Neurointervention.
2023 Nov;18(3):182-189. 10.5469/neuroint.2023.00381.
Rescue Endovascular Treatment to Prevent Neurological Deterioration in Acute Symptomatic Bilateral Vertebral Artery Occlusion
- Affiliations
-
- 1Department of Neurology, School of Medicine, Chosun University, Gwangju, Korea
- 2Department of Neurosurgery, School of Medicine, Chosun University, Gwangju, Korea
- KMID: 2547280
- DOI: http://doi.org/10.5469/neuroint.2023.00381
Abstract
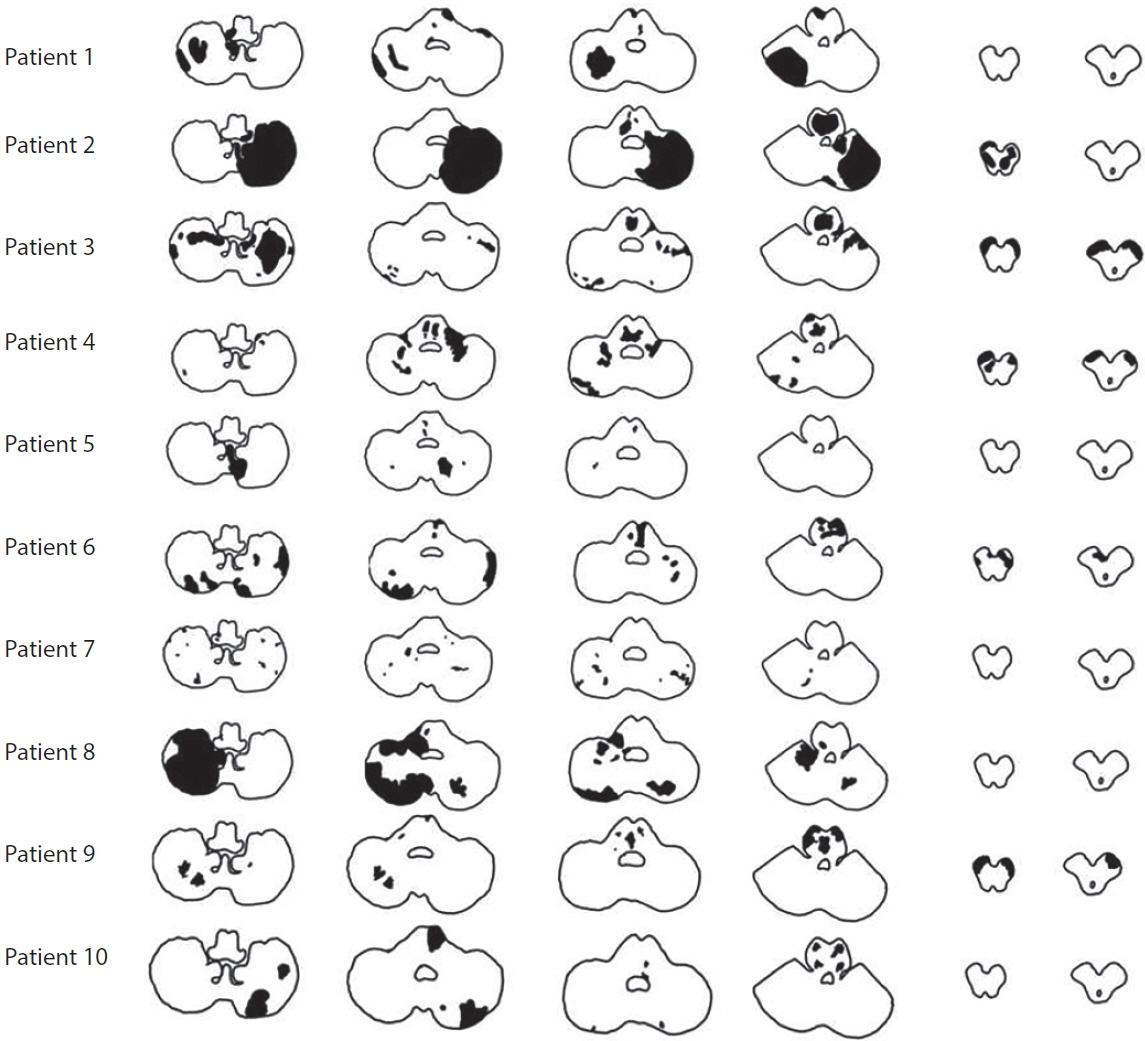
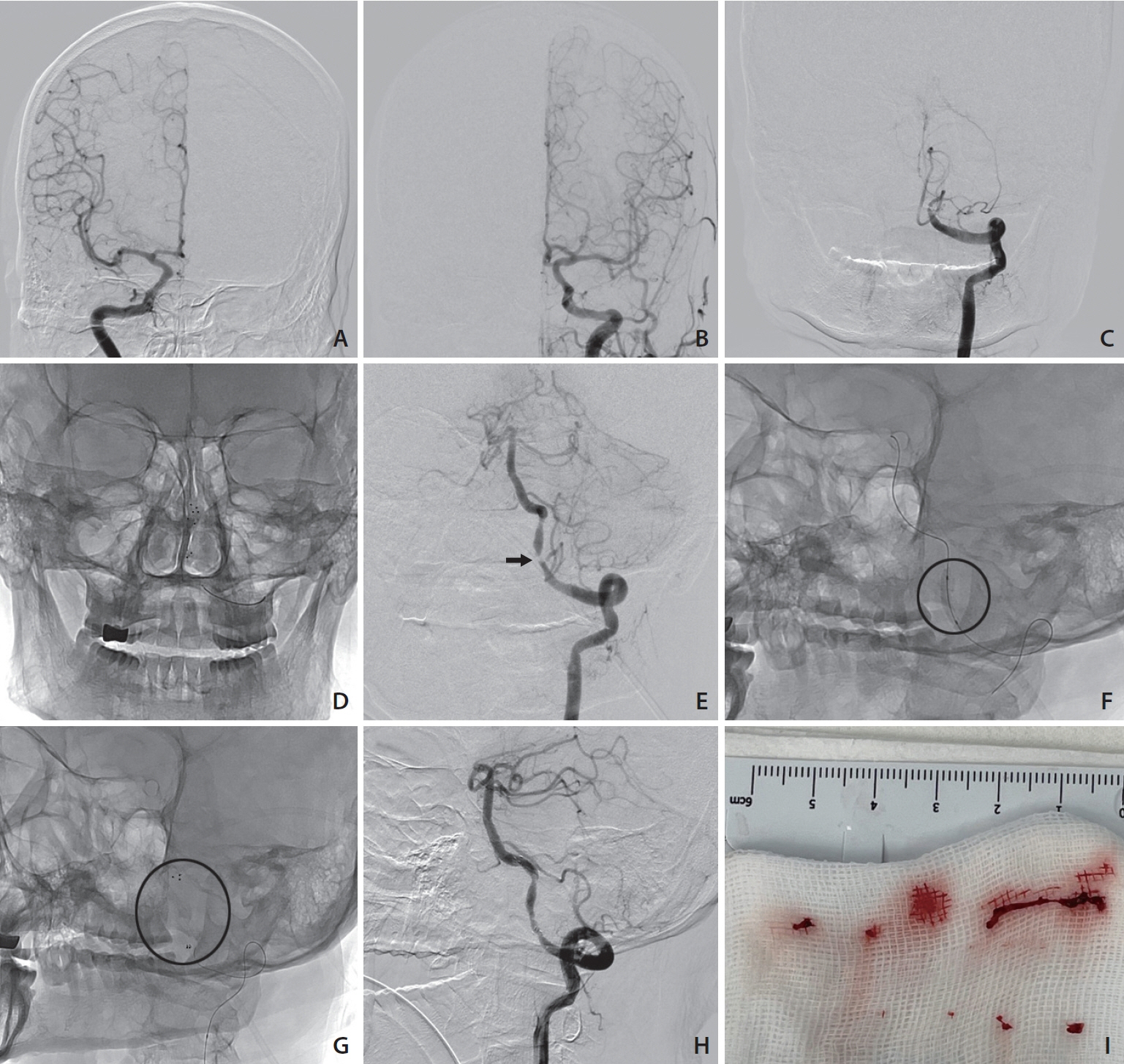
- Bilateral vertebral artery occlusive disease has been considered as a favorable condition with good collaterals. However, the prognosis of acute ischemic stroke secondary to symptomatic bilateral vertebral artery occlusion (BVAO) and endovascular treatment (EVT) has rarely been reported. We retrospectively selected patients with acute ischemic stroke admitted for symptomatic BVAO between January 2020 and February 2023. All patients with ischemic stroke were evaluated for ischemic lesion and arterial status using brain imaging and angiography. The prognosis of acute stroke with symptomatic BVAO was compared between EVT and conventional treatment. Outcomes were evaluated using modified Rankin Scale (mRS) score at 3 months follow-up. Within the study period, 17 of 2,655 acute ischemic stroke patients were diagnosed with ischemic stroke with symptomatic BVAO. The median age of these patients was 70 (interquartile range 44–89) years, and 13 (76%) were male. Seven patients received emergent EVT with stenting and 10 patients received conventional medical treatment only. Nine of 10 patients with conventional treatment had in-hospital stroke progression and developed new ischemic lesions in the pons and midbrain. Five patients with fetal and hypoplastic posterior communicating artery presented bilateral cerebral peduncular lesions. At 3 months follow-up, 6 patients (35%) had favorable outcomes (mRS 0–2), of which 5 were treated with vertebral artery stenting and 1 received conventional treatment. Ischemic stroke in patients with acute symptomatic BVAO is uncommon. However, stroke progression is common, and the prognosis of most patients is poor. Rescue management such as EVT might be considered for symptomatic BVAO.
Figure
Reference
-
1. Caplan L. Posterior circulation ischemia: then, now, and tomorrow. The Thomas Willis lecture-2000. Stroke. 2000; 31:2011–2023.
Article2. Caplan L, Chung CS, Wityk R, Glass T, Tapia J, Pazdera L, et al. New England Medical Center posterior circulation stroke registry: I. Methods, data base, distribution of brain lesions, stroke mechanisms, and outcomes. J Clin Neurol. 2005; 1:14–30.
Article3. Caplan LR. The intracranial vertebral artery: a neglected species. The Johann Jacob Wepfer Award 2012. Cerebrovasc Dis. 2012; 34:20–30.
Article4. Shin HK, Yoo KM, Chang HM, Caplan LR. Bilateral intracranial vertebral artery disease in the New England Medical Center, posterior circulation registry. Arch Neurol. 1999; 56:1353–1358.
Article5. Wityk RJ, Chang HM, Rosengart A, Han WC, DeWitt LD, Pessin MS, et al. Proximal extracranial vertebral artery disease in the New England Medical Center posterior circulation registry. Arch Neurol. 1998; 55:470–478.
Article6. Rüegg S, Engelter S, Jeanneret C, Hetzel A, Probst A, Steck AJ, et al. Bilateral vertebral artery occlusion resulting from giant cell arteritis: report of 3 cases and review of the literature. Medicine (Baltimore). 2003; 82:1–12.
Article7. Maitas O, Bob-Manuel T, Price J, Noor A, Obi K, Okoh N, et al. Vertebral artery interventions: a comprehensive updated review. Curr Cardiol Rev. 2023; 19:e170322202296.
Article8. Bogousslavsky J, Gates PC, Fox AJ, Barnett HJ. Bilateral occlusion of vertebral artery: clinical patterns and long-term prognosis. Neurology. 1986; 36:1309–1315.
Article9. Ortiz de Mendivil A, Alcalá-Galiano A, Ochoa M, Salvador E, Millán JM. Brainstem stroke: anatomy, clinical and radiological findings. Semin Ultrasound CT MR. 2013; 34:131–141.
Article10. Duan H, Chen L, Shen S, Zhang Y, Li C, Yi Z, et al. Staged endovascular treatment for symptomatic occlusion originating from the intracranial vertebral arteries in the early non-acute stage. Front Neurol. 2021; 12:673367.
Article11. Caplan LR. Bilateral distal vertebral artery occlusion. Neurology. 1983; 33:552–558.
Article12. Tariq N, Maud A, Shah QA, Suri MF, Qureshi AI. Clinical outcome of patients with acute posterior circulation stroke and bilateral vertebral artery occlusion. J Vasc Interv Neurol. 2011; 4:9–14.13. Xu Z, Ma N, Mo D, Wong EH, Gao F, Jiao L, et al. Endovascular recanalization for chronic symptomatic intracranial vertebral artery total occlusion. Minim Invasive Surg. 2014; 2014:949585.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Locked-in Syndrome Performed Endovascular Treatment for Vertebral Artery Dissection and Basilar Artery Occlusion Caused by a Golf Swing
- Endovascular Surgery of Vertebral Artery Dissecting Aneurysm
- Bilateral Vertebral Artery Dissecting Aneurysms: A Long Term Follow-up Results of Microsurgical Trapping and Proximal Occlusion
- Growing Thrombosed Dissecting Aneurysm of the Vertebral Artery after Endovascular Proximal Artery Occlusion: the Role of the Vasa Vasorum
- Strategic Dual Approach for the Management of a Symptomatic Giant Partially Thrombosed Aneurysm at the Basilar Tip - Integrating Intrasaccular Flow Diversion and Endovascular Flow Reversal