Clin Exp Otorhinolaryngol.
2024 Feb;17(1):37-45. 10.21053/ceo.2023.00010.
Changes in Revision Cochlear Implantation and Device Failure Profiles
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Hearing Research Laboratory, Samsung Medical Center, Seoul, Korea
- KMID: 2553054
- DOI: http://doi.org/10.21053/ceo.2023.00010
Abstract
Objectives
. As cochlear implantation (CI) experiences rapid innovations and its indications expand, the characteristics of revision CI (RCI) are evolving. This study investigated changes in the RCI profile and explored their clinical implications.
Methods
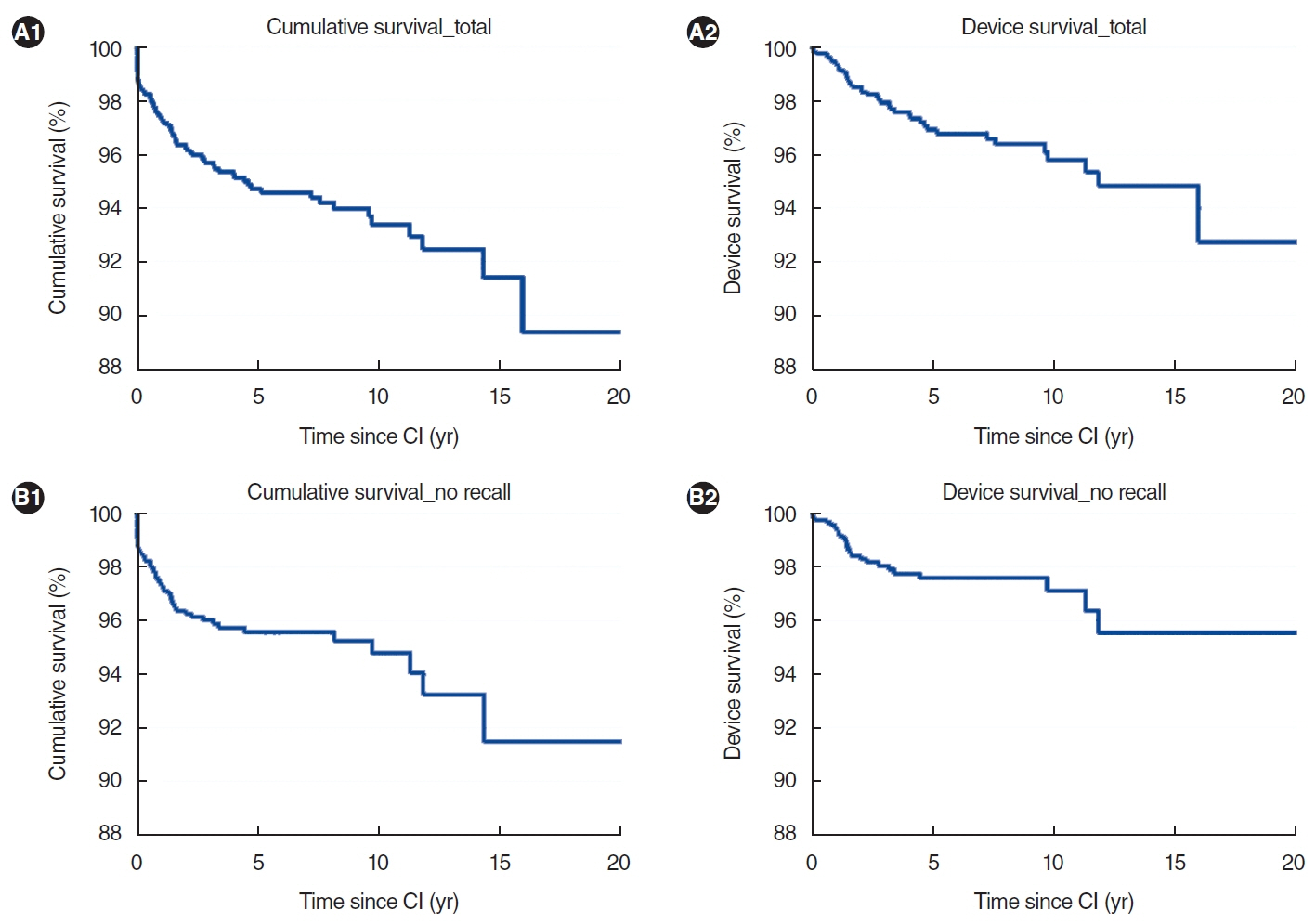
. A retrospective chart review was conducted of all CIs performed at a tertiary medical institution between October 2001 and January 2023. The rates of and reasons for RCI were evaluated in relation to the manufacturer and device model. Kaplan-Meier analysis was employed to examine cumulative and device survival curves. Cumulative and device survival rates were additionally analyzed based on age group, period of primary CI, and manufacturer. A Cox proportional hazards model was employed to evaluate the association between RCI and the device manufacturer.
Results
. Among 1,430 CIs, 73 (5.1%) required RCI. The predominant reason for RCI was device failure (40 of 73 RCIs [54.8%]), with an overall device failure rate of 2.8%. This was followed by flap-associated problems and migration (nine of 73 RCIs each [12.3%]). Flap retention issues emerged as a new cause in three cases (two involving the CI 632 and one involving the SYNCHRONY 2 implant), and six instances of electrode tip fold-over arose (four for the CI 600 series and two for the CI 500 series). The overall 10-year cumulative and device survival rates were 93.4% and 95.8%, respectively. After excluding models with recall issues, significant differences in cumulative (P =0.010) and device (P =0.001) survival rates were observed across manufacturers.
Conclusion
. While the overall CI survival rate is stable, device failure persists as the predominant reason for RCI. Moreover, the types of complications leading to revision (including issues with flap retention and electrode tip fold-over) have shifted, particularly for newer implant models. Given the clinical importance of device failure and subsequent reoperation, clinicians should remain informed about and responsive to these trends.
Figure
Reference
-
1. Dettman SJ, Dowell RC, Choo D, Arnott W, Abrahams Y, Davis A, et al. Long-term communication outcomes for children receiving cochlear implants younger than 12 months: a multicenter study. Otol Neurotol. 2016; Feb. 37(2):e82–95.2. Naik AN, Varadarajan VV, Malhotra PS. Early pediatric cochlear implantation: an update. Laryngoscope Investig Otolaryngol. 2021; Jun. 6(3):512–21.3. Fakurnejad S, Vail D, Song Y, Alyono J, Blevins NH. Trends in age of cochlear implant recipients, and the impact on perioperative complication rates. Otol Neurotol. 2020; Apr. 41(4):438–43.4. Bourn SS, Goldstein MR, Morris SA, Jacob A. Cochlear implant outcomes in the very elderly. Am J Otolaryngol. 2022; 43(1):103200.5. Wichova H, Mills D, Beatty S, Peng K, Miller M. Cochlear implantation performance outcomes in patients over 80 years old. Laryngoscope Investig Otolaryngol. 2022; Jun. 7(3):847–53.6. Kim SY, Kim MB, Chung WH, Cho YS, Hong SH, Moon IJ. Evaluating reasons for revision surgery and device failure rates in patients who underwent cochlear implantation surgery. JAMA Otolaryngol Head Neck Surg. 2020; May. 146(5):414–20.7. Kimura KS, O’Connell BP, Nassiri AM, Dedmon MM, Haynes DS, Bennett ML. Outcomes of revision cochlear implantation. Otol Neurotol. 2020; Jul. 41(6):e705–11.8. Lane C, Zimmerman K, Agrawal S, Parnes L. Cochlear implant failures and reimplantation: a 30-year analysis and literature review. Laryngoscope. 2020; Mar. 130(3):782–9.9. Gumus B, Incesulu AS, Kaya E, Kezban Gurbuz M, Ozgur Pinarbasli M. Analysis of cochlear implant revision surgeries. Eur Arch Otorhinolaryngol. 2021; Mar. 278(3):675–82.10. Layfield E, Hwa TP, Naples J, Maina I, Brant JA, Eliades SJ, et al. Failure and revision surgery after cochlear implantation in the adult population: a 10-year single-institution retrospective and systematic review of the literature. Otol Neurotol. 2021; Mar. 42(3):408–13.11. Rayamajhi P, Kurkure R, Castellino A, Kumar S, Ha M, Nandhan R, et al. A clinical profile of revision cochlear implant surgery: MERF experience. Cochlear Implants Int. 2021; Mar. 22(2):61–7.12. Sagiv D, Yaar-Soffer Y, Yakir Z, Henkin Y, Shapira Y. Rates, indications, and speech perception outcomes of revision cochlear implantations. J Clin Med. 2021; Jul. 10(15):3215.13. Chen J, Chen B, Shi Y, Li Y. A retrospective review of cochlear implant revision surgery: a 24-year experience in China. Eur Arch Otorhinolaryngol. 2022; Mar. 279(3):1211–20.14. Karamert R, Duzlu M, Tutar H, Eravci FC, Turkcan AK, Zorlu ME, et al. Assessment of cochlear implant revision surgeries in a cohort of 802 patients. Otol Neurotol. 2019; Apr. 40(4):464–70.15. Rupp R, Balk M, Sievert M, Leibl V, Schleder S, Allner M, et al. Risk of magnetic resonance imaging-induced magnet dislocation for different types of cochlear implants: a single-center retrospective study. J Otolaryngol Head Neck Surg. 2023; Apr. 52(1):28.16. Posner D, Scott A, Polite C, Lustig LR. External magnet displacement in cochlear implants: causes and management. Otol Neurotol. 2010; Jan. 31(1):88–93.17. Ozturan O, Yenigun A, Senturk E, Calim OF, Aksoy F, Eren SB. Temporal scalp thickness, body mass index, and suprafascial placement of receiver coil of the cochlear implant. J Craniofac Surg. 2017; Nov. 28(8):e781–5.18. Kim YH, Cho SI. Skin flap necrosis by bone marking with methylene blue in cochlear implantation. J Audiol Otol. 2015; Sep. 19(2):108–10.19. Qin F, Li W, Qiu J, Zhang L, Zhong M. After cochlear implantation: complications related to flap around implants. J Otol. 2016; Dec. 11(4):198–201.20. Searle T, Marshall E, Craddock L, Monksfield P. Skin flap thickness and magnet strength in cochlear implants. Cochlear Implants Int. 2021; Mar. 22(2):80–4.21. Wagner L, Honig E, Frohlich L, Plontke S, Rahne T. Optimal retention force of audio processor magnets. Otol Neurotol. 2019; Jun. 40(5):e482–7.22. Jwair S, Prins A, Wegner I, Stokroos RJ, Versnel H, Thomeer HG. Scalar translocation comparison between lateral wall and perimodiolar cochlear implant arrays: a meta-analysis. Laryngoscope. 2021; Jun. 131(6):1358–68.23. Ishiyama A, Risi F, Boyd P. Potential insertion complications with cochlear implant electrodes. Cochlear Implants Int. 2020; Jul. 21(4):206–19.24. Ramos-Macias A, R De Miguel A, Falcon-Gonzalez JC. Mechanisms of electrode fold-over in cochlear implant surgery when using a flexible and slim perimodiolar electrode array. Acta Otolaryngol. 2017; Nov. 137(11):1129–35.25. Zuniga MG, Rivas A, Hedley-Williams A, Gifford RH, Dwyer R, Dawant BM, et al. Tip fold-over in cochlear implantation: case series. Otol Neurotol. 2017; Feb. 38(2):199–206.26. Hogerle C, Englhard A, Simon F, Gruninger I, Mlynski R, Hempel JM, et al. Cochlear implant electrode tip fold-over: our experience with long and flexible electrode. Otol Neurotol. 2022; Jan. 43(1):64–71.27. Gabrielpillai J, Burck I, Baumann U, Stover T, Helbig S. Incidence for tip foldover during cochlear implantation. Otol Neurotol. 2018; Oct. 39(9):1115–21.28. Kay-Rivest E, McMenomey SO, Jethanamest D, Shapiro WH, Friedmann DR, Waltzman SB, et al. Predictive value of transimpedance matrix measurements to detect electrode tip foldover. Otol Neurotol. 2022; Oct. 43(9):1027–32.29. Gomez Serrano M, Patel S, Harris R, Selvadurai D. Initial surgical and clinical experience with the Nucleus CI532 slim modiolar electrode in the UK. Cochlear Implants Int. 2019; Jul. 20(4):207–16.30. Mittmann P, Lauer G, Ernst A, Mutze S, Hassepass F, Arndt S, et al. Electrophysiological detection of electrode fold-over in perimodiolar cochlear implant electrode arrays: a multi-center study case series. Eur Arch Otorhinolaryngol. 2020; Jan. 277(1):31–5.31. Grolman W, Maat A, Verdam F, Simis Y, Carelsen B, Freling N, et al. Spread of excitation measurements for the detection of electrode array foldovers: a prospective study comparing 3-dimensional rotational x-ray and intraoperative spread of excitation measurements. Otol Neurotol. 2009; Jan. 30(1):27–33.32. Cosetti MK, Troob SH, Latzman JM, Shapiro WH, Roland JT, Waltzman SB. An evidence-based algorithm for intraoperative monitoring during cochlear implantation. Otol Neurotol. 2012; Feb. 33(2):169–76.33. Trakimas DR, Kozin ED, Ghanad I, Barber SR, Curtin H, Remenschneider AK. Precurved cochlear implants and tip foldover: a cadaveric imaging study. Otolaryngol Head Neck Surg. 2018; Feb. 158(2):343–9.