J Korean Med Sci.
2024 Jan;39(3):e32. 10.3346/jkms.2024.39.e32.
Risk Factors and Trends in Adolescent’s Suicide Attempt Rates Before and After the Coronavirus Disease 2019 Pandemic
- Affiliations
-
- 1Department of Psychiatry, Wonkwang University Hospital, Iksan, Korea
- 2Department of Psychiatry, School of Medicine, Wonkwang University, Iksan, Korea
- 3Department of Psychiatry, Incheon Chamsarang Hospital, Incheon, Korea
- KMID: 2551179
- DOI: http://doi.org/10.3346/jkms.2024.39.e32
Abstract
- Background
Understanding adolescents’ mental health during the coronavirus disease 2019 (COVID-19) pandemic and identifying those most at risk is an urgent public health challenge. This study explored the trend of suicide attempts and the association between loneliness, family financial stress, and suicide attempts during the COVID-19 pandemic among adolescents.
Methods
Data of the 2020 to 2022 Korea Youth Risk Behavior Surveys for adolescents aged 13–18 years were used. Multivariate logistic regression analyses were performed to examine the association between suicide attempts, family financial stress, and loneliness during the COVID-19 pandemic.
Results
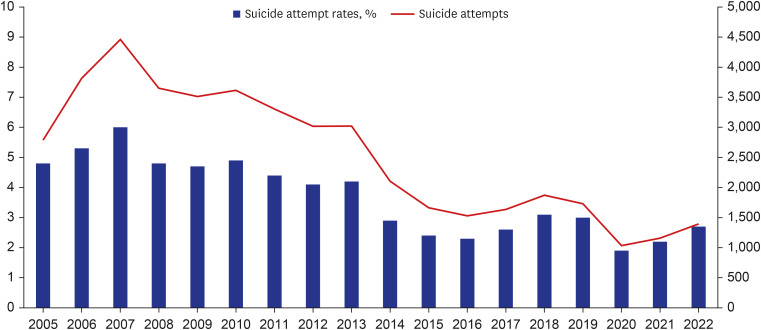
The trend of suicide attempt rates was lowest in 2020 (1.9%, 1,034 out of 53,534) and it showed an increasing trend with rates of 2.2% (1,159 out of 53,445) in 2021 and 2.5% (1,271 out of 50,455) in 2022. The risk of suicide attempt was higher among adolescents who experienced financial stress (in 2020: adjusted odds ratio [AOR], 1.53, 95% confidence interval [CI], 1.26–1.88; in 2021: AOR, 1.63, 95% CI, 1.03–1.54) and felt lonely (in 2020: AOR, 2.19, 95% CI, 1.78–2.70; in 2021: AOR, 2.65, 95% CI, 2.16–3.26; in 2022: AOR, 1.3, 95% CI, 1.04–1.55) than those who did not.
Conclusion
The COVID-19 pandemic affected the suicide attempts of adolescents, with financial stress and feelings of loneliness closely linked to this impact. Although the pandemic nears its end, the persistent risk of suicide attempts among adolescents remains a concern. Therefore, it is imperative to implement targeted screening and interventions to address adolescent suicide risk.
Keyword
Figure
Reference
-
1. Jones EAK, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health. 2021; 18(5):2470. PMID: 33802278.2. Bruining H, Bartels M, Polderman TJC, Popma A. COVID-19 and child and adolescent psychiatry: an unexpected blessing for part of our population? Eur Child Adolesc Psychiatry. 2021; 30(7):1139–1140. PMID: 32623697.3. Zalsman G, Stanley B, Szanto K, Clarke DE, Carli V, Mehlum L. Suicide in the time of COVID-19: review and recommendations. Arch Suicide Res. 2020; 24(4):477–482. PMID: 33200946.4. Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020; 7(10):883–892. PMID: 32707037.5. Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020; 291:113264. PMID: 32622172.6. Kim KW, Lim JS, Yang CM, Jang SH, Lee SY. Classification of adolescent psychiatric patients at high risk of suicide using the personality assessment inventory by machine learning. Psychiatry Investig. 2021; 18(11):1137–1143.7. Golberstein E, Gonzales G, Meara E. How do economic downturns affect the mental health of children? Evidence from the National Health Interview Survey. Health Econ. 2019; 28(8):955–970. PMID: 31165566.8. Magson NR, Freeman JY, Rapee RM, Richardson CE, Oar EL, Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J Youth Adolesc. 2021; 50(1):44–57. PMID: 33108542.9. Mansfield KL, Newby D, Soneson E, Vaci N, Jindra C, Geulayov G, et al. COVID-19 partial school closures and mental health problems: a cross-sectional survey of 11,000 adolescents to determine those most at risk. JCPP Adv. 2021; 1(2):e12021. PMID: 34514466.10. Kawohl W, Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020; 7(5):389–390. PMID: 32353269.11. Brenner MH, Bhugra D. Acceleration of anxiety, depression, and suicide: secondary effects of economic disruption related to COVID-19. Front Psychiatry. 2020; 11:592467. PMID: 33384627.12. Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020; 14(1):20. PMID: 32419840.13. Anderson KN, Swedo EA, Trinh E, Ray CM, Krause KH, Verlenden JV, et al. Adverse childhood experiences during the COVID-19 pandemic and associations with poor mental health and suicidal behaviors among high school students - adolescent behaviors and experiences survey, United States, January-June 2021. MMWR Morb Mortal Wkly Rep. 2022; 71(41):1301–1305. PMID: 36227769.14. Goto R, Okubo Y, Skokauskas N. Reasons and trends in youth’s suicide rates during the COVID-19 pandemic. Lancet Reg Health West Pac. 2022; 27:100567. PMID: 35966624.15. Durante JC, Lau M. Adolescents, suicide, and the COVID-19 pandemic. Pediatr Ann. 2022; 51(4):e144–e149. PMID: 35417315.16. Korea Disease Control and Prevention Agency. Korea Youth Risk Behavior Survey. Updated 2023. Accessed September 12, 2023. https://www.kdca.go.kr/yhs/home.jsp .17. Lim JS, Yang CM, Baek JW, Lee SY, Kim BN. Prediction models for suicide attempts among adolescents using machine learning techniques. Clin Psychopharmacol Neurosci. 2022; 20(4):609–620. PMID: 36263637.18. Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020; 113(10):707–712. PMID: 32539153.19. Mourouvaye M, Bottemanne H, Bonny G, Fourcade L, Angoulvant F, Cohen JF, et al. Association between suicide behaviours in children and adolescents and the COVID-19 lockdown in Paris, France: a retrospective observational study. Arch Dis Child. 2021; 106(9):918–919. PMID: 33355154.20. Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. 2021; 5(2):229–238. PMID: 33452498.21. Auger N, Low N, Chadi N, Israël M, Steiger H, Lewin A, et al. Suicide attempts in children aged 10-14 years during the first year of the COVID-19 pandemic. J Adolesc Health. 2023; 72(6):899–905. PMID: 36870902.22. Xiao Y, Junus A, Li T, Yip P. Temporal and spatial trends in suicide-related visits before and during the COVID-19 pandemic in the US, 2018-2021. J Affect Disord. 2023; 324:24–35. PMID: 36566936.23. Statistics Korea Statistics Research Institute. Children and Youth Well-being in Korea 2022 (Korean version). Updated 2023. Accessed July 30, 2023. https://kostat.go.kr/board.es?mid=b10105000000&bid=0060&act=view&list_no=426078&tag=&nPage=1&ref_bid= .24. Charpignon ML, Ontiveros J, Sundaresan S, Puri A, Chandra J, Mandl KD, et al. Evaluation of suicides among US adolescents during the COVID-19 pandemic. JAMA Pediatr. 2022; 176(7):724–726. PMID: 35467724.25. Madigan S, Racine N, Vaillancourt T, Korczak DJ, Hewitt JM, Pador P, et al. Changes in depression and anxiety among children and adolescents from before to during the COVID-19 pandemic: a systematic review and meta-analysis. JAMA Pediatr. 2023; 177(6):567–581. PMID: 37126337.26. Oliveira JM, Butini L, Pauletto P, Lehmkuhl KM, Stefani CM, Bolan M, et al. Mental health effects prevalence in children and adolescents during the COVID-19 pandemic: a systematic review. Worldviews Evid Based Nurs. 2022; 19(2):130–137. PMID: 35229967.27. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020; 7(4):e21. PMID: 32199510.28. Carr MJ, Steeg S, Webb RT, Kapur N, Chew-Graham CA, Abel KM, et al. Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: a population-based cohort study. Lancet Public Health. 2021; 6(2):e124–e135. PMID: 33444560.29. Cantor J, Sood N, Bravata DM, Pera M, Whaley C. The impact of the COVID-19 pandemic and policy response on health care utilization: evidence from county-level medical claims and cellphone data. J Health Econ. 2022; 82:102581. PMID: 35067386.30. Neppl TK, Senia JM, Donnellan MB. Effects of economic hardship: testing the family stress model over time. J Fam Psychol. 2016; 30(1):12–21. PMID: 26551658.31. Conger RD, Conger KJ, Elder GH Jr, Lorenz FO, Simons RL, Whitbeck LB. A family process model of economic hardship and adjustment of early adolescent boys. Child Dev. 1992; 63(3):526–541. PMID: 1600820.32. Argabright ST, Tran KT, Visoki E, DiDomenico GE, Moore TM, Barzilay R. COVID-19-related financial strain and adolescent mental health. Lancet Reg Health Am. 2022; 16:100391. PMID: 36405885.33. Holt-Lunstad J. A pandemic of social isolation? World Psychiatry. 2021; 20(1):55–56. PMID: 33432754.34. Binagwaho A. We need compassionate leadership management based on evidence to defeat COVID-19. Int J Health Policy Manag. 2020; 9(10):413–414. PMID: 32610733.35. Jones AC, Schinka KC, van Dulmen MH, Bossarte RM, Swahn MH. Changes in loneliness during middle childhood predict risk for adolescent suicidality indirectly through mental health problems. J Clin Child Adolesc Psychol. 2011; 40(6):818–824. PMID: 22023273.36. Ziedan E, Simon KI, Wing C. Effects of state COVID-19 closure policy on non-COVID-19 health care utilization. NBER Work Pap Ser. 2020; 27621.37. Qi M, Zhou SJ, Guo ZC, Zhang LG, Min HJ, Li XM, et al. The effect of social support on mental health in Chinese adolescents during the outbreak of COVID-19. J Adolesc Health. 2020; 67(4):514–518. PMID: 32753347.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influencing Factors on Suicide Attempt among Adolescents in South Korea
- Analysis of suicide statistics and trends between 2011 and 2021 among Korean women
- Association of the COVID-19 Pandemic and Low-rescue Suicide Attempts in Patients Visiting the Emergency Department after Attempting Suicide
- Suicide attempts presenting to the emergency department before and during the COVID-19 pandemic: a comparative study
- The Relationship Between Bullying and Risk of Suicide Among Adolescents During the COVID-19 Pandemic in Indonesia