Neurointervention.
2024 Mar;19(1):45-51. 10.5469/neuroint.2023.00416.
Endovascular Treatment May Be Effective in Preventing Recurrence of Ischemic Stroke in Vertebral Artery Stump Syndrome: A Case Series
- Affiliations
-
- 1Department of Neurosurgery, Shinko Hospital, Kobe, Japan
- KMID: 2552879
- DOI: http://doi.org/10.5469/neuroint.2023.00416
Abstract
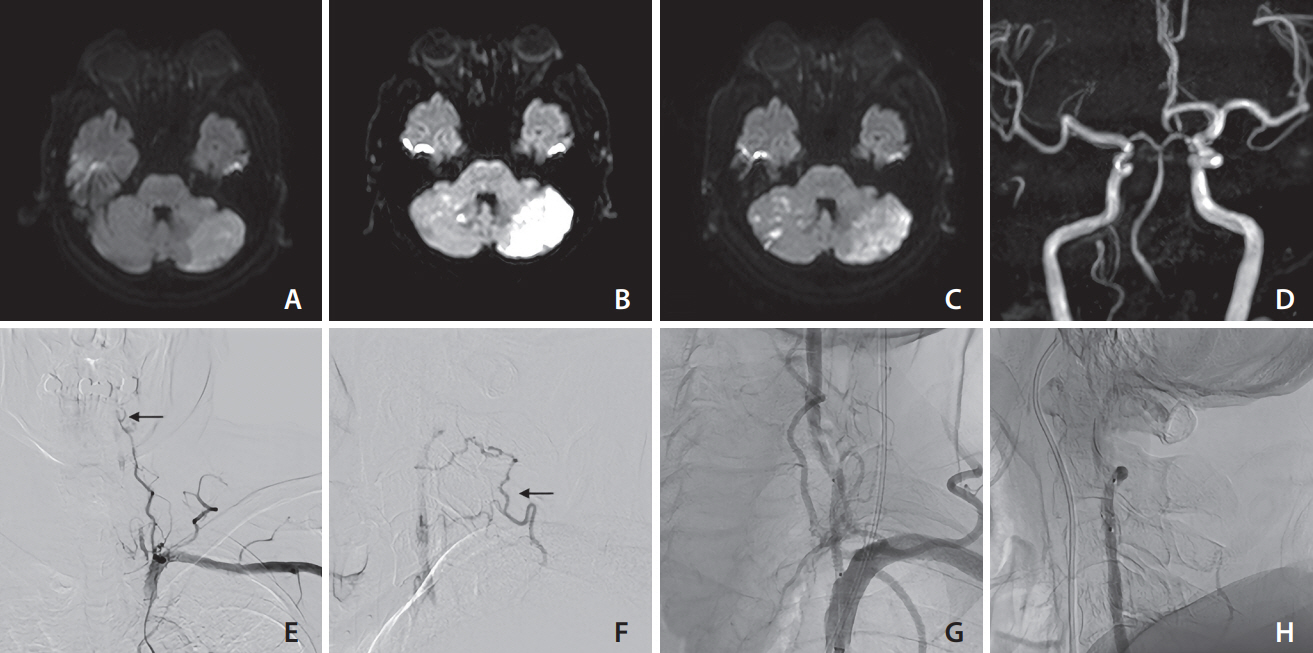
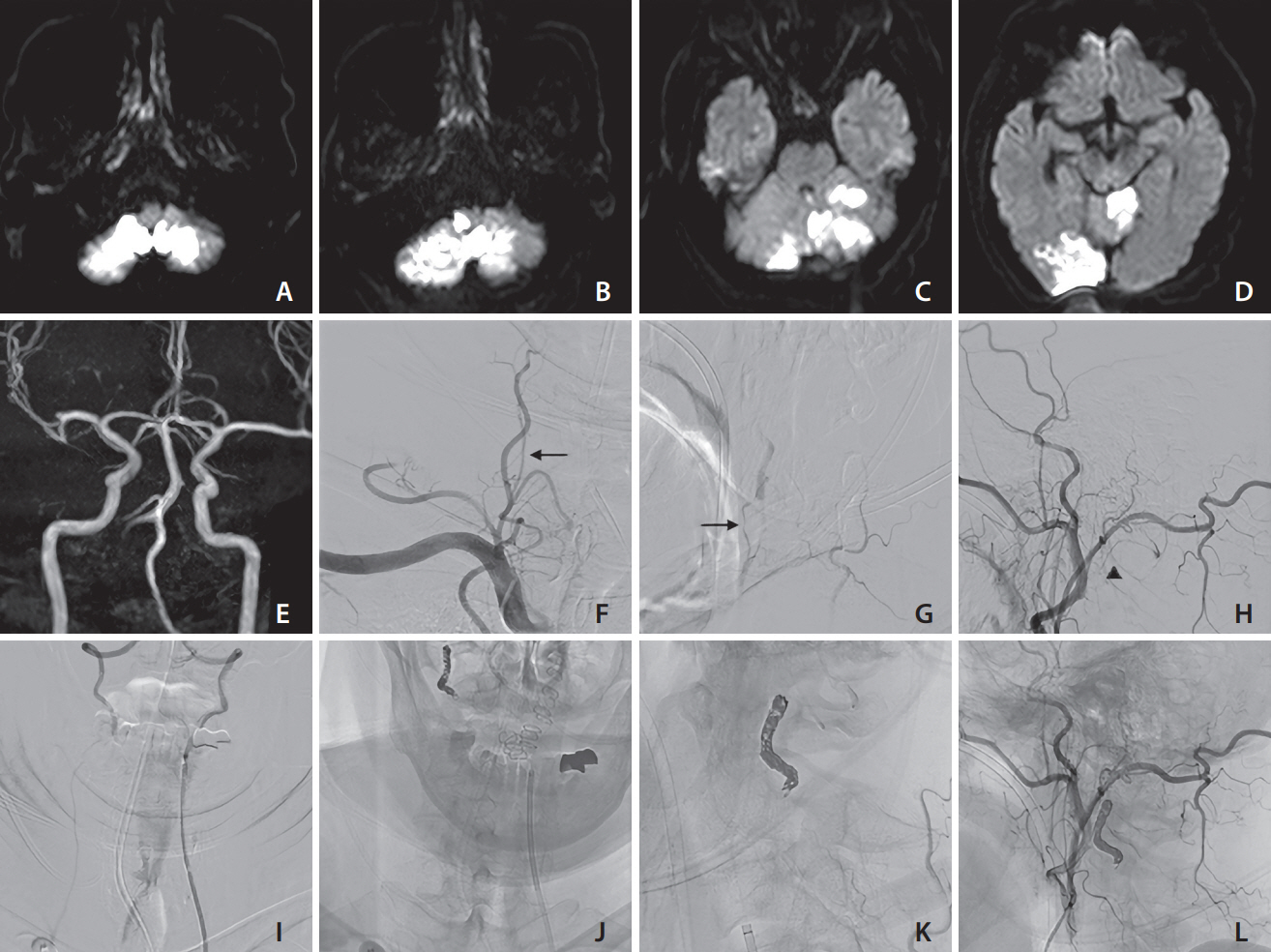
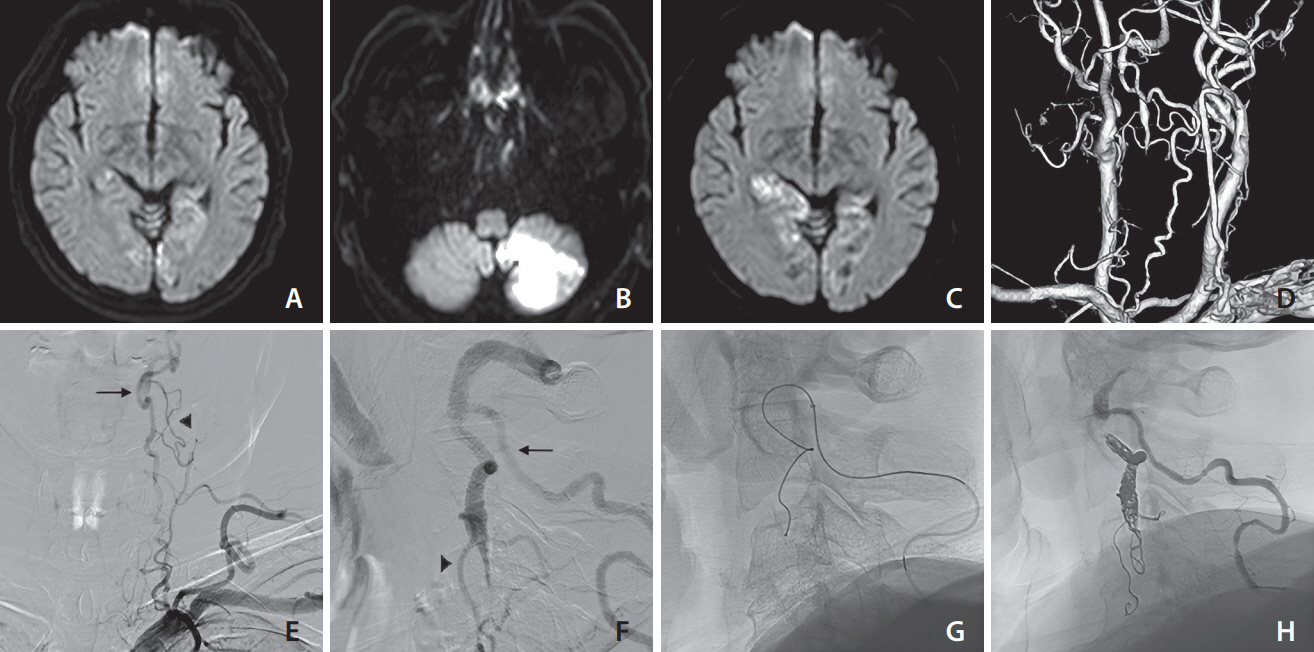
- Vertebral artery stump syndrome (VASS) is a rare condition that can cause posterior circulation ischemic stroke due to occlusion of the ipsilateral vertebral artery (VA) orifice, resulting in blood flow stagnation and embolus formation. Although there is no established treatment for this condition, we observed 3 cases of VASS out of 326 acute ischemic stroke cases at a single institution from April 2021 to October 2022. Despite the best possible antithrombotic treatment, all 3 patients had recurrent ischemic strokes. One patient underwent drug-eluting stenting of the VA orifice to relieve occlusive flow. The other 2 patients received coil embolization, which resulted in the disappearance of their culprit collateral flow. None of the patients had recurrent ischemic strokes after endovascular intervention. Based on our observations, stenting and coil embolization are effective methods for preventing future recurrences of VASS.
Figure
Reference
-
1. Kawano H, Inatomi Y, Hirano T, Yonehara T. Vertebral artery stump syndrome in acute ischemic stroke. J Neurol Sci. 2013; 324:74–79.
Article2. Yamano A, Nakai Y, Akutagawa K, Igarashi H, Tsukada K, Terakado T, et al. Fatal recurrent ischemic stroke caused by vertebral artery stump syndrome. Surg Neurol Int. 2021; 12:445.
Article3. Nguyen TN, Raymond J, Mahmoud M, Weill A, Roy D, Guilbert F. Vertebral artery stump syndrome. J Neurol Neurosurg Psychiatry. 2008; 79:91–92.
Article4. Ji R, Li B, Xu Z. Retrograde recanalisation for vertebral artery stump syndrome: a case report. Stroke Vasc Neurol. 2022; 7:462–464.
Article5. Okamoto A, Nakagawa I, Kotsugi M, Yokoyama S, Yamada S, Park YS, et al. Endovascular vertebral artery orifice angioplasty for the prevention of acute ischemic stroke following vertebral artery stump syndrome. Surg Neurol Int. 2022; 13:382.
Article6. Zhang W, Wang S, Li C, Wang Z, Yue F, Zhou J, et al. A case series and literature review of vertebral artery stump syndrome. Front Neurol. 2022; 12:770845.
Article7. Oda K, Noda M, Ishibashi T, Kogiku M, Abe K, Kishi H, et al. Percutaneous transluminal angioplasty for suspected vertebral artery stump syndrome. Neuroradiol J. 2020; 33:520–524.
Article8. Maeoka R, Nakagawa I, Ohnishi H, Kuga Y, Nakase H, Ohnishi H. A thread of hope for successful revascularization for acute embolic basilar artery occlusion due to miserable vertebral artery stump syndrome. A technical report. J Clin Neurosci. 2020; 73:299–303.
Article9. Katayama M, Endo H, Matsuda M, Kamiyama K, Osato T, Nakamura H. Vertebral artery stump syndrome: a 7-year follow-up case report. Radiol Case Rep. 2022; 17:2923–2926.
Article10. Tempaku A. Cerebral angiography directly visualizes to-and-fro stream of vertebral artery stump syndrome. J Gen Fam Med. 2017; 18:462–463.
Article11. Suzuki M, Dembo T, Hara W, Tajima T, Yamashita M, Oji S, et al. Vertebral artery stump syndrome. Intern Med. 2018; 57:733–736.
Article12. Markus HS, Larsson SC, Kuker W, Schulz UG, Ford I, Rothwell PM, VIST Investigators, et al. Stenting for symptomatic vertebral artery stenosis: the vertebral artery ischaemia stenting trial. Neurology. 2017; 89:1229–1236.
Article13. Li L, Wang X, Yang B, Wang Y, Gao P, Chen Y, et al. Validation and comparison of drug eluting stent to bare metal stent for restenosis rates following vertebral artery ostium stenting: a single-center real-world study. Interv Neuroradiol. 2020; 26:629–636.
Article14. Watanabe H, Domei T, Morimoto T, Natsuaki M, Shiomi H, Toyota T, STOPDAPT-2 Investigators, et al. Effect of 1-month dual antiplatelet therapy followed by clopidogrel vs 12-month dual antiplatelet therapy on cardiovascular and bleeding events in patients receiving PCI: the STOPDAPT-2 randomized clinical trial. JAMA. 2019; 321:2414–2427.15. Sorteberg A, Bakke SJ, Boysen M, Sorteberg W. Angiographic balloon test occlusion and therapeutic sacrifice of major arteries to the brain. Neurosurgery. 2008; 63:651–660. dicussion 660-661.
Article16. Zoarski GH, Seth R. Safety of unilateral endovascular occlusion of the cervical segment of the vertebral artery without antecedent balloon test occlusion. AJNR Am J Neuroradiol. 2014; 35:856–861.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rescue Endovascular Treatment to Prevent Neurological Deterioration in Acute Symptomatic Bilateral Vertebral Artery Occlusion
- Locked-in Syndrome Performed Endovascular Treatment for Vertebral Artery Dissection and Basilar Artery Occlusion Caused by a Golf Swing
- Simultaneous Onset of Ischemic and Hemorrhagic Stroke Due To Intracranial Artery Dissection
- Spontaneous Thrombolysis of Multiple Thrombi at Distal Region of Hypoplastic Vertebral Artery After Stent-assisted Angioplasty on Vertebral Artery Origin Stenosis: Angiographic Follow-up
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom