J Korean Med Sci.
2024 Mar;39(9):e87. 10.3346/jkms.2024.39.e87.
Pre-Sepsis Length of Hospital Stay and Mortality: A Nationwide Multicenter Cohort Study
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Critical Care Medicine, Seoul National University Hospital, Seoul, Korea
- 4Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2553336
- DOI: http://doi.org/10.3346/jkms.2024.39.e87
Abstract
- Background
Prolonged length of hospital stay (LOS) is associated with an increased risk of hospital-acquired conditions and worse outcomes. We conducted a nationwide, multicenter, retrospective cohort study to determine whether prolonged hospitalization before developing sepsis has a negative impact on its prognosis.
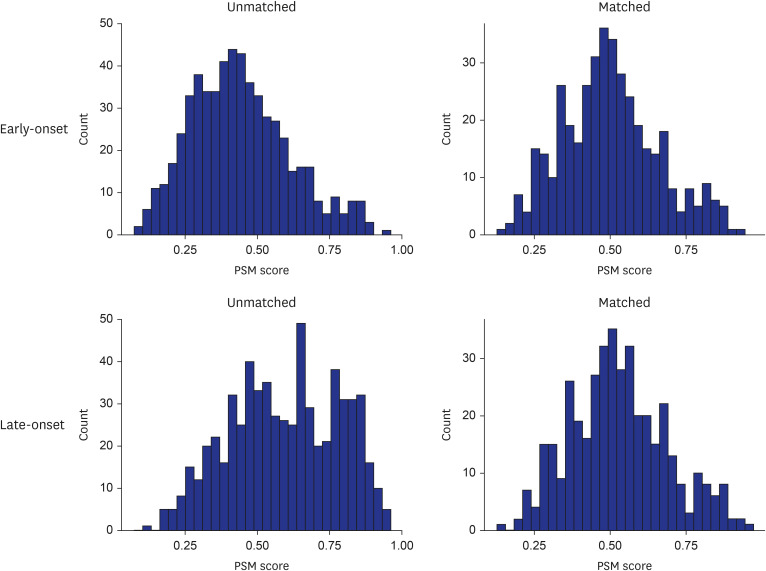
Methods
We analyzed data from 19 tertiary referral or university-affiliated hospitals between September 2019 and December 2020. Adult patients with confirmed sepsis during hospitalization were included. In-hospital mortality was the primary outcome. The patients were divided into two groups according to their LOS before the diagnosis of sepsis: early- (< 5 days) and late-onset groups (≥ 5 days). Conditional multivariable logistic regression for propensity score matched-pair analysis was employed to assess the association between lateonset sepsis and the primary outcome.
Results
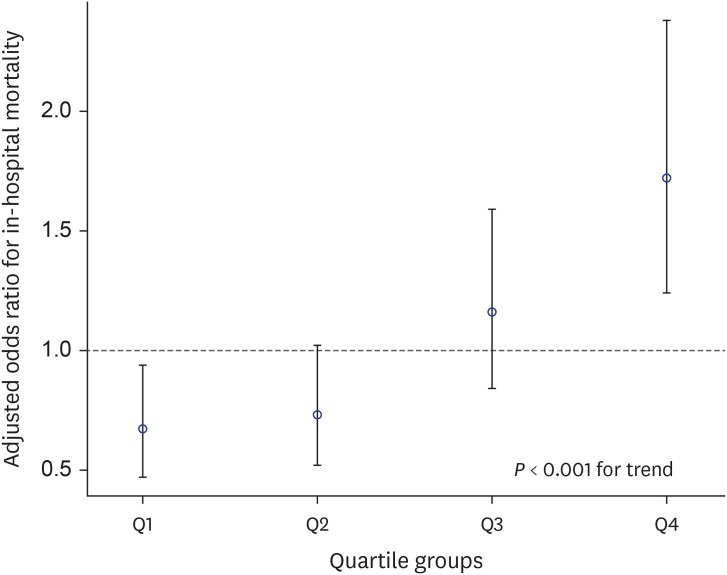
A total of 1,395 patients were included (median age, 68.0 years; women, 36.3%). The early- and late-onset sepsis groups comprised 668 (47.9%) and 727 (52.1%) patients. Propensity score-matched analysis showed an increased risk of in-hospital mortality in the late-onset group (adjusted odds ratio [aOR], 3.00; 95% confidence interval [CI], 1.69–5.34). The same trend was observed in the entire study population (aOR, 1.85; 95% CI, 1.37–2.50). When patients were divided into LOS quartile groups, an increasing trend of mortality risk was observed in the higher quartiles (Pfor trend < 0.001).
Conclusion
Extended LOS before developing sepsis is associated with higher in-hospital mortality. More careful management is required when sepsis occurs in patients hospitalized for ≥ 5 days.
Figure
Reference
-
1. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016; 315(8):801–810. PMID: 26903338.2. Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet. 2020; 395(10219):200–211. PMID: 31954465.3. Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021; 49(11):e1063–e1143. PMID: 34605781.4. Jarczak D, Kluge S, Nierhaus A. Sepsis-pathophysiology and therapeutic concepts. Front Med (Lausanne). 2021; 8:628302. PMID: 34055825.5. Bein T, Hackner K, Zou T, Schultes S, Bösch T, Schlitt HJ, et al. Socioeconomic status, severity of disease and level of family members’ care in adult surgical intensive care patients: the prospective ECSSTASI study. Intensive Care Med. 2012; 38(4):612–619. PMID: 22273749.6. Mudge AM, McRae P, Hubbard RE, Peel NM, Lim WK, Barnett AG, et al. Hospital-associated complications of older people: a proposed multicomponent outcome for acute care. J Am Geriatr Soc. 2019; 67(2):352–356. PMID: 30423197.7. Moore L, Cisse B, Batomen Kuimi BL, Stelfox HT, Turgeon AF, Lauzier F, et al. Impact of socio-economic status on hospital length of stay following injury: a multicenter cohort study. BMC Health Serv Res. 2015; 15(1):285. PMID: 26204932.8. White DB, Angus DC, Shields AM, Buddadhumaruk P, Pidro C, Paner C, et al. A randomized trial of a family-support intervention in intensive care units. N Engl J Med. 2018; 378(25):2365–2375. PMID: 29791247.9. Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010; 210(6):901–908. PMID: 20510798.10. Ibrahim H, Harhara T, Athar S, Nair SC, Kamour AM. Multi-disciplinary discharge coordination team to overcome discharge barriers and address the risk of delayed discharges. Risk Manag Healthc Policy. 2022; 15:141–149. PMID: 35140535.11. Mao F, Greysen SR. Quantifying the risks of hospitalization-is it really as safe as we believe? J Hosp Med. 2020; 15(1):62–63. PMID: 31869303.12. Valente da Silva HG, Santos SO, Silva NO, Ribeiro FD, Josua LL, Moreira AS. Nutritional assessment associated with length of inpatients’ hospital stay. Nutr Hosp. 2012; 27(2):542–547. PMID: 22732981.13. Ford N, Patten G, Rangaraj A, Davies MA, Meintjes G, Ellman T. Outcomes of people living with HIV after hospital discharge: a systematic review and meta-analysis. Lancet HIV. 2022; 9(3):e150–e159. PMID: 35245507.14. Philbin EF, Roerden JB. Longer hospital length of stay is not related to better clinical outcomes in congestive heart failure. Am J Manag Care. 1997; 3(9):1285–1291. PMID: 10178477.15. Jeon K, Na SJ, Oh DK, Park S, Choi EY, Kim SC, et al. Characteristics, management and clinical outcomes of patients with sepsis: a multicenter cohort study in Korea. Acute Crit Care. 2019; 34(3):179–191. PMID: 31723927.16. Park S, Jeon K, Oh DK, Choi EY, Seong GM, Heo J, et al. Normothermia in patients with sepsis who present to emergency departments is associated with low compliance with sepsis bundles and increased in-hospital mortality rate. Crit Care Med. 2020; 48(10):1462–1470. PMID: 32931189.17. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007; 147(8):573–577. PMID: 17938396.18. Chang BP. Can hospitalization be hazardous to your health? A nosocomial based stress model for hospitalization. Gen Hosp Psychiatry. 2019; 60:83–89. PMID: 31376645.19. Schimmel EM. The hazards of hospitalization. Ann Intern Med. 1964; 60(1):100–110. PMID: 14106730.20. Pronovost PJ, Watson SR, Goeschel CA, Hyzy RC, Berenholtz SM. Sustaining reductions in central line-associated bloodstream infections in michigan intensive care units: a 10-year analysis. Am J Med Qual. 2016; 31(3):197–202. PMID: 25609646.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative norepinephrine versus dopamine in patients undergoing noncardiac surgery: a propensity-matched analysis using a nationwide intensive care database
- Prognostic Factors of Neonatal Sepsis Mortality in Developing Country
- Effects of Emergency Department Length of Stay on Prognosis for Critically Ill Patients Undergoing Traumatic Emergency Surgery
- The Role of Whole-Body Computed Tomography in Severely Injured Patients Retrospective Single Center Cohort Study
- Impact of the Timing of Percutaneous Nephrostomy on the Prognosis of Obstructive Urolithiasis With Sepsis: A Retrospective Cohort Study