Anesth Pain Med.
2023 Oct;18(4):421-430. 10.17085/apm.23029.
Single and double injection paravertebral block comparison in reduction mammaplasty cases: a randomized controlled study
- Affiliations
-
- 1Department of Anesthesiology and Reanimation, Liv Hospital Vadİstanbul, Istanbul, Turkiye
- 2Department of Anesthesiology, Washington University in St Louis, School of Medicine, St Louis, MO, USA
- 3Department of Anesthesiology and Reanimation, Istanbul University Istanbul Faculty of Medicine, Istanbul, Turkiye
- 4Department of Plastic, Reconstructive and Aesthetic Surgery, Istanbul University Istanbul Faculty of Medicine, Istanbul, Turkiye
- 5Department of Anesthesiology and Reanimation, Basaksehir Cam and Sakura State Hospital, Istanbul, Turkiye
- 6Department of Anesthesiology and Reanimation, Sancaktepe State Hospital, Istanbul, Turkiye
- KMID: 2550923
- DOI: http://doi.org/10.17085/apm.23029
Abstract
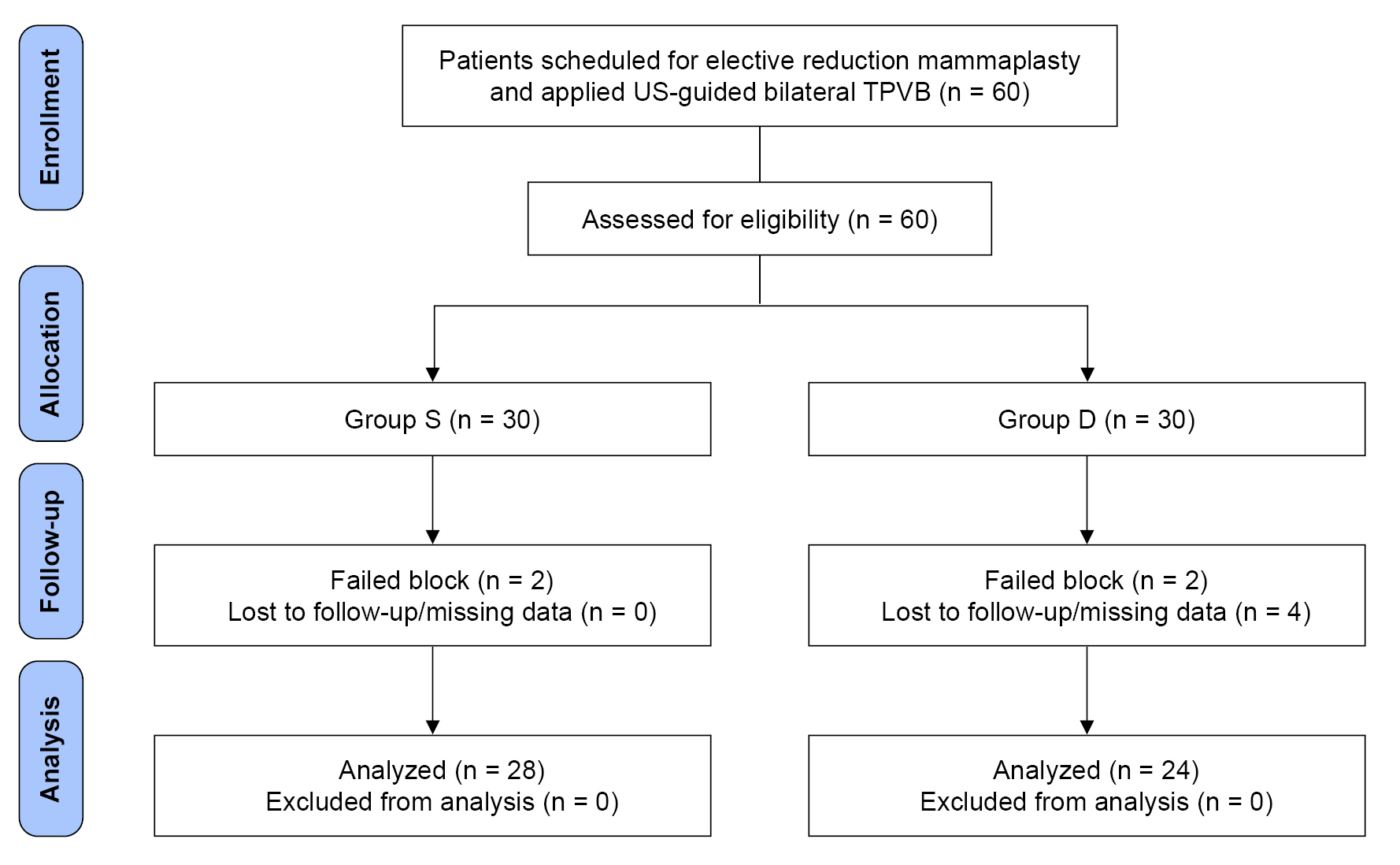
- Background
This study compares the analgesic effects and dermatomal blockade distributions of single and double injection bilateral thoracic paravertebral block (TPVB) techniques in patients undergoing reduction mammaplasty. Methods: After obtaining ethics committee approval, 60 patients scheduled for bilateral reduction mammaplasty were included in the study. Preoperatively, the patients received one of single (Group S: T3–T4) or double (Group D: T2–T3 & T4–T5) injection bilateral TPVBs using bupivacaine 0.375% 20 ml per side. All patients were operated under general anesthesia. The T3–T6 dermatomal blockade distributions on the midclavicular line were followed by pin-prick test for 30 min preoperatively and 48 h postoperatively. All patients received paracetamol 1 g when numeric rating scale (NRS) pain score was ≥ 4, and also tramadol 1 mg/kg when NRS was ≥ 4 again after 1 h. The primary endpoint was NRS pain scores at postoperative 12th h. The secondary endpoints were dermatomal blockade distributions and NRS scores through the postoperative first 48 h, time until first pain and the analgesic consumption on days 1 and 2. Results: Fifty-two patients completed the study. The NRS pain scores at 12th h were similar (right side: P = 0.100, left side: P = 0.096). The remaining NRS scores and other parameters were also comparable within the groups (P ≥ 0.05). Only single injection TPVB application time was shorter (P < 0.001). Conclusions: The single injection TPVB technique provided sufficient dermatomal distribution and analgesic efficacy with the advantages of being faster and less invasive.
Keyword
Figure
Reference
-
1. Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL. Incidence, patient satisfaction, and perceptions of post-surgical pain: results from a US national survey. Curr Med Res Opin. 2014; 30:149–60.2. American Society of Plastic Surgeons. Plastic surgery statistics report. Plastic Surgery Statistics Report [Internet]. 2018. [2021 Oct 25]. Available from https://www.plasticsurgery.org/documents/News/Statistics/2018/plastic-surgery-statistics-full-report-2018.pdf.3. Von Sperling ML, Høimyr H, Finnerup K, Jensen TS, Finnerup NB. Chronic postoperative pain and sensory changes following reduction mammaplasty. Scand J Pain. 2011; 2:57–61.4. Bell RF, Sivertsen A, Mowinkel P, Vindenes H. A bilateral clinical model for the study of acute and chronic pain after breast-reduction surgery. Acta Anaesthesiol Scand. 2001; 45:576–82.
Article5. Spivey TL, Gutowski ED, Zinboonyahgoon N, King TA, Dominici L, Edwards RR, et al. Chronic pain after breast surgery: a prospective, observational study. Ann Surg Oncol. 2018; 25:2917–24.
Article6. Roth RS, Qi J, Hamill JB, Kim HM, Ballard TNS, Pusic AL, et al. Is chronic postsurgical pain surgery-induced? A study of persistent postoperative pain following breast reconstruction. Breast. 2018; 37:119–25.
Article7. Urits I, Lavin C, Patel M, Maganty N, Jacobson X, Ngo AL, et al. Chronic pain following cosmetic breast surgery: a comprehensive review. Pain Ther. 2020; 9:71–82.
Article8. Small C, Laycock H. Acute postoperative pain management. Br J Surg. 2020; 107:e70–e80.
Article9. Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017; 152:691–7.
Article10. Chou R, Gordon DB, De Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016; 17:131–57.
Article11. Jones MR, Hadley GR, Kaye AD, Lirk P, Urman RD. Paravertebral blocks for same-day breast surgery. Curr Pain Headache Rep. 2017; 21:35.
Article12. Kaya FN, Turker G, Mogol EB, Bayraktar S. Thoracic paravertebral block for video-assisted thoracoscopic surgery: single injection versus multiple injections. J Cardiothorac Vasc Anesth. 2012; 26:90–4.
Article13. Kasimahanti R, Arora S, Bhatia N, Singh G. Ultrasound-guided single- vs double-level thoracic paravertebral block for postoperative analgesia in total mastectomy with axillary clearance. J Clin Anesth. 2016; 33:414–21.
Article14. Uppal V, Sondekoppam RV, Sodhi P, Johnston D, Ganapathy S. Single-injection versus multiple-injection technique of ultrasound-guided paravertebral blocks: a randomized controlled study comparing dermatomal spread. Reg Anesth Pain Med. 2017; 42:575–81.15. Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010; 8:18.
Article16. Watkins AC, White PF. Fast-tracking after ambulatory surgery. J Perianesth Nurs. 2001; 16:379–87.
Article17. Vogt A, Stieger DS, Theurillat C, Curatolo M. Single-injection thoracic paravertebral block for postoperative pain treatment after thoracoscopic surgery. Br J Anaesth. 2005; 95:816–21.18. Salviz EA, Sivrikoz N, Ozonur A, Orhan-Sungur M, Savran-Karadeniz M, Altun D, et al. Ultrasound-guided bilateral thoracic paravertebral blocks as an adjunct to general anesthesia in patients undergoing reduction mammaplasty: a historical cohort study. Plast Reconstr Surg. 2017; 139:20e–8e.
Article19. Gardiner S, Rudkin G, Cooter R, Field J, Bond M. Paravertebral blockade for day-case breast augmentation: a randomized clinical trial. Anesth Analg. 2012; 115:1053–9.20. Klein SM, Bergh A, Steele SM, Georgiade GS, Greengrass RA. Thoracic paravertebral block for breast surgery. Anesth Analg. 2000; 90:1402–5.
Article21. Naja MZ, Ziade MF, Lönnqvist PA. Nerve-stimulator guided paravertebral blockade vs. general anaesthesia for breast surgery: a prospective randomized trial. Eur J Anaesthesiol. 2003; 20:897–903.
Article22. Das S, Bhattacharya P, Mandal MC, Mukhopadhyay S, Basu SR, Mandol BK. Multiple-injection thoracic paravertebral block as an alternative to general anaesthesia for elective breast surgeries: a randomised controlled trial. Indian J Anaesth. 2012; 56:27–33.
Article23. Abdallah FW, Morgan PJ, Cil T, McNaught A, Escallon JM, Semple JL, et al. Ultrasound-guided multilevel paravertebral blocks and total intravenous anesthesia improve the quality of recovery after ambulatory breast tumor resection. Anesthesiology. 2014; 120:703–13.
Article24. Glissmeyer C, Johnson W, Sherman B, Glissmeyer M, Garreau J, Johnson N. Effect of paravertebral nerve blocks on narcotic use after mastectomy with reconstruction. Am J Surg. 2015; 209:881–3.
Article25. Şalvız EA, Bingül ES, Güzel M, Karadeniz MS, Turhan Ö, Demirel EE, et al. Comparison of performance characteristics and efficacy of bilateral thoracic paravertebral blocks in obese and non-obese patients undergoing reduction mammaplasty surgery: a historical cohort study. Aesthetic Plast Surg. 2023; 47:1343–52.
Article26. Luyet C, Eichenberger U, Greif R, Vogt A, Szücs Farkas Z, Moriggl B. Ultrasound-guided paravertebral puncture and placement of catheters in human cadavers: an imaging study. Br J Anaesth. 2009; 102:534–9.
Article27. Cowie B, McGlade D, Ivanusic J, Barrington MJ. Ultrasound-guided thoracic paravertebral blockade: a cadaveric study. Anesth Analg. 2010; 110:1735–9.28. Marhofer D, Marhofer P, Kettner SC, Fleischmann E, Prayer D, Schernthaner M, et al. Magnetic resonance imaging analysis of the spread of local anesthetic solution after ultrasound-guided lateral thoracic paravertebral blockade: a volunteer study. Anesthesiology. 2013; 118:1106–12.29. Ben-Ari A, Moreno M, Chelly JE, Bigeleisen PE. Ultrasound-guided paravertebral block using an intercostal approach. Anesth Analg. 2009; 109:1691–4.
Article30. Renes SH, Bruhn J, Gielen MJ, Scheffer GJ, Van Geffen GJ. In-plane ultrasound-guided thoracic paravertebral block: a preliminary report of 36 cases with radiologic confirmation of catheter position. Reg Anesth Pain Med. 2010; 35:212–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Application of Reduction Mammaplasty with Various Methods
- Evaluation of Temperature Elevation on the Ipsilateral Upper Extremity after T2 Paravertebral Block
- Ultrasound Guided Thoracic Paravertebral Space Block for Chronic Intractable Upper Back Pain
- The analgesic efficacy of a single injection of ultrasound-guided retrolaminar paravertebral block for breast surgery: a prospective, randomized, double-blinded study
- A randomized double-blind controlled study comparing erector spinae plane block and thoracic paravertebral block for postoperative analgesia after breast surgery