J Korean Neurosurg Soc.
2024 Mar;67(2):166-176. 10.3340/jkns.2023.0035.
The Effect of Preoperative Three Dimensional Modeling and Simulation on Outcome of Intracranial Aneursym Surgery
- Affiliations
-
- 1Department of Neurosurgery, Ege University School of Medicine, Izmir, Turkey
- 2Department of Biomechanics, Dokuz Eylül University Health Science Institution, Izmir, Turkey
- 3Department of Radiology, Ege University School of Medicine, Izmir, Turkey
- 4Department of Neurosurgery, Dokuz Eylül University School of Medicine, Izmir, Turkey
- KMID: 2553122
- DOI: http://doi.org/10.3340/jkns.2023.0035
Abstract
Objective
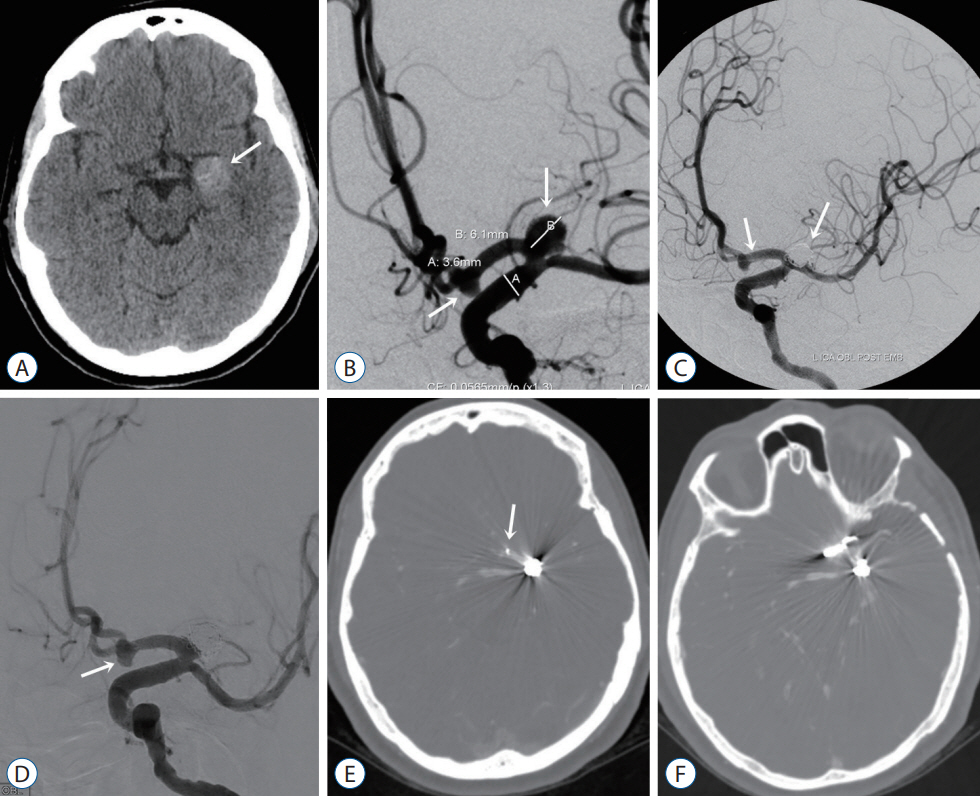
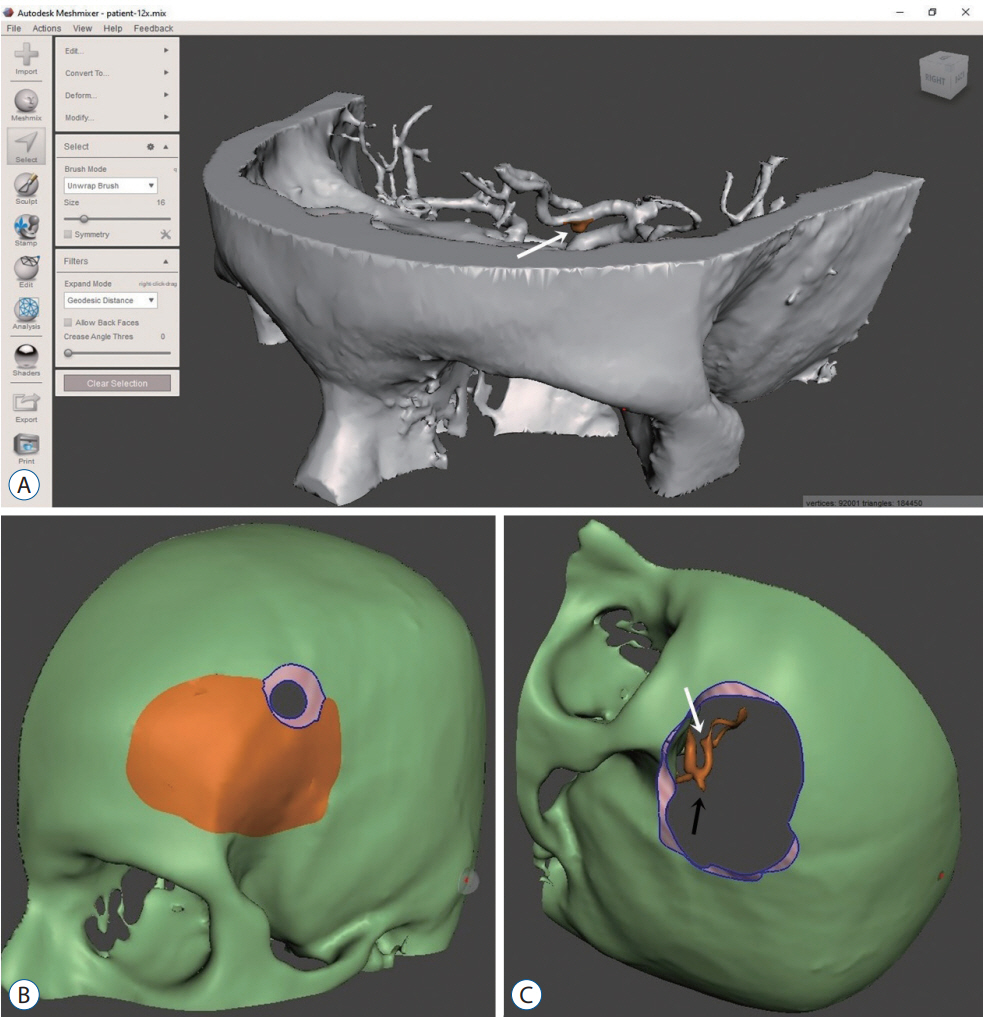
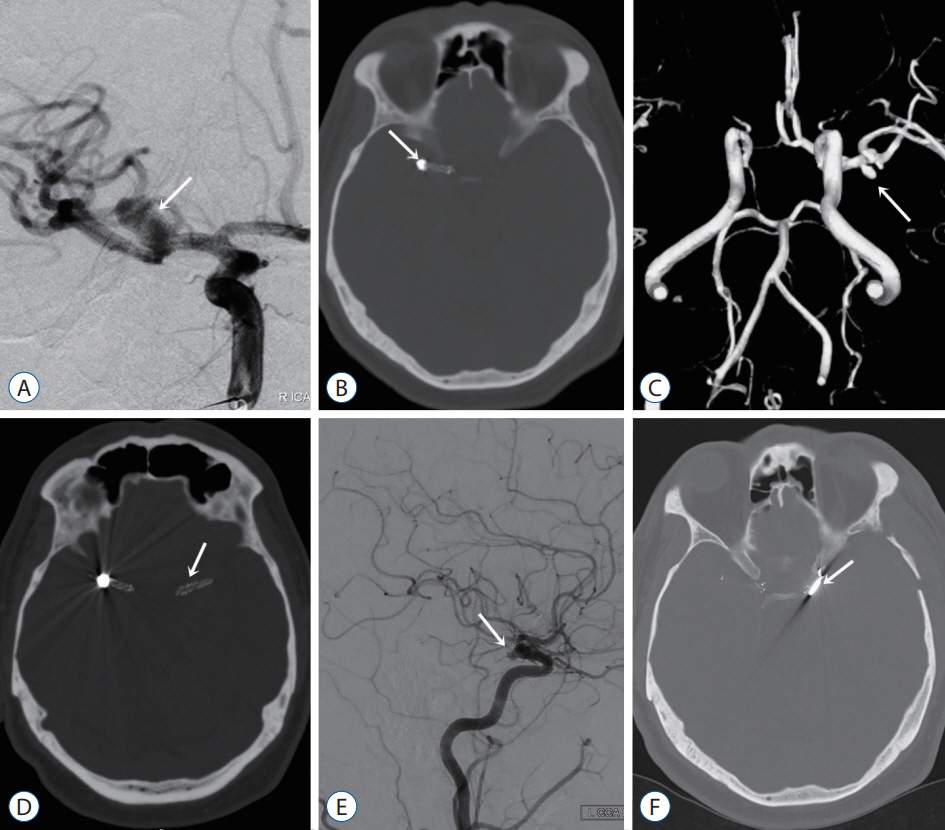
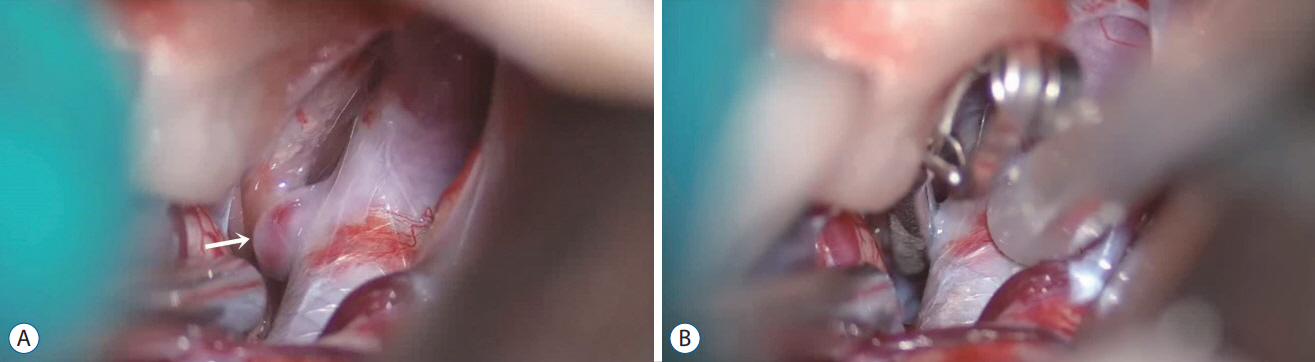
: Three-dimensional (3D) printing in vascular surgery is trending and is useful for the visualisation of intracranial aneurysms for both surgeons and trainees. The 3D models give the surgeon time to practice before hand and plan the surgery accordingly. The aim of this study was to examine the effect of preoperative planning with 3D printing models of aneurysms in terms of surgical time and patient outcomes.
Methods
: Forty patients were prospectively enrolled in this study and divided into two groups : groups I and II. In group I, only the angiograms were studied before surgery. Solid 3D modelling was performed only for group II before the operation and was studied accordingly. All surgeries were performed by the same senior vascular neurosurgeon. Demographic data, surgical data, both preoperative and postoperative modified Rankin scale (mRS) scores, and Glasgow outcome scores (GOS) were evaluated.
Results
: The average time of surgery was shorter in group II, and the difference was statistically significant between the two groups (p<0.001). However, no major differences were found for the GOS, hospitalisation time, or mRS.
Conclusion
: This study is the first prospective study of the utility of 3D aneurysm models. We show that 3D models are useful in surgery preparation. In the near future, these models will be used widely to educate trainees and pre-plan surgical options for senior surgeons.
Keyword
Figure
Reference
-
References
1. Bakker NA, Metzemaekers JD, Groen RJ, Mooij JJ, Van Dijk JM. International Subarachnoid Aneurysm Trial 2009: endovascular coiling of ruptured intracranial aneurysms has no significant advantage over neurosurgical clipping. Neurosurgery. 66:961–962. 2010.2. Cavallo C, Safavi-Abbasi S, Kalani MYS, Gandhi S, Sun H, Oppenlander ME, et al. Pulmonary complications after spontaneous aneurysmal subarachnoid hemorrhage: experience from barrow neurological institute. World Neurosurg. 119:e366–e373. 2018.3. Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 43:1711–1737. 2012.4. Fotakopoulos G, Tsianaka E, Fountas K, Makris D, Spyrou M, Hernesniemi J. Clipping versus coiling in anterior circulation ruptured intracranial aneurysms: a meta-analysis. World Neurosurg. 104:482–488. 2017.5. Hernesniemi J, Ishii K, Niemelä M, Kivipelto L, Fujiki M, Shen H. Subtemporal approach to basilar bifurcation aneurysms: advanced technique and clinical experience. Acta Neurochir Suppl. 94:31–38. 2005.6. Hernesniemi J, Koivisto T. Comments on “The impact of the International Subarachnoid Aneurysm Treatment Trial (ISAT) on neurosurgical practice”. Acta Neurochir (Wien). 146:203–208. 2004.7. Hernesniemi J, Niemelä M. Clipping of a ruptured aneurysm with clot removal in one session: still gold standard of treatment. World Neurosurg. 74:579–580. 2010.8. Jabbarli R, Wrede KH, Pierscianek D, Dammann P, El Hindy N, Özkan N, et al. Outcome after clipping of unruptured intracranial aneurysms depends on caseload. World Neurosurg. 89:666–671.e1. 2016.9. Kimura T, Morita A, Nishimura K, Aiyama H, Itoh H, Fukaya S, et al. Simulation of and training for cerebral aneurysm clipping with 3-dimensional models. Neurosurgery. 65:719–726. discussion 725-726. 2009.10. Lehecka M, Dashti R, Lehto H, Kivisaari R, Niemelä M, Hernesniemi J. Distal anterior cerebral artery aneurysms. Acta Neurochir Suppl. 107:15–26. 2010.11. Mashiko T, Kaneko N, Konno T, Otani K, Nagayama R, Watanabe E. Training in cerebral aneurysm clipping using self-made 3-dimensional models. J Surg Educ. 74:681–689. 2017.12. Mashiko T, Otani K, Kawano R, Konno T, Kaneko N, Ito Y, et al. Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping. World Neurosurg. 83:351–361. 2015.13. Molyneux AJ, Birks J, Clarke A, Sneade M, Kerr RS. The durability of endovascular coiling versus neurosurgical clipping of ruptured cerebral aneurysms: 18 year follow-up of the UK cohort of the international subarachnoid aneurysm trial (ISAT). Lancet. 385:691–697. 2015.14. Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 366:809–817. 2005.15. Nanda A, Patra DP, Bir SC, Maiti TK, Kalakoti P, Bollam P. Microsurgical clipping of unruptured ıntracranial aneurysms: a single surgeon’s experience over 16 years. World Neurosurg. 100:85–99. 2017.16. Park SE, Park EK, Shim KW, Kim DS. Modified cranioplasty technique using 3-dimensional printed ımplants in preventing temporalis muscle hollowing. World Neurosurg. 126:e1160–e1168. 2019.17. Ploch CC, Mansi CSSA, Jayamohan J, Kuhl E. Using 3D printing to create personalized brain models for neurosurgical training and preoperative planning. World Neurosurg. 90:668–674. 2016.18. Ryan JR, Almefty KK, Nakaji P, Frakes DH. Cerebral aneurysm clipping surgery simulation using patient-specific 3D printing and silicone casting. World Neurosurg. 88:175–181. 2016.19. Song J, Kim BS, Shin YS. Treatment outcomes of unruptured intracranial aneurysm; experience of 1,231 consecutive aneurysms. Acta Neurochir (Wien). 157:1303–1311. 2015.20. Spetzler RF, McDougall CG, Zabramski JM, Albuquerque FC, Hills NK, Nakaji P, et al. Ten-year analysis of saccular aneurysms in the Barrow Ruptured Aneurysm Trial. J Neurosurg. 132:771–776. 2019.21. Spetzler RF, Zabramski JM, McDougall CG, Albuquerque FC, Hills NK, Wallace RC, et al. Analysis of saccular aneurysms in the Barrow Ruptured Aneurysm Trial. J Neurosurg. 128:120–125. 2018.22. Steiner T, Juvela S, Unterberg A, Jung C, Forsting M, Rinkel G, et al. European Stroke Organization guidelines for the management of intracranial aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 35:93–112. 2013.23. Tulamo R, Frösen J, Hernesniemi J, Niemelä M. Inflammatory changes in the aneurysm wall: a review. J Neurointerv Surg. 10(Suppl 1):i58–i67. 2018.24. Wang L, Ye X, Hao Q, Chen Y, Chen X, Wang H, et al. Comparison of two three-dimensional printed models of complex intracranial aneurysms for surgical simulation. World Neurosurg. 103:671–679. 2017.25. Wang L, Ye X, Hao Q, Ma L, Chen X, Wang H, et al. Three-dimensional intracranial middle cerebral artery aneurysm models for aneurysm surgery and training. J Clin Neurosci. 50:77–82. 2018.26. Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 362:103–110. 2003.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral intraoral vertical ramus osteotomy based on preoperative three-dimensional simulation surgery in a patient with facial asymmetry
- Virtual Preoperative Simulation for Excision of Spinal Tumors: Surgeon Processing of Medical Computer-Assisted Design Software
- 3-Dimensional Model Simulation Craniomaxillofacial Surgery using Rapid Prototyping Technique
- Obtaining Informed Consent Using Patient Specific 3D Printing Cerebral Aneurysm Model
- Corrective Surgery Using Virtual Surgical Simulation and a Three-Dimensional Printed Osteotomy Guide: A Case Report