95. 10.3346/jkms.2024.39.e95.
Trends in Incidence and Drug Prescriptions for Croup in Children Under 5 Years of Age: A 2002–2019 Population-Based Study
- Affiliations
-
- 1Department of Pediatrics, Kyung Hee University Medical Center, Kyung Hee University College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea
- 3Department of Orthopaedic Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 4Department of Pediatrics, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- KMID: 2553340
- DOI: http://doi.org/10.3346/jkms.2024.39.e95
Abstract
- Background
Tracking national croup trends can provide important insights for childhood health management. This study aimed to analyze the incidence and drug prescription trends in Korean children over a two-decade period.
Methods
This population-based study encompassed 479,783 children aged < 5 years from 2002–2019, utilizing the National Health Insurance Service-National Sample Cohort. We identified participants with a primary croup diagnosis who were admitted to or visited the emergency room. Age-specific and age-adjusted incidence rates/10,000 person-years were calculated. We assessed using orthogonal polynomial contrasts and stratified by various factors (sex, age, residential area, economic status, comorbidities, and healthcare facility types). We observed changes in the use of five medications: inhaled steroids, systemic steroids, inhaled epinephrine, antibiotics, and short-acting bronchodilators. Generalized binomial logistic regression was used to analyze factors influencing prescription strategies.
Results
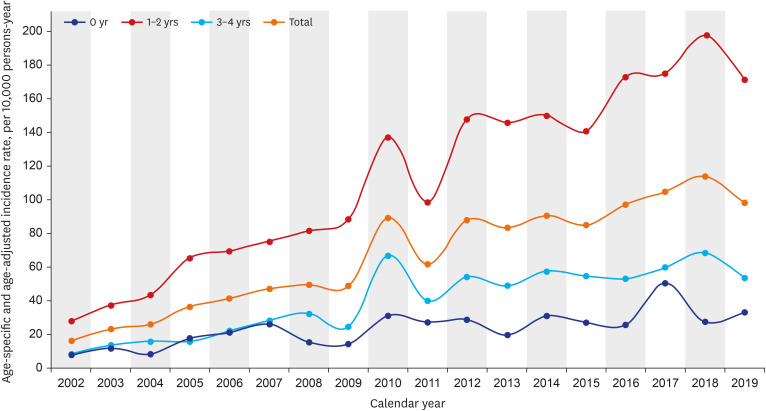
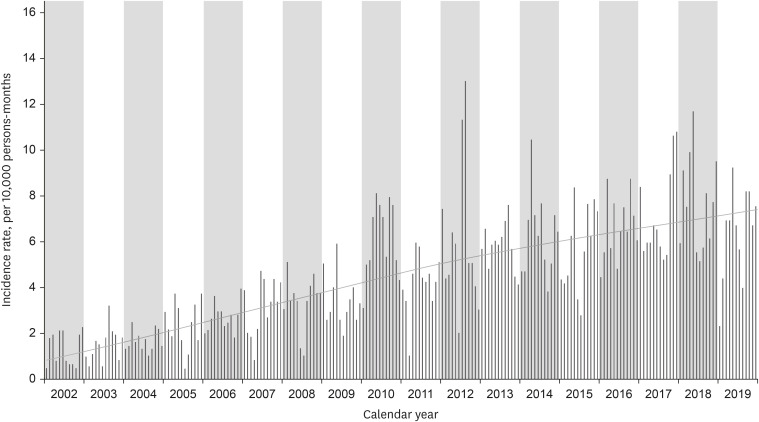
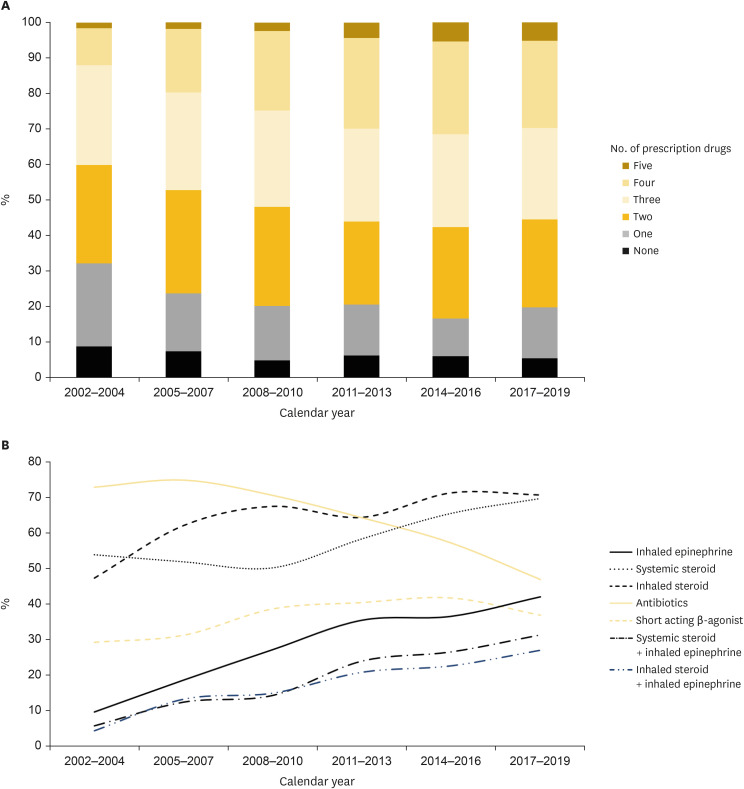
In 2002, the croup-related visits were 16.1/10,000 person-years, increasing to 98.3 in 2019 (Pfor trend < 0.001). This trend persisted, regardless of age, sex, region, and economic status. Children with comorbid atopic dermatitis or asthma maintained consistent croup rates, while those without comorbidities increased. Treatment trends showed decreasing antibiotic (73–47%) and oxygen use (21.3–3.4%), with increasing nebulized epinephrine (9.3–41.5%) and multiple drug prescriptions (67.8–80.3%). Primary care centers exhibited a greater increase in prescription usage and hospitalization duration than did tertiary healthcare institutions.
Conclusion
Over the past two decades, croup incidence has risen, accompanied by increased epinephrine use and decreased antibiotic prescriptions. Longer hospitalization and higher medication use were mainly observed in primary care facilities.
Keyword
Figure
Reference
-
1. Cherry JD. Clinical practice. Croup. N Engl J Med. 2008; 358(4):384–391. PMID: 18216359.2. Petrocheilou A, Tanou K, Kalampouka E, Malakasioti G, Giannios C, Kaditis AG. Viral croup: diagnosis and a treatment algorithm. Pediatr Pulmonol. 2014; 49(5):421–429. PMID: 24596395.3. Bjornson CL, Johnson DW. Croup. Lancet. 2008; 371(9609):329–339. PMID: 18295000.4. Denny FW, Murphy TF, Clyde WA Jr, Collier AM, Henderson FW, Senior RS, et al. Croup: an 11-year study in a pediatric practice. Pediatrics. 1983; 71(6):871–876. PMID: 6304611.5. Kim KR, Park H, Kim DR, Kim YJ. Changes in epidemiology of parainfluenza virus and respiratory syncytial virus infection during coronavirus disease 2019 pandemic in Korea. Clin Exp Pediatr. 2022; 65(6):320–321. PMID: 35287257.6. Segal AO, Crighton EJ, Moineddin R, Mamdani M, Upshur RE. Croup hospitalizations in Ontario: a 14-year time-series analysis. Pediatrics. 2005; 116(1):51–55. PMID: 15995030.7. Marx A, Török TJ, Holman RC, Clarke MJ, Anderson LJ. Pediatric hospitalizations for croup (laryngotracheobronchitis): biennial increases associated with human parainfluenza virus 1 epidemics. J Infect Dis. 1997; 176(6):1423–1427. PMID: 9395350.8. Rosychuk RJ, Klassen TP, Voaklander DC, Senthilselvan A, Rowe BH. Seasonality patterns in croup presentations to emergency departments in Alberta, Canada: a time series analysis. Pediatr Emerg Care. 2011; 27(4):256–260. PMID: 21490537.9. Rihkanen H, Rönkkö E, Nieminen T, Komsi KL, Räty R, Saxen H, et al. Respiratory viruses in laryngeal croup of young children. J Pediatr. 2008; 152(5):661–665. PMID: 18410770.10. Lee YJ, Kim HB, Kim BS, Kim CK, Kim CH, Kim HY, et al. Seasonal patterns and etiologies of croup in children during the period 2010–2015: a multicenter retrospective study. Allergy Asthma Respir Dis. 2019; 7(2):78–85.11. Doull I. Corticosteroids in the management of croup. BMJ. 1995; 311(7015):1244. PMID: 7496221.12. Bjornson C, Russell KF, Vandermeer B, Durec T, Klassen TP, Johnson DW. Nebulized epinephrine for croup in children. Cochrane Database Syst Rev. 2011; (2):CD006619. PMID: 21328284.13. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID: 26822938.14. Kim JH, Lee JE, Shim SM, Ha EK, Yon DK, Kim OH, et al. Cohort profile: national investigation of birth cohort in Korea study 2008 (NICKs-2008). Clin Exp Pediatr. 2021; 64(9):480–488. PMID: 33445832.15. Kim OH, Lee SW, Ha EK, Kim JH, Jo YH, Rhie S, et al. Neurodevelopmental outcomes and comorbidities of children with congenital muscular torticollis: evaluation using the National Health Screening Program for Infants and Children database. Clin Exp Pediatr. 2022; 65(6):312–319. PMID: 34886594.16. Naing NN. Easy way to learn standardization: direct and indirect methods. Malays J Med Sci. 2000; 7(1):10–15. PMID: 22844209.17. Rosychuk RJ, Klassen TP, Metes D, Voaklander DC, Senthilselvan A, Rowe BH. Croup presentations to emergency departments in Alberta, Canada: a large population-based study. Pediatr Pulmonol. 2010; 45(1):83–91. PMID: 19953656.18. Hanna J, Brauer PR, Morse E, Berson E, Mehra S. Epidemiological analysis of croup in the emergency department using two national datasets. Int J Pediatr Otorhinolaryngol. 2019; 126:109641. PMID: 31442871.19. Lee SJ, Lee SH, Ha EK, Sheen YH, Sung MS, Jung YH, et al. Prevalence of respiratory virus infection with regard to age, sex, and seasonality factors: a single center experience against children hospitalized during the 10 years. Allergy Asthma Respir Dis. 2017; 5(6):320–325.20. Ham H, Jang J, Choi S, Oh S, Jo S, Choi S, et al. Epidemiological characterization of respiratory viruses detected from acute respiratory patients in Seoul. Ann Clin Microbiol. 2013; 16(4):188–195.21. Lee H, Lee CK, Nam MH, Roh KH, Yoon SY, Lim CS, et al. Epidemiologic features of parainfluenza virus type 1, 2 and 3 infection in Seoul and a neighboring area, 2008-2011. Korean J Clin Microbiol. 2012; 15(2):54–59.22. Lee SJ, Lee SH, Ha EK, Sheen YH, Sung MS, Jung YH, et al. Prevalence of respiratory virus infection with regard to age, sex, and seasonality factors: a single center experience against children hospitalized during the 10 years. Allergy Asthma Respir Dis. 2017; 5(6):320–325.23. Kim SH, Huh JH, Bae SY, Kim JS, Yoon SY, Lim CS, et al. Epidemiology of respiratory viral infection in 2004-2006. Korean J Lab Med. 2006; 26(5):351–357. PMID: 18156750.24. Seo JJ, Kim MJ, Kim SH, Kee HY, Chung JK, Kim E, et al. Characterization of respiratory viral infection in children in Gwangju. Infect Chemother. 2008; 40(4):218–229.25. Bass JW, Bruhn FW, Merritt WT. Corticosteroids and racemic epinephrine with IPPB in the treatment of croup. J Pediatr. 1980; 96(1):173–174. PMID: 6985659.26. Koren G, Frand M, Barzilay Z, MacLeod SM. Corticosteroid treatment of laryngotracheitis v spasmodic croup in children. Am J Dis Child. 1983; 137(10):941–944. PMID: 6688500.27. Yates RW, Doull IJ. A risk-benefit assessment of corticosteroids in the management of croup. Drug Saf. 1997; 16(1):48–55. PMID: 9010642.28. Connors K, Gavula D, Terndrup T. The use of corticosteroids in croup: a survey. Pediatr Emerg Care. 1994; 10(4):197–199. PMID: 7937294.29. Geelhoed GC, Macdonald WB. Oral and inhaled steroids in croup: a randomized, placebo-controlled trial. Pediatr Pulmonol. 1995; 20(6):355–361. PMID: 8649914.30. Westley CR, Cotton EK, Brooks JG. Nebulized racemic epinephrine by IPPB for the treatment of croup: a double-blind study. Am J Dis Child. 1978; 132(5):484–487. PMID: 347921.31. Taussig LM, Castro O, Beaudry PH, Fox WW, Bureau M. Treatment of laryngotracheobronchitis (croup). Use of intermittent positive-pressure breathing and racemic epinephrine. Am J Dis Child. 1975; 129(7):790–793. PMID: 1096594.32. Brown JC. The management of croup. Br Med Bull. 2002; 61(1):189–202. PMID: 11997306.33. Johnson D. Croup. Clin Evid. 2005; (14):310–327. PMID: 16620410.34. Kaditis AG, Wald ER. Viral croup: current diagnosis and treatment. Pediatr Infect Dis J. 1998; 17(9):827–834. PMID: 9779773.35. Klassen TP. Croup. A current perspective. Pediatr Clin North Am. 1999; 46(6):1167–1178. PMID: 10629679.36. Tyler A, McLeod L, Beaty B, Juarez-Colunga E, Birkholz M, Hyman D, et al. Variation in inpatient croup management and outcomes. Pediatrics. 2017; 139(4):e20163582. PMID: 28292873.37. Choi YY, Kim YS, Lee SY, Sim J, Choe YJ, Han MS. Croup as a manifestation of SARS-CoV-2 omicron variant infection in young children. J Korean Med Sci. 2022; 37(20):e140. PMID: 35607737.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Seasonality and etiology of croup in pediatric patients hospitalized with lower respiratory tract infections: A long-term study between 2009 and 2017
- Croup as a Manifestation of SARSCoV-2 Omicron Variant Infection in Young Children
- Incidence and Mortality Trends in Critically Ill Children: A Korean Population-Based Study
- Clinical characteristics of children and adolescents with croup and epiglottitis who visited 146 Emergency Departments in Korea
- Decrease in Oxygen Saturation with Pulse Oximetry Caused by Postintubation Croup in Pediatric Patients