J Surg Ultrasound.
2023 Nov;10(2):52-57. 10.46268/jsu.2023.10.2.52.
Treatment of Leg Ulcers Accompanied by Chronic Venous Insufficiency and Lymphedema Caused by IgG4-Related Disease
- Affiliations
-
- 1Department of Surgery, Jeonbuk National University Medical School and Hospital, Jeonju, Korea
- KMID: 2553146
- DOI: http://doi.org/10.46268/jsu.2023.10.2.52
Abstract
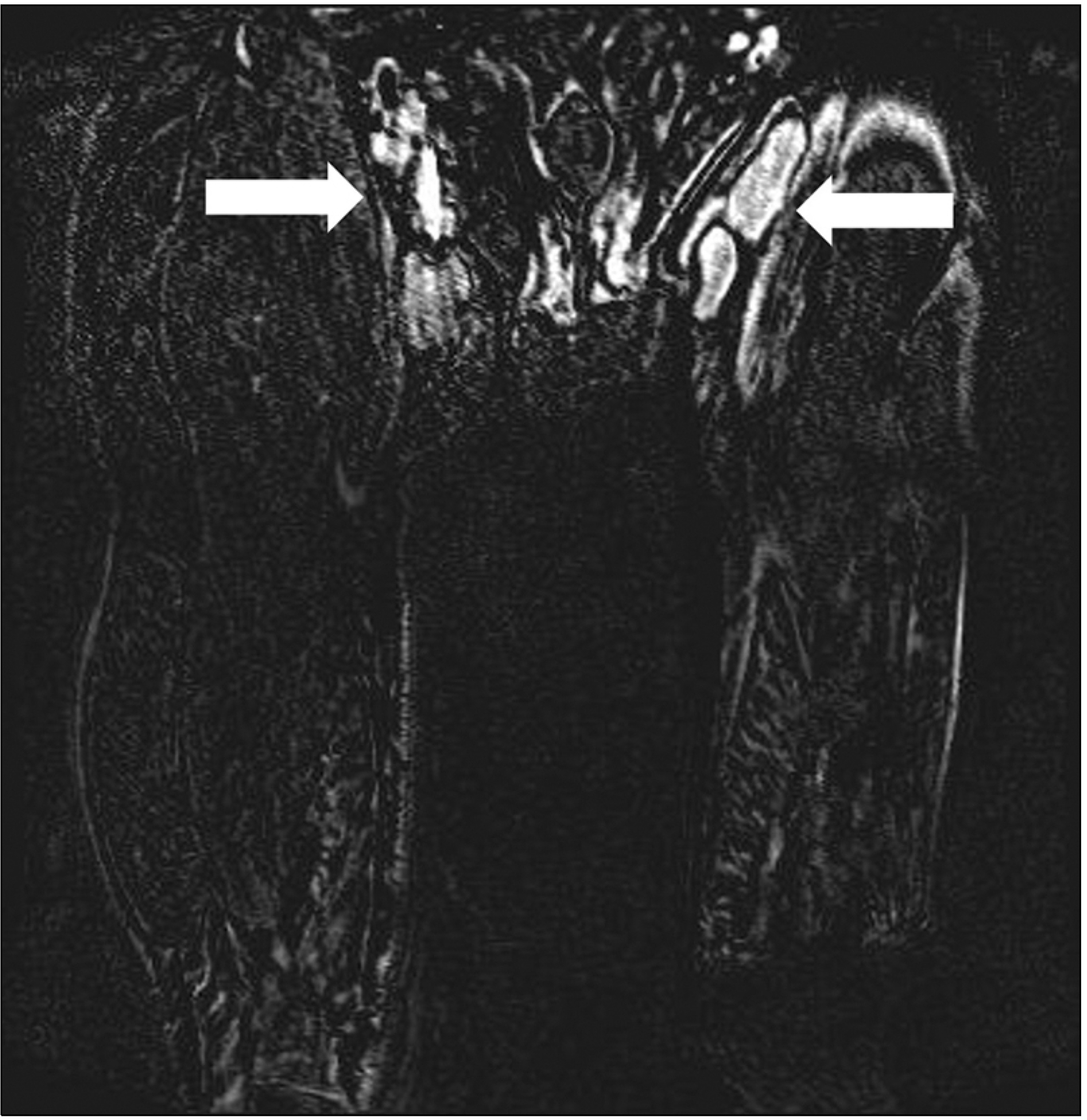
- IgG4-related disease is a multi-organ immune-medicated condition that mimics malignancies, infections, and inflammatory disorders. This report presents the case of a 62-year-old man with a history of repeated cellulitis and ulcers on his lower extremities who was diagnosed incidentally with IgG4-related disease during treatment. The patient’s unhealed ulcer was initially treated by debridement and aseptic dressing several times, but the wounds showed no improvement. Lower extremity venous ultrasound revealed unusually enlarged LN around the great saphenous vein (GSV) near the inguinal area and severe varicosity in both truncal veins. Lymphoscintigraphy was performed according to the ultrasound results, which showed secondary lymphedema in both legs. IgG4-released disease was diagnosed in an excisional biopsy of the lymph node near the great saphenous vein during stripping and ligation of the truncal vein. After continuous wound debridement and the administration of steroids and immunosuppressants, the patient's leg ulcer improved after approximately three months.
Figure
Reference
-
1. Mahajan VS, Mattoo H, Deshpande V, Pillai SS, Stone JH. 2014; IgG4-related disease. Annu Rev Pathol. 9:315–47. DOI: 10.1146/annurev-pathol-012513-104708. PMID: 24111912.
Article2. Umehara H, Okazaki K, Masaki Y, Kawano M, Yamamoto M, Saeki T, et al. 2012; A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol. 22:1–14. DOI: 10.3109/s10165-011-0508-6. PMID: 21881964.
Article3. Stone JH, Khosroshahi A, Deshpande V, Chan JK, Heathcote JG, Aalberse R, et al. 2012; Recommendations for the nomenclature of IgG4-related disease and its individual organ system manifestations. Arthritis Rheum. 64:3061–7. DOI: 10.1002/art.34593. PMID: 22736240. PMCID: PMC5963880.
Article4. Kamisawa T, Zen Y, Pillai S, Stone JH. 2015; IgG4-related disease. Lancet. 385:1460–71. DOI: 10.1016/S0140-6736(14)60720-0. PMID: 25481618.
Article5. Akiyama M, Kaneko Y, Takeuchi T. 2019; Characteristics and prognosis of IgG4-related periaortitis/periarteritis: a systematic literature review. Autoimmun Rev. 18:102354. DOI: 10.1016/j.autrev.2019.102354. PMID: 31323364.
Article6. Zen Y, Nakanuma Y. 2011; Pathogenesis of IgG4-related disease. Curr Opin Rheumatol. 23:114–8. DOI: 10.1097/BOR.0b013e3283412f4a. PMID: 21045701.
Article7. Stone JH, Zen Y, Deshpande V. 2012; IgG4-related disease. N Engl J Med. 366:539–51. DOI: 10.1056/NEJMra1104650. PMID: 22316447.
Article8. Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. 2003; A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 38:982–4. DOI: 10.1007/s00535-003-1175-y. PMID: 14614606.
Article9. Deshpande V, Gupta R, Sainani N, Sahani DV, Virk R, Ferrone C, et al. 2011; Subclassification of autoimmune pancreatitis: a histologic classification with clinical significance. Am J Surg Pathol. 35:26–35. DOI: 10.1097/PAS.0b013e3182027717. PMID: 21164284.10. Stone JH, Khosroshahi A, Hilgenberg A, Spooner A, Issel-bacher EM, Stone JR. 2009; IgG4-related systemic disease and lymphoplasmacytic aortitis. Arthritis Rheum. 60:3139–45. DOI: 10.1002/art.24798. PMID: 19790067.
Article11. Dahlgren M, Khosroshahi A, Nielsen GP, Deshpande V, Stone JH. 2010; Riedel's thyroiditis and multifocal fibrosclerosis are part of the IgG4-related systemic disease spectrum. Arthritis Care Res (Hoboken). 62:1312–8. DOI: 10.1002/acr.20215. PMID: 20506114.
Article12. Saeki T, Saito A, Hiura T, Yamazaki H, Emura I, Ueno M, et al. 2006; Lymphoplasmacytic infiltration of multiple organs with immunoreactivity for IgG4: IgG4-related systemic disease. Intern Med. 45:163–7. DOI: 10.2169/internalmedicine.45.1431. PMID: 16508232.
Article13. Smith B, Carroll MB. 2012; Persistent lymphadenopathy due to IgG4- re-l-a-ted disease. Case Reports Immunol. 2012:158208. DOI: 10.1155/2012/158208. PMID: 25383229. PMCID: PMC4207595.14. Kamisawa T, Shimosegawa T, Okazaki K, Nishino T, Wata-nabe H, Kanno A, et al. 2009; Standard steroid treatment for autoimmune pancreatitis. Gut. 58:1504–7. DOI: 10.1136/gut.2008.172908. PMID: 19398440.
Article15. Kamisawa T, Okazaki K, Kawa S, Shimosegawa T, Tanaka M. Research Committee for Intractable Pancreatic Disease and Japan Pancreas Society. 2010; Japanese consensus guidelines for management of autoimmune pancreatitis: III. Treatment and prognosis of AIP. J Gastroenterol. 45:471–7. DOI: 10.1007/s00535-010-0221-9. PMID: 20213336.
Article16. Hart PA, Kamisawa T, Brugge WR, Chung JB, Culver EL, Czakó L, et al. 2013; Long-term outcomes of autoimmune pancreatitis: a multicentre, international analysis. Gut. 62:1771–6. DOI: 10.1136/gutjnl-2012-303617. PMID: 23232048. PMCID: PMC3862979.
Article17. Kamisawa T, Egawa N, Inokuma S, Tsuruta K, Okamoto A, Kamata N, et al. 2003; Pancreatic endocrine and exocrine function and salivary gland function in autoimmune pancreatitis before and after steroid therapy. Pancreas. 27:235–8. DOI: 10.1097/00006676-200310000-00007. PMID: 14508128.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Leg Ulcers Accompanied by Chronic Venous Insufficiency and Lymphedema Caused by IgG4-Related Disease
- Unilateral Leg Swelling Caused by a Ganglion Cyst on the Hip Joint
- Venous Leg Ulcer in a Sarcoidosis Patient: A Case Report
- Optimal Diagnosis and Therapy of Venous Ulcer
- Pseudo-Kaposi's Sarcoma Developing After Surgery on a Lower Limb Fracture