Healthc Inform Res.
2024 Jan;30(1):60-72. 10.4258/hir.2024.30.1.60.
Prediction of Cervical Cancer Patients’ Survival Period with Machine Learning Techniques
- Affiliations
-
- 1Master’s Degree Program in Industrial Engineering, Faculty of Engineering, Chiang Mai University, Chiang Mai, Thailand
- 2Division of Radiation Oncology, Department of Radiology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
- 3Department of Industrial Engineering, Faculty of Engineering, Chiang Mai University, Chiang Mai, Thailand
- KMID: 2551861
- DOI: http://doi.org/10.4258/hir.2024.30.1.60
Abstract
Objectives
The objective of this research is to apply machine learning (ML) algorithms to predict the survival of cervical cancer patients. The aim was to address the limitations of traditional statistical methods, which often fail to provide accurate answers due to the complexity of the problem.
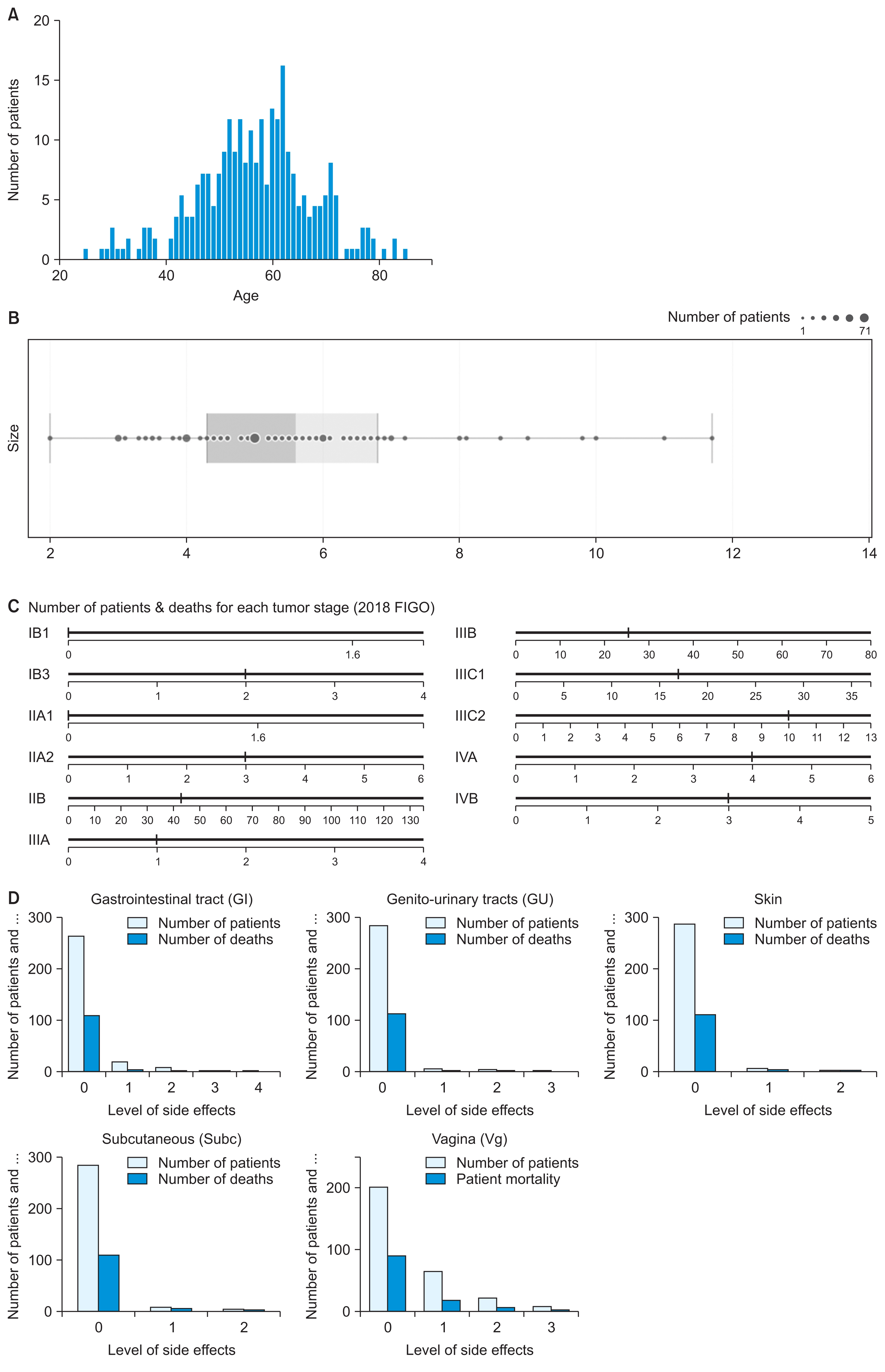
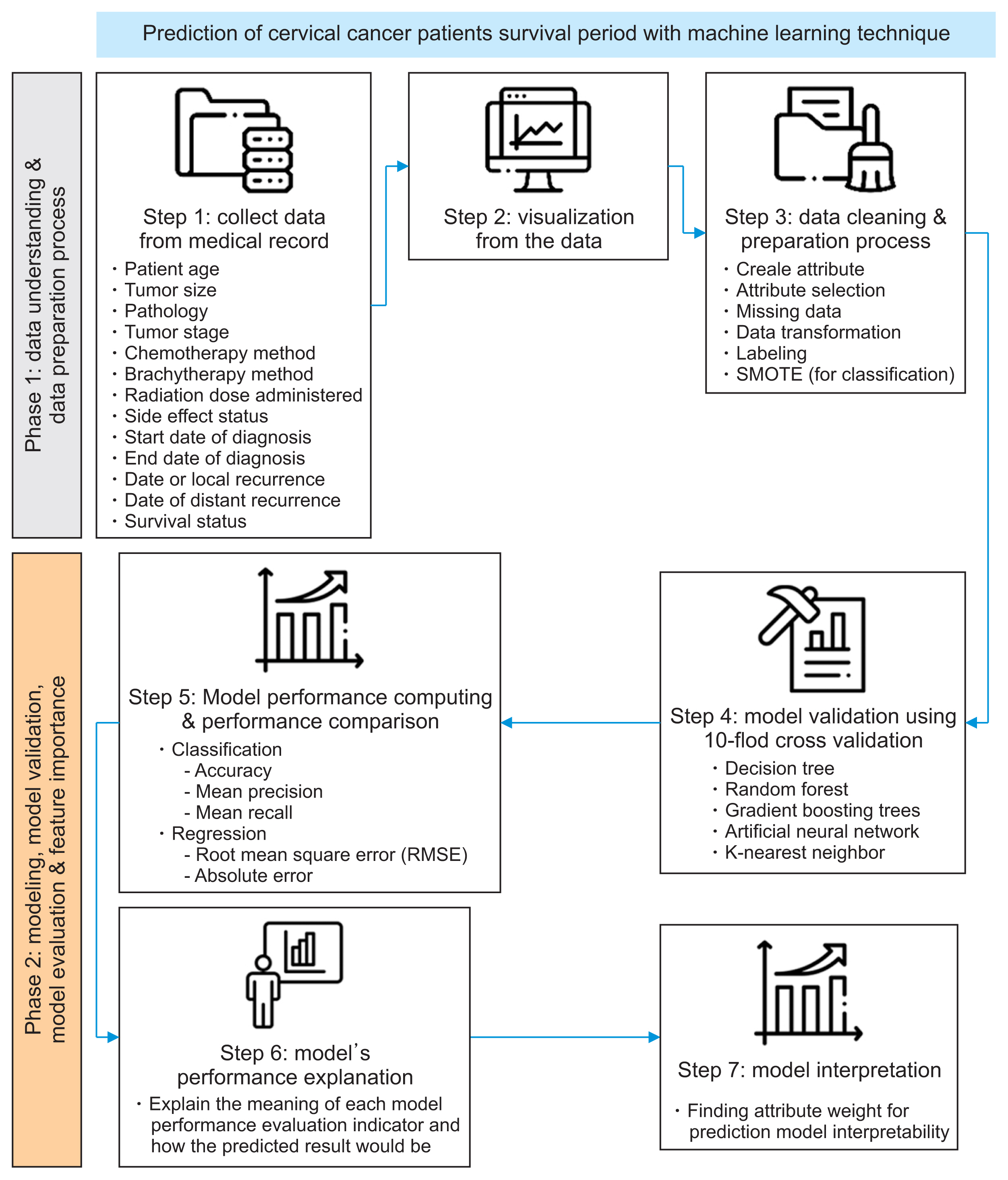
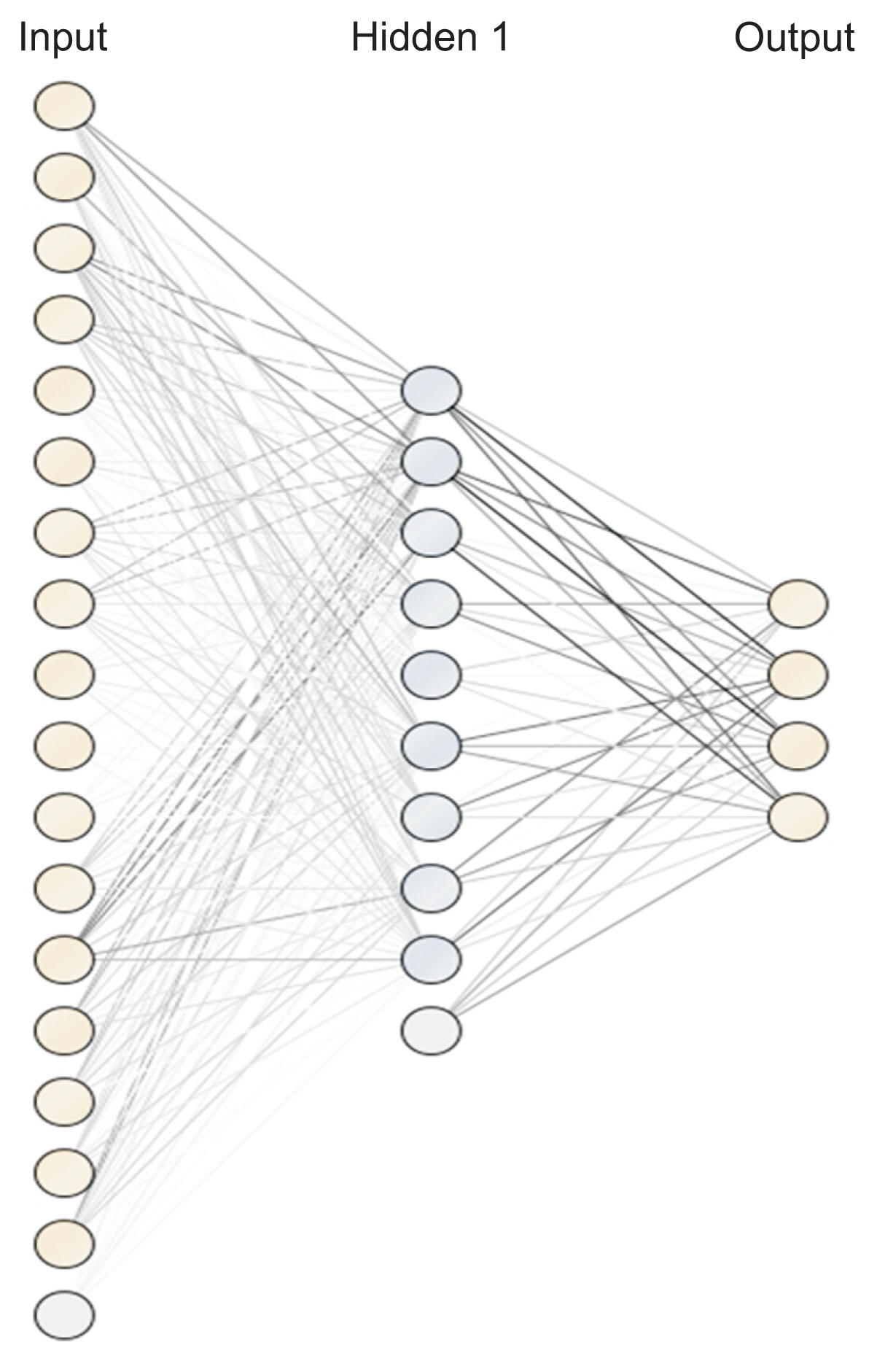
Methods
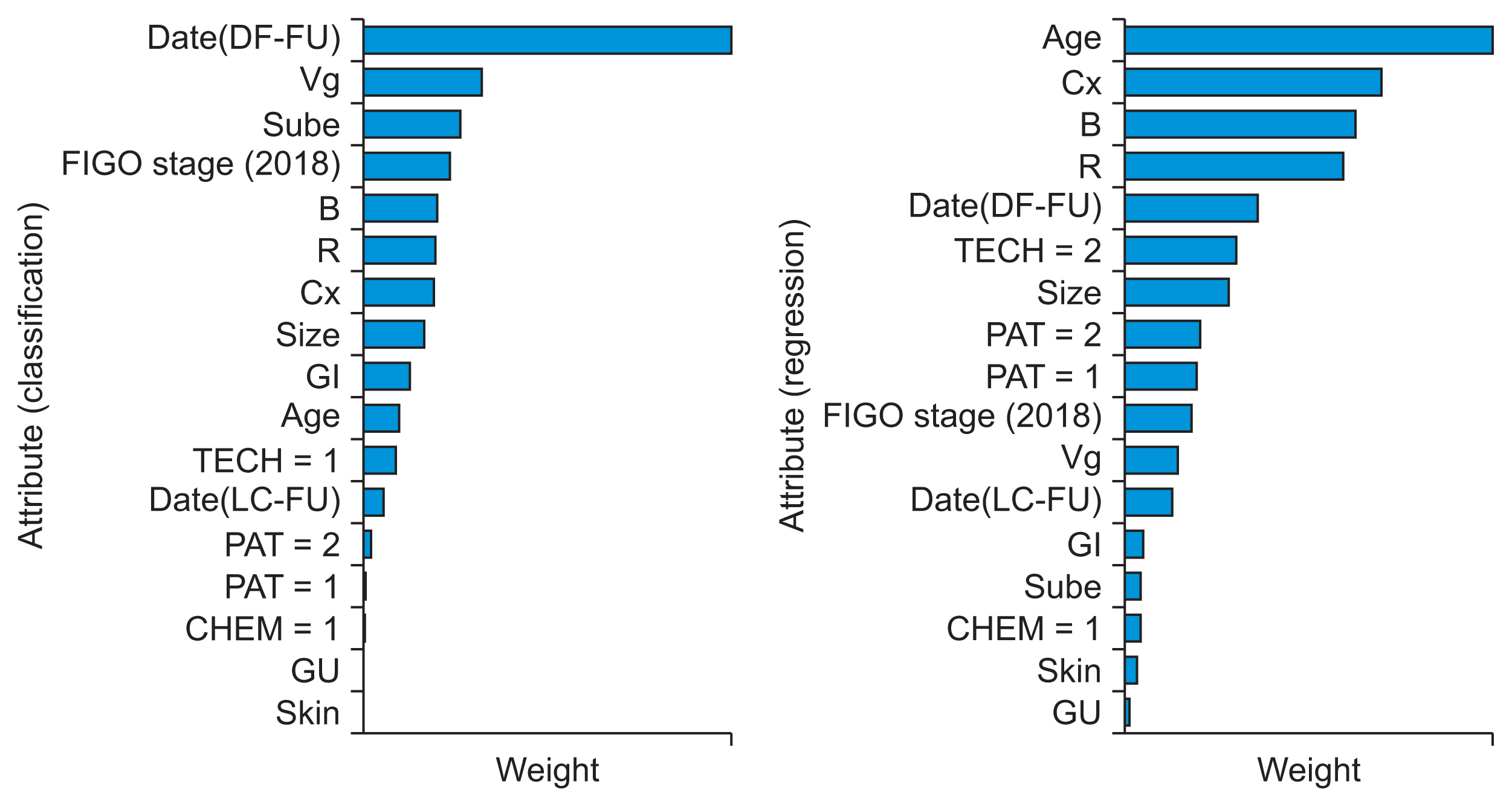
This research employed visualization techniques for initial data understanding. Subsequently, ML algorithms were used to develop both classification and regression models for survival prediction. In the classification models, we trained the algorithms to predict the time interval between the initial diagnosis and the patient’s death. The intervals were categorized as “<6 months,” “6 months to 3 years,” “3 years to 5 years,” and “>5 years.” The regression model aimed to predict survival time (in months). We used attribute weights to gain insights into the model, highlighting features with a significant impact on predictions and offering valuable insights into the model’s behavior and decision-making process.
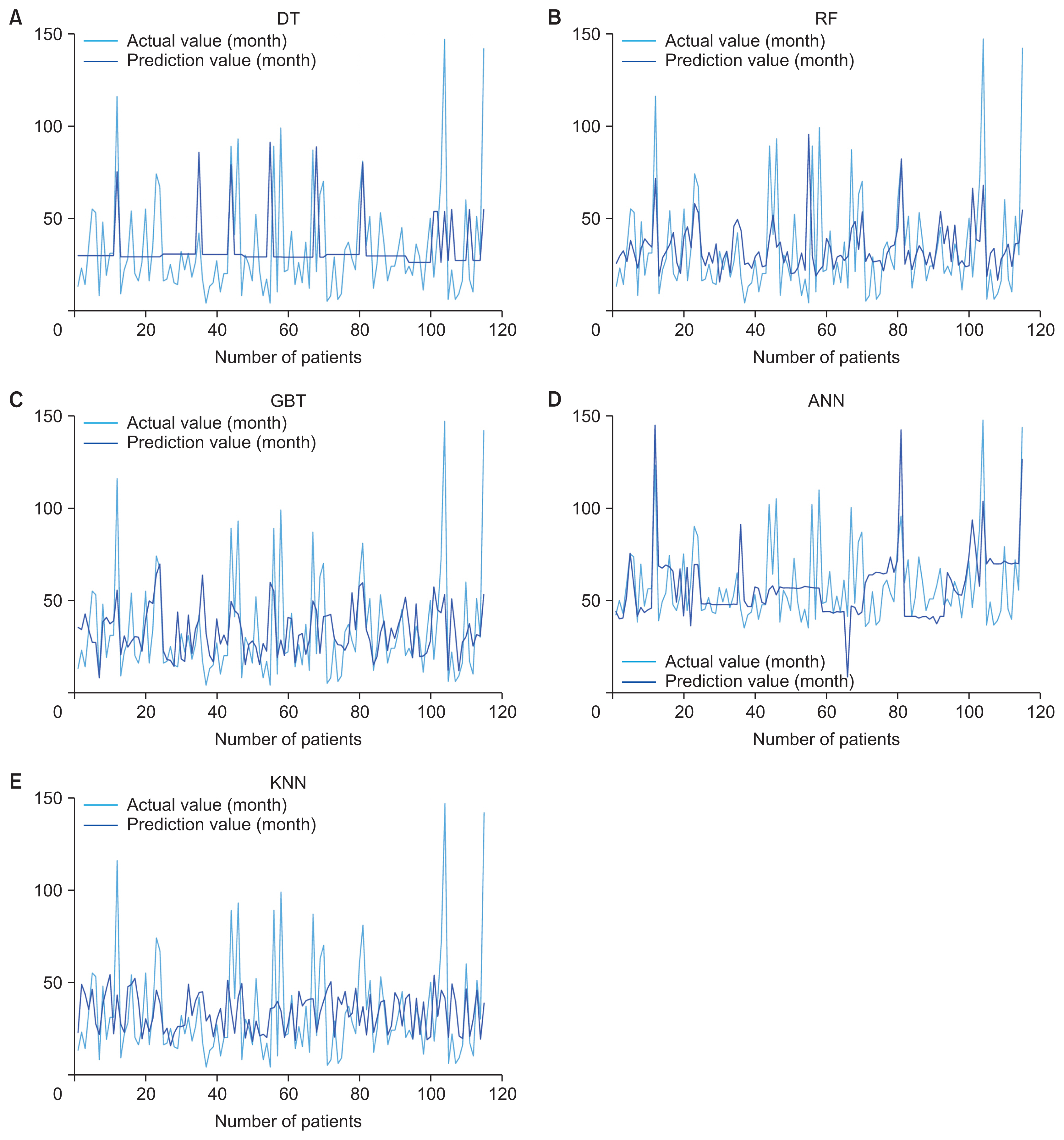
Results
The gradient boosting trees algorithm achieved an 81.55% accuracy in the classification model, while the random forest algorithm excelled in the regression model, with a root mean square error of 22.432. Notably, radiation doses around the affected areas significantly influenced survival duration.
Conclusions
Machine learning demonstrated the ability to provide high-accuracy predictions of survival periods in both classification and regression problems. This suggests its potential use as a decision-support tool in the process of treatment planning and resource allocation for each patient.
Keyword
Figure
Reference
-
References
1. Hassanpour SH, Dehghani M. Review of cancer from perspective of molecular. J Cancer Res Pract. 2017; 4(4):127–9. https://doi.org/10.1016/j.jcrpr.2017.07.001.
Article2. Sudhakar A. History of cancer, ancient and modern treatment methods. J Cancer Sci Ther. 2009; 1(2):1–4. https://doi.org/10.4172/1948-5956.100000e2.
Article3. Schneider IJ, Schmidt TP, dos Santos AM, Correa VP, Garcia LP, de Oliveira C, et al. Overall survival analyses of female malignancies in Southern Brazil during 2008–2017: a closer look at breast, cervical and ovarian cancer. Dialogues Health. 2022; 1:100010. https://doi.org/10.1016/j.dialog.2022.100010.
Article4. Vaiyapuri T, Alaskar H, Syed L, Aljohani E, Alkhayyat A, Shankar K, et al. Modified metaheuristics with stacked sparse denoising autoencoder model for cervical cancer classification. Comput Electr Eng. 2022; 103:108292. https://doi.org/10.1016/j.compeleceng.2022.108292.
Article5. Riano I, Contreras-Chavez P, Pabon CM, Meza K, Kiel L, Bejarano S, et al. An overview of cervical cancer prevention and control in Latin America and the Caribbean countries. Hematol Oncol Clin North Am. 2024; 38(1):13–33. https://doi.org/10.1016/j.hoc.2023.05.012.
Article6. Parvathi AJ, Gopika H, Suresh J, Sree SL, Harikumar S. Machine learning based approximate query processing for women health analytics. Procedia Comput Sci. 2023; 218:174–88. https://doi.org/10.1016/j.procs.2022.12.413.
Article7. Lee SH, Abdul Rahim N, Ong SK, Abdul Rahman H, Naing L. Survival of cervical cancer patients in Brunei Darussalam: 2002–2017. Heliyon. 2023; 9(5):e16080. https://doi.org/10.1016/j.heliyon.2023.e16080.
Article8. Khan A, Hussain S, Iyer JK, Kaul A, Bonnewitz M, Kaul R. Human papillomavirus-mediated expression of complement regulatory proteins in human cervical cancer cells. Eur J Obstet Gynecol Reprod Biol. 2023; 288:222–8. https://doi.org/10.1016/j.ejogrb.2023.07.014.
Article9. Alabi RO, Makitie AA, Pirinen M, Elmusrati M, Leivo I, Almangush A. Comparison of nomogram with machine learning techniques for prediction of overall survival in patients with tongue cancer. Int J Med Inform. 2021; 145:104313. https://doi.org/10.1016/j.ijmedinf.2020.104313.
Article10. Zhu S, Zheng Z, Hu W, Lei C. Conditional cancer-specific survival for inflammatory breast cancer: analysis of SEER, 2010 to 2016. Clin Breast Cancer. 2023; 23(6):628–39. https://doi.org/10.1016/j.clbc.2023.05.005.
Article11. Zhao M, Huang W, Zou S, Shen Q, Zhu X. A five-genes-based prognostic signature for cervical cancer overall survival prediction. Int J Genomics. 2020; 2020:8347639. https://doi.org/10.1155/2020/8347639.
Article12. Kleinbaum DG, Klein M. Survival analysis a self-learning text. 3rd ed. New York (NY): Springer;2012. https://doi.org/10.1007/978-1-4419-6646-9.
Article13. Rebernick RJ, Bell HN, Wakeam E. Survival analyses: a statistical review for surgeons. Semin Thorac Cardiovasc Surg. 2022; 34(4):1388–94. https://doi.org/10.1053/j.semtcvs.2022.01.001.
Article14. Matsuo K, Purushotham S, Jiang B, Mandelbaum RS, Takiuchi T, Liu Y, et al. Survival outcome prediction in cervical cancer: Cox models vs deep-learning model. Am J Obstet Gynecol. 2019; 220(4):381. https://doi.org/10.1016/j.ajog.2018.12.030.
Article15. Adeoye J, Tan JY, Choi SW, Thomson P. Prediction models applying machine learning to oral cavity cancer outcomes: a systematic review. Int J Med Inform. 2021; 154:104557. https://doi.org/10.1016/j.ijmedinf.2021.104557.
Article16. Su Y, Tian X, Gao R, Guo W, Chen C, Chen C, et al. Colon cancer diagnosis and staging classification based on machine learning and bioinformatics analysis. Comput Biol Med. 2022; 145:105409. https://doi.org/10.1016/j.compbiomed.2022.105409.
Article17. Guo C, Wang J, Wang Y, Qu X, Shi Z, Meng Y, et al. Novel artificial intelligence machine learning approaches to precisely predict survival and site-specific recurrence in cervical cancer: a multi-institutional study. Transl Oncol. 2021; 14(5):101032. https://doi.org/10.1016/j.tranon.2021.101032.
Article18. Lynch CM, Abdollahi B, Fuqua JD, de Carlo AR, Bartholomai JA, Balgemann RN, et al. Prediction of lung cancer patient survival via supervised machine learning classification techniques. Int J Med Inform. 2017; 108:1–8. https://doi.org/10.1016/j.ijmedinf.2017.09.013.
Article19. Wang Y, Ji C, Wang Y, Ji M, Yang JJ, Zhou CM. Predicting postoperative liver cancer death outcomes with machine learning. Curr Med Res Opin. 2021; 37(4):629–34. https://doi.org/10.1080/03007995.2021.1885361.
Article20. Akcay M, Etiz D, Celik O, Ozen A. Evaluation of prognosis in nasopharyngeal cancer using machine learning. Technol Cancer Res Treat. 2020; 19:1533033820909829. https://doi.org/10.1177/1533033820909829.
Article21. Tapak L, Shirmohammadi-Khorram N, Amini P, Alafchi B, Hamidi O, Poorolajal J. Prediction of survival and metastasis in breast cancer patients using machine learning classifiers. Clin Epidemiol Glob Health. 2019; 7(3):293–9. https://doi.org/10.1016/j.cegh.2018.10.003.
Article22. Tharavichitkul E, Jia-Mahasap B, Muangwong P, Chakrabandhu S, Klunklin P, Onchan W, et al. Survival outcome of cervical cancer patients treated by image-guided brachytherapy: a ‘real world’ single center experience in Thailand from 2008 to 2018. J Radiat Res. 2022; 63(4):657–65. https://doi.org/10.1093/jrr/rrac025.
Article23. Zhou YY, Chang M, Li CP, Han XL, Fang P, Xia XP. Causal effect of age first had sexual intercourse and lifetime number of sexual partners on cervical cancer. Heliyon. 2023; 10(1):e23758. https://doi.org/10.1016/j.heliyon.2023.e23758.
Article24. Gill BS, Lin JF, Krivak TC, Sukumvanich P, Laskey RA, Ross MS, et al. National Cancer Data Base analysis of radiation therapy consolidation modality for cervical cancer: the impact of new technological advancements. Int J Radiat Oncol Biol Phys. 2014; 90(5):1083–90. https://doi.org/10.1016/j.ijrobp.2014.07.017.
Article25. Fiste O, Liontos M, Zagouri F, Stamatakos G, Dimopoulos MA. Machine learning applications in gynecological cancer: a critical review. Crit Rev Oncol Hematol. 2022; 179:103808. https://doi.org/10.1016/j.critrevonc.2022.103808.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Machine Learning vs. Statistical Model for Prediction Modelling: Application in Medical Imaging Research
- Predictive Modeling of Outcomes After Traumatic and Nontraumatic Spinal Cord Injury Using Machine Learning: Review of Current Progress and Future Directions
- Clinico-pathologic Factors and Machine Learning Algorithm for Survival Prediction in Parotid Gland Cancer
- Prediction of Diabetic Neuropathy Using Machine Learning Techniques
- Machine Learning-Based Predictor for Treatment Outcomes of Patients With Salivary Gland Cancer After Operation