J Stroke.
2024 Jan;26(1):41-53. 10.5853/jos.2023.01613.
Mechanical Thrombectomy for In-Hospital Onset Stroke: A Comparative Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Radiology, Mayo Clinic, Rochester, MN, USA
- 2Department of Radiology, Keck School of Medicine, University of Southern California (USC), Los Angeles, CA, USA
- 3Department of Neurological Surgery, Mayo Clinic, Rochester, MN, USA
- KMID: 2551346
- DOI: http://doi.org/10.5853/jos.2023.01613
Abstract
- Background and Purpose
In-hospital onset stroke (IHOS) accounts for a significant proportion of large vessel occlusion acute ischemic strokes, leading to worse outcomes due to delays in evaluation and treatment. Limited data is available on the effectiveness of mechanical thrombectomy in IHOS patients. This study aims to assess the safety and efficacy of mechanical thrombectomy for patients with IHOS and compare the outcomes with those of community-onset strokes (COS).
Methods
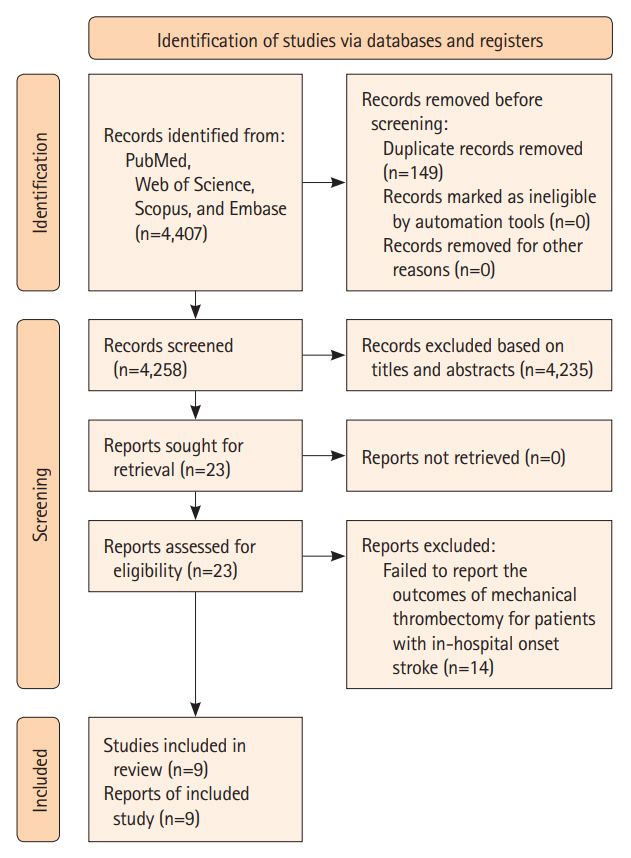
We conducted a systematic review and meta-analysis following established guidelines, by searching PubMed, Scopus, Web of Science, and Embase databases up to April 11, 2023. Eligible studies reporting outcomes of interest were included, and relevant data was extracted and analyzed using Stata software version 17.0.
Results
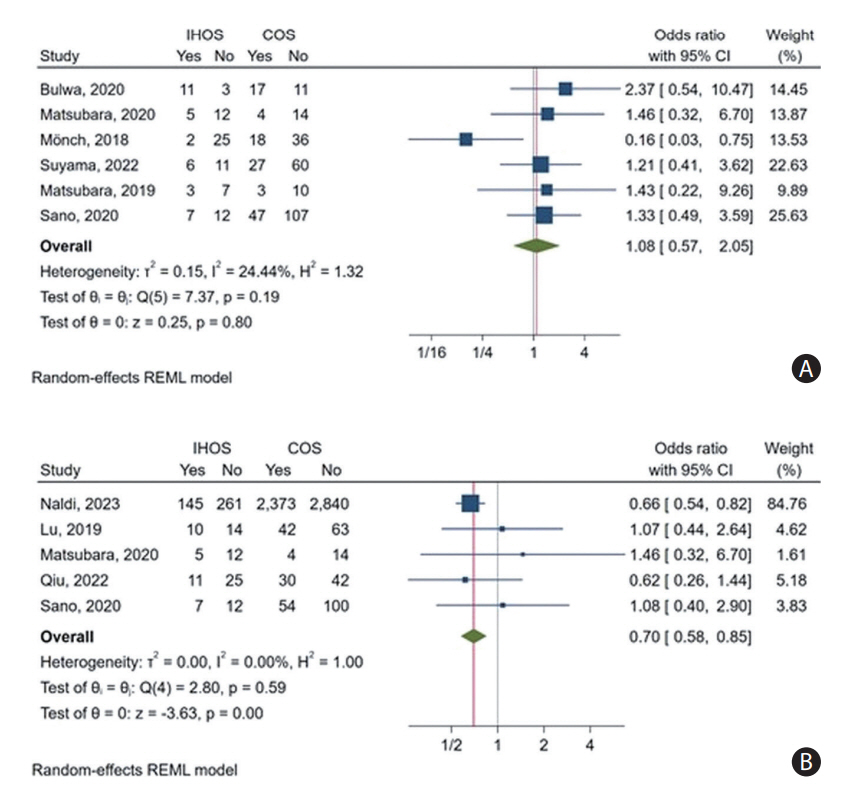
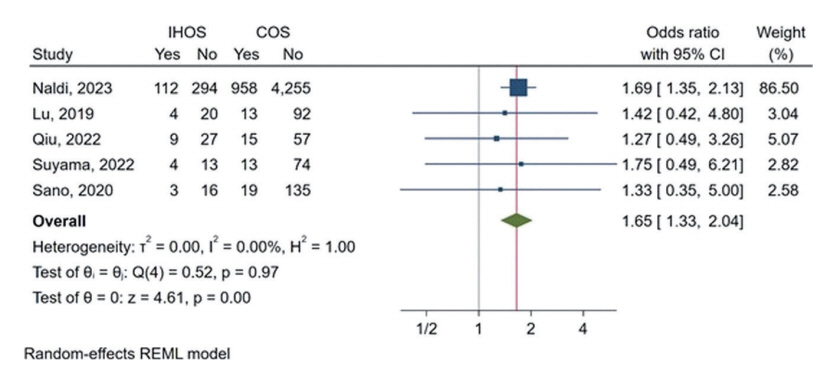
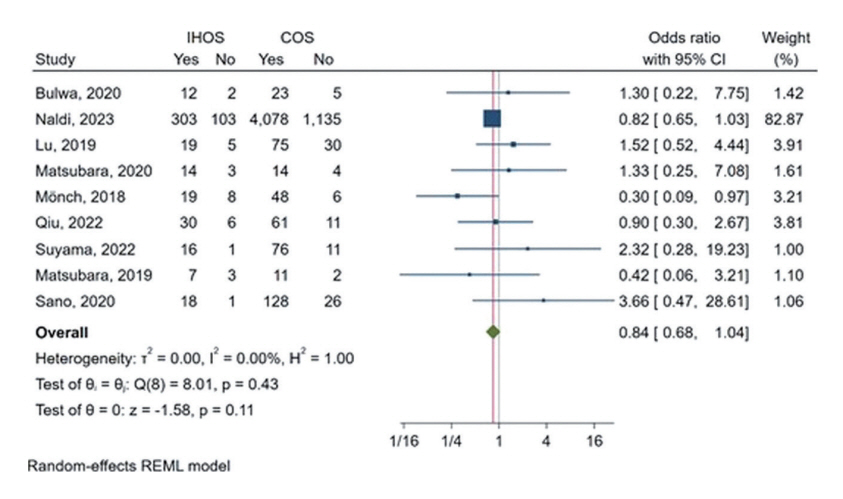
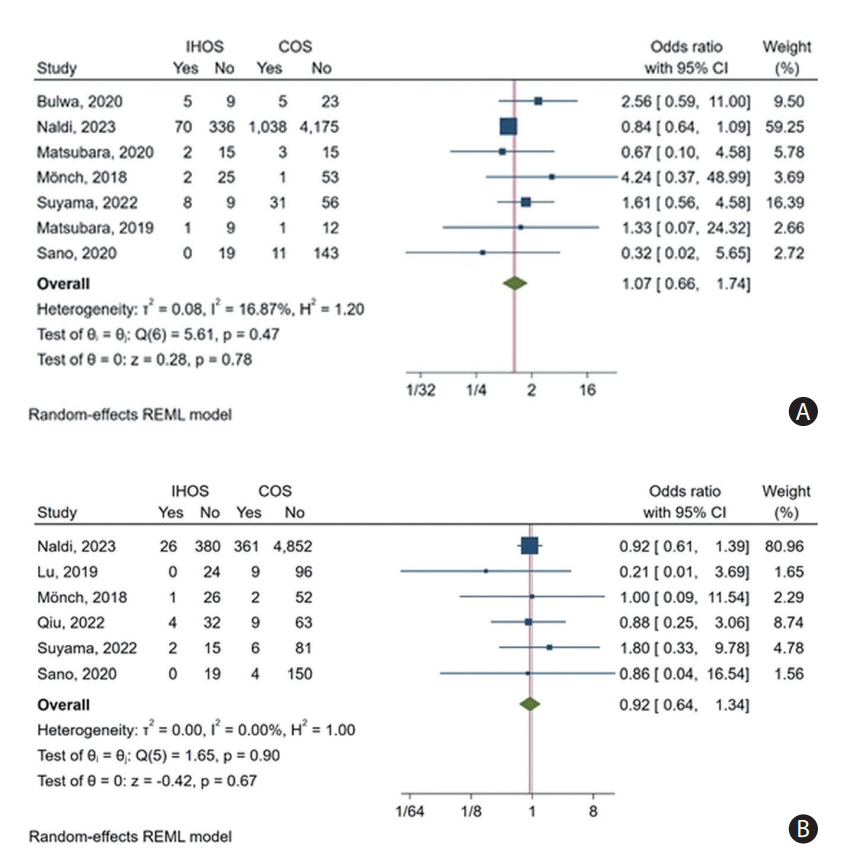
In a meta-analysis of nine studies, comprising 540 cases of IHOS and 5,744 cases of COS, IHOS cases had a significantly lower rate of good functional outcomes on follow-up (35.46% vs. 40.74%, P<0.01) and a higher follow-up mortality rate (26.29% vs. 18.08%, P<0.01) compared to COS patients. Both groups had comparable successful recanalization rates (IHOS: 79.32% vs. COS: 81.44%, P=0.11), incidence rates of periprocedural complications (IHOS: 15.10%, COS: 12.96%, P=0.78), and symptomatic intracranial hemorrhage (IHOS: 6.24%, COS: 6.88%, P=0.67). It is worth noting that much of the observed effect size for mortality and good functional outcomes on follow-up was derived from only one and two studies, respectively.
Conclusion
While the current literature suggests that mechanical thrombectomy is a safe and effective treatment for IHOS, further research is necessary to comprehensively evaluate its impact, particularly during follow-up.
Keyword
Figure
Reference
-
References
1. Lu MY, Chen CH, Yeh SJ, Tsai LK, Lee CW, Tang SC, et al. Comparison between in-hospital stroke and community-onset stroke treated with endovascular thrombectomy. PLoS One. 2019; 14:e0214883.2. Suyama K, Matsumoto S, Nakahara I, Suyama Y, Morioka J, Hasebe A, et al. Delays in initial workflow cause delayed initiation of mechanical thrombectomy in patients with in-hospital ischemic stroke. Fujita Med J. 2022; 8:73–78.3. Naldi A, Pracucci G, Cavallo R, Saia V, Boghi A, Lochner P, et al. Mechanical thrombectomy for in-hospital stroke: data from the Italian registry of endovascular treatment in acute stroke. J Neurointerv Surg. 2023; Mar. 7. [Epub]. https://doi.org/10.1136/jnis-2022-019939.4. Bulwa Z, Del Brutto VJ, Loggini A, Ammar FE, Martinez RC, Christoforidis G, et al. Mechanical thrombectomy for patients with in-hospital ischemic stroke: a case-control study. J Stroke Cerebrovasc Dis. 2020; 29:104692.5. Matsubara N, Hiramatsu R, Yagi R, Ohnishi H, Miyachi S, Futamura G, et al. Characteristics and treatment results of in-hospital acute ischemic stroke due to large vessel occlusion treated by mechanical thrombectomy. J Neuroendovascular Ther. 2019; 13:281–287.6. Qiu K, Zu QQ, Zhao LB, Liu S, Shi HB. Outcomes between in-hospital stroke and community-onset stroke after thrombectomy: propensity-score matching analysis. Interv Neuroradiol. 2022; 28:296–301.7. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6:e1000097.8. Sterne JA, Hernán MA, Reeves BC, Savovic´ J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016; 355:i4919.9. Brown LD, Cai TT, DasGupta A. Interval estimation for a binomial proportion. Statist Sci. 2001; 16:101–133.10. McGrath S, Sohn H, Steele R, Benedetti A. Meta-analysis of the difference of medians. Biom J. 2020; 62:69–98.11. McGrath S, Katzenschlager S, Zimmer AJ, Seitel A, Steele R, Benedetti A. Standard error estimation in meta-analysis of studies reporting medians. Stat Methods Med Res. 2023; 32:373–388.12. Galbraith RF. The radial plot: graphical assessment of spread in ages. Int J Rad Appl Instrum D. 1990; 17:207–214.13. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000; 56:455–463.14. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634.15. Nyaga VN. METAPREG: Stata module to compute fixed and random effects meta-analysis and meta-regression of proportions. Statistical Software Components S458693 [Internet]. Chestnut Hill, MA: Boston College, Department of Economics;2019. [accessed May 1, 2023]. Available from: https://ideas.repec.org/c/boc/bocode/s458693.html.16. McGrath S, Zhao X, Ozturk O, Katzenschlager S, Steele R, Benedetti A. Metamedian: an R package for meta-analyzing studies reporting medians. arXiv [Preprint]. 2023. [accessed 2023 May 1]. Available at: https://doi.org/10.48550/arXiv.2302.14243.17. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010; 36:1–48.18. Mönch S, Lehm M, Maegerlein C, Hedderich D, Berndt M, Boeckh-Behrens T, et al. Worse endovascular mechanical recanalization results for patients with in-hospital onset acute ischemic stroke. J Neurol. 2018; 265:2525–2530.19. Sano T, Kobayashi K, Ichikawa T, Hakozaki K, Tanemura H, Ishigaki T, et al. In-hospital ischemic stroke treated by mechanical thrombectomy. J Neuroendovasc Ther. 2020; 14:133–140.20. Matsubara N, Hiramatsu R, Yagi R, Ohnishi H, Miyachi S, Tsuji Y, et al. Other hospital-onset acute ischemic stroke due to large vessel occlusion treated by mechanical thrombectomy after inter-hospital transfer. Neurol Med Chir (Tokyo). 2020; 60:209–216.21. Cumbler E. In-hospital ischemic stroke. Neurohospitalist. 2015; 5:173–181.22. Kassardjian CD, Willems JD, Skrabka K, Nisenbaum R, Barnaby J, Kostyrko P, et al. In-patient code stroke: a quality improvement strategy to overcome knowledge-to-action gaps in response time. Stroke. 2017; 48:2176–2183.23. Almutairi S, Choudhury H, Najm M, Bala F, Almekhlafi MA. Workflow and outcomes of endovascular thrombectomy for in-hospital stroke a systematic review and meta-analysis. J Stroke Cerebrovasc Dis. 2021; 30:105937.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mechanical Thrombectomy in Strokes with Large-Vessel Occlusion Beyond 6 Hours: A Pooled Analysis of Randomized Trials
- Safety and Efficacy of Mechanical Thrombectomy with Solitaire Stent Retrieval for Acute Ischemic Stroke: A Systematic Review
- Clot Composition Analysis as a Diagnostic Tool to Gain Insight into Ischemic Stroke Etiology: A Systematic Review
- Paradigm Shift in Intra-Arterial Mechanical Thrombectomy for Acute Ischemic Stroke : A Review of Randomized Controlled Trials after 2015
- Mothership versus Drip-and-Ship Model for Mechanical Thrombectomy in Acute Stroke: A Systematic Review and Meta-Analysis for Clinical and Radiological Outcomes