J Stroke.
2024 Jan;26(1):108-111. 10.5853/jos.2023.02768.
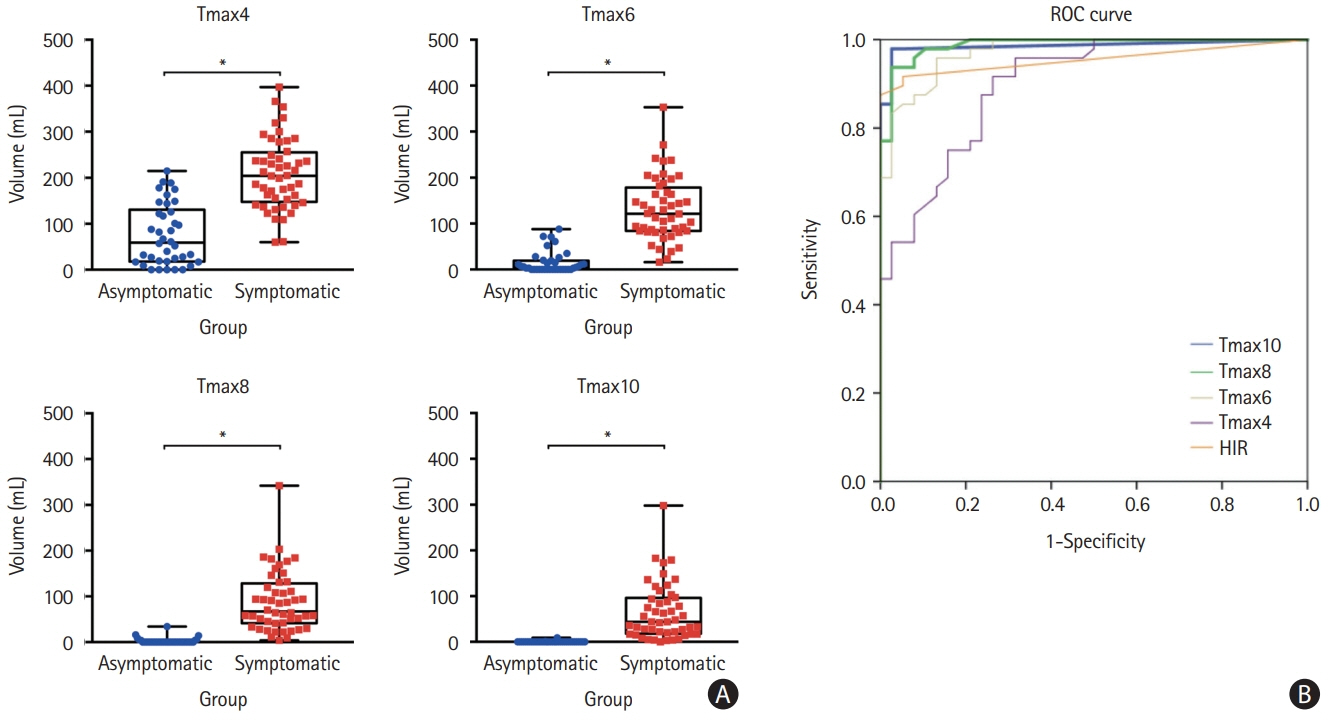
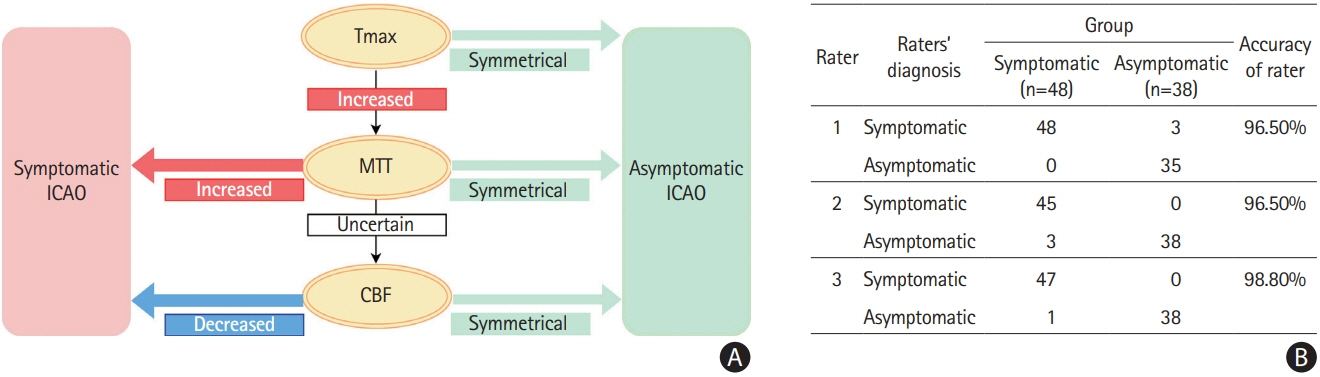
Perfusion Profiles May Differ Between Asymptomatic Versus Symptomatic Internal Carotid Artery Occlusion
- Affiliations
-
- 1Department of Neurology and Neurological Sciences, Stanford Stroke Center, Palo Alto, CA, USA
- 2Department of Neurology, Stroke Center, Chang Gung Memorial Hospital and Chang Gung University, Taoyuan, Taiwan
- 3Department of Diagnostic and Interventional Neuroradiology, Stanford University School of Medicine, Stanford, CA, USA
- KMID: 2551353
- DOI: http://doi.org/10.5853/jos.2023.02768
Figure
Reference
-
References
1. Sarraj A, Albers GW, Blasco J, Arenillas JF, Ribo M, Hassan AE, et al. Thrombectomy versus medical management in mild strokes due to large vessel occlusion: exploratory analysis from the EXTEND-IA trials and a pooled international cohort. Ann Neurol. 2022; 92:364–378.2. Lansberg MG, Straka M, Kemp S, Mlynash M, Wechsler LR, Jovin TG, et al. MRI profile and response to endovascular reperfusion after stroke (DEFUSE 2): a prospective cohort study. Lancet Neurol. 2012; 11:860–867.3. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, OrtegaGutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–718.4. Guenego A, Marcellus DG, Martin BW, Christensen S, Albers GW, Lansberg MG, et al. Hypoperfusion intensity ratio is correlated with patient eligibility for thrombectomy. Stroke. 2019; 50:917–922.5. Zhang B, Wang G, Gao Y, Tan H, Wang P. Influence of the integrity of circle of Willis on asymptomatic or mild patients with first diagnosed chronic internal carotid artery occlusion. Eur J Radiol. 2023; 165:110954.6. Lee MJ, Son JP, Kim SJ, Ryoo S, Woo SY, Cha J, et al. Predicting collateral status with magnetic resonance perfusion parameters: probabilistic approach with a Tmax-derived prediction model. Stroke. 2015; 46:2800–2807.7. Ishikawa M, Sugawara H, Nagai M, Kusaka G, Tanaka Y, Naritaka H. Collateral flow and white matter disease in patients with internal carotid artery occlusion. Eur Neurol. 2017; 77:56–65.8. Chaves CJ, Staroselskaya I, Linfante I, Llinas R, Caplan LR, Warach S. Patterns of perfusion-weighted imaging in patients with carotid artery occlusive disease. Arch Neurol. 2003; 60:237–242.9. Calamante F, Christensen S, Desmond PM, Ostergaard L, Davis SM, Connelly A. The physiological significance of the time-to-maximum (Tmax) parameter in perfusion MRI. Stroke. 2010; 41:1169–1174.10. Thanvi B, Robinson T. Complete occlusion of extracranial internal carotid artery: clinical features, pathophysiology, diagnosis and management. Postgrad Med J. 2007; 83:95–99.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Carotid Artery Occlusive Diseases Treated with Staged Subclavian-carotid Artery bypass and Carotid Endarterectomy: Case Report
- Patterns of Stroke and Collateralization of the Internal Carotid Artery Occlusion in the Neck
- Anesthetic management of a patient with bilateral common carotid and subclavian arteries occlusion using cerebral oximetry monitoring: A case report
- Asymptomatic Bilateral Internal Carotid Artery Occlusion with Ring Finger Protein 213 Gene Polymorphism
- Symptomatic Bilateral Carotid Artery Occlusion: An Uncommon Pattern of Carotid Pathology