Anesth Pain Med.
2023 Oct;18(4):357-366. 10.17085/apm.23046.
Feasibility of using red cell distribution width for prediction of postoperative mortality in severe burn patients: an association with acute kidney injury after surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, National Medical Center, Seoul, Korea
- 2Department of Occupational and Environmental Medicine, College of Medicine, Dong-A University, Busan, Korea
- 3Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2550915
- DOI: http://doi.org/10.17085/apm.23046
Abstract
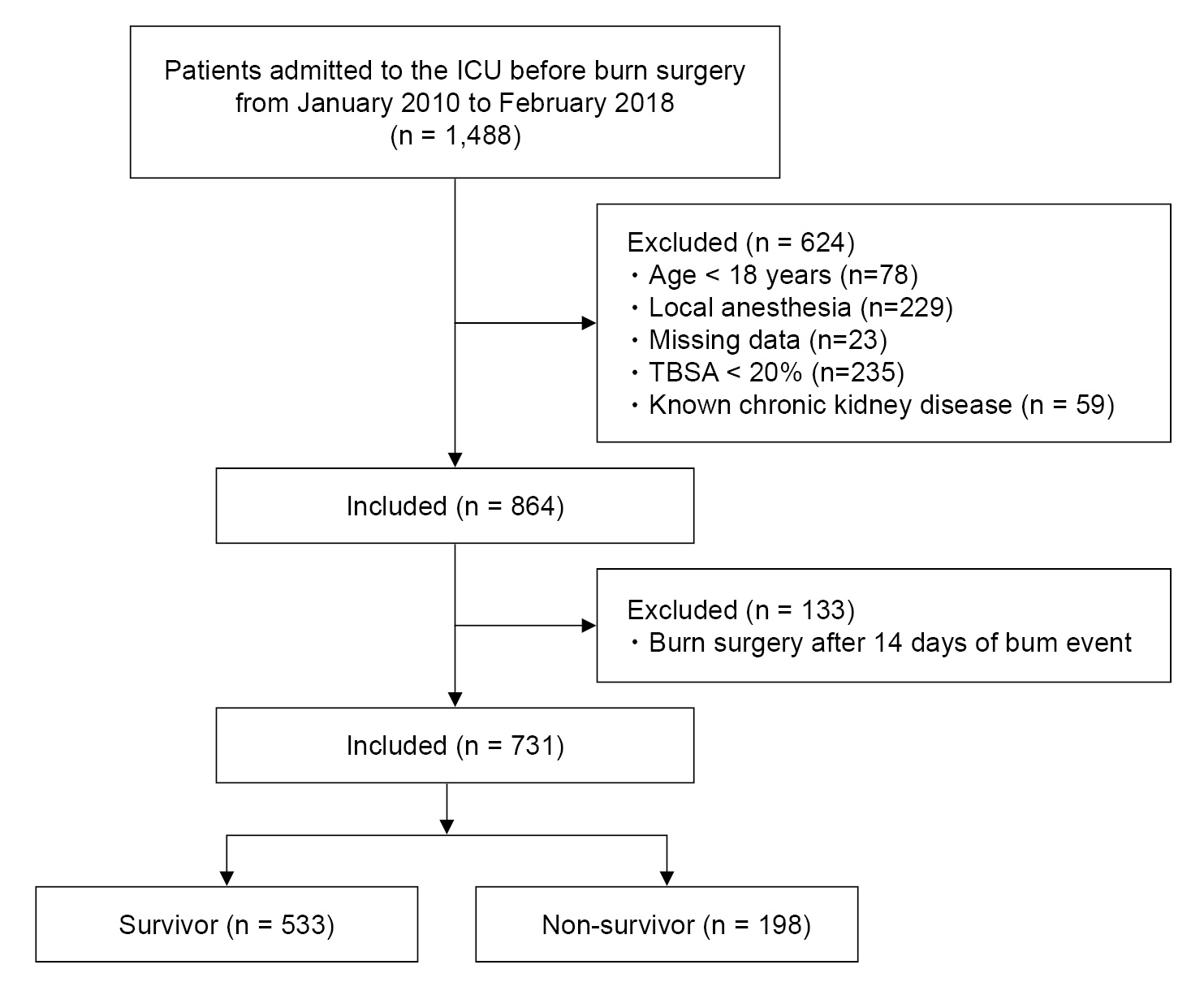
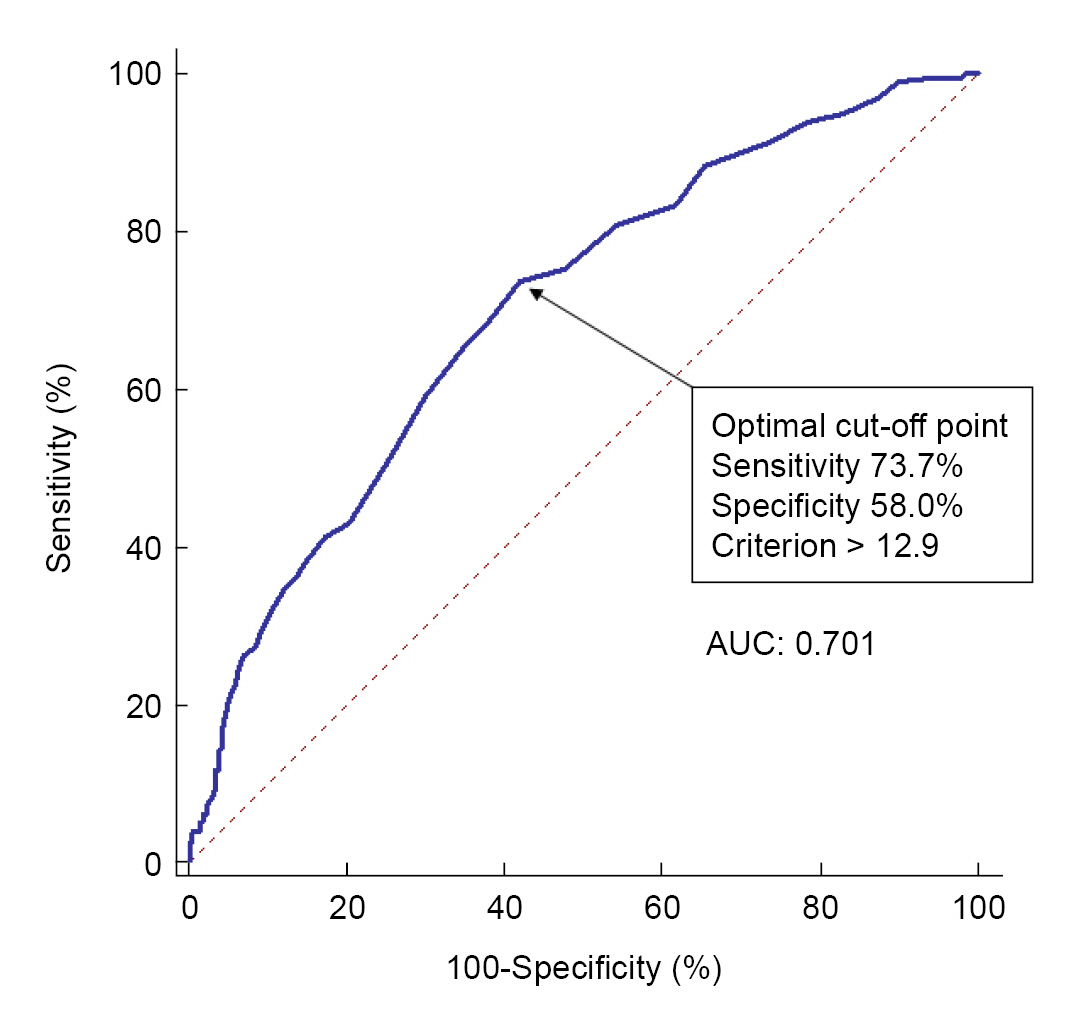
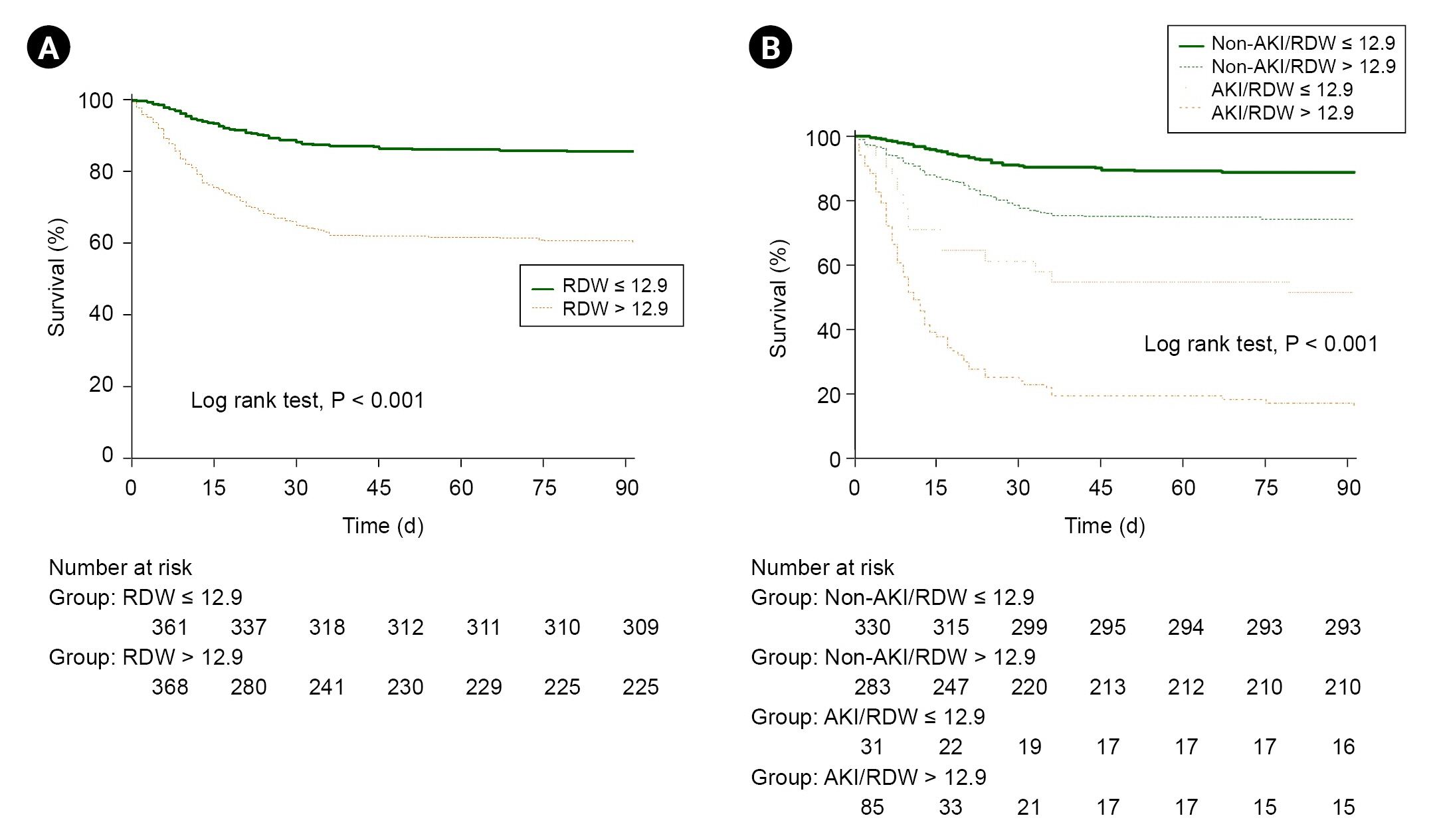
- Background
Severe burns cause pathophysiological processes that result in mortality. A laboratory biomarker, red cell distribution width (RDW), is known as a predictor of mortality in critically-ill patients. We examined the association between RDW and postoperative mortality in severe burn patients. Methods: We retrospectively analyzed medical data of 731 severely burned patients who underwent surgery under general anesthesia. We evaluated whether preoperative RDW value can predict 3-month mortality after burn surgery using receiver operating characteristic (ROC) curve analysis, logistic regression, and Cox proportional-hazards regression analysis. Mortality was also analyzed according to preoperative RDW values and incidence of postoperative acute kidney injury (AKI). Results: The 3-month mortality rate after burn surgery was 27.1% (198/731). The area under the ROC curve of preoperative RDW to predict mortality after burn surgery was 0.701 (95% confidence interval [CI], 0.667–0.734; P < 0.001) with a cut-off point of 12.9. The adjusted hazard ratio in patients with RDW > 12.9 was 1.238 (95% CI, 1.138–1.347; P < 0.001). Subgroup analysis showed that the survival rate was 88.8% for the non-AKI group with RDW ≤ 12.9 and 17.6% for the AKI group with RDW > 12.9. Preoperative RDW was considered an independent risk factor for mortality (odds ratio, 1.679; 95% CI, 1.378– 2.046; P < 0.001). Conclusions: Preoperative RDW may predict 3-month postoperative mortality in patients with severe burns, while preoperative RDW > 12.9 and postoperative AKI may further increase mortality after burn surgery.
Figure
Reference
-
1. Strudwick XL, Cowin AJ. The role of the inflammatory response in burn injury. Hot topics in burn injuries. In : Kartal SP, Bayramgurler D, editors. Adelaide: Intechopen;2017. p. 37–57.2. Kearney L, Francis EC, Clover AJ. New technologies in global burn care - a review of recent advances. Int J Burns Trauma. 2018; 8:77–87.3. Osuka A, Ishihara T, Shimizu K, Shintani A, Ogura H, Ueyama M. Natural kinetics of blood cells following major burn: Impact of early decreases in white blood cells and platelets as prognostic markers of mortality. Burns. 2019; 45:1901–7.
Article4. Salvagno GL, Sanchis-Gomar F, Picanza A, Lippi G. Red blood cell distribution width: A simple parameter with multiple clinical applications. Crit Rev Clin Lab Sci. 2015; 52:86–105.5. Guo J, Qin Q, Hu H, Zhou D, Sun Y, Deng A. Red cell distribution width (RDW) as a prognostic tool in burn patients. Clin Lab. 2016; 62:1973–8.
Article6. Xiao CH, Wan J, Liu H, Qiu L, Wang F, Liu S, et al. Red blood cell distribution width is an independent risk factor in the prediction of acute respiratory distress syndrome after severe burns. Burns. 2019; 45:1158–63.
Article7. Park JH, Cho Y, Shin D, Choi SS. Prediction of mortality after burn surgery in critically Ill burn patients using machine learning models. J Pers Med. 2022; 12:1293.
Article8. Bai C, Huang H, Yao X, Zhu S, Li B, Hang J, et al. Application of flexible bronchoscopy in inhalation lung injury. Diagn Pathol. 2013; 8:174.
Article9. Templeton AJ, Ace O, McNamara MG, Al-Mubarak M, Vera-Badillo FE, Hermanns T, et al. Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2014; 23:1204–12.
Article10. Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014; 106:dju124.
Article11. Valdimarsson H, Mulholland C, Fridriksdottir V, Coleman D. A longitudinal study of leucocyte blood counts and lymphocyte responses in pregnancy: a marked early increase of monocyte-lymphocyte ratio. Clin Exp Immunol. 1983; 53:437–43.12. Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014; 20:6212–22.
Article13. Kellum JA, Lameire N; KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care. 2013; 17:204.
Article14. Nielson CB, Duethman NC, Howard JM, Moncure M, Wood JG. Burns: pathophysiology of systemic complications and current management. J Burn Care Res. 2017; 38:e469–81.15. Schwacha MG. Macrophages and post-burn immune dysfunction. Burns. 2003; 29:1–14.
Article16. Angulo M, Moreno L, Aramendi I, Dos Santos G, Cabrera J, Burghi G. Complete blood count and derived indices: evolution pattern and prognostic value in adult burned patients. J Burn Care Res. 2020; 41:1260–6.
Article17. Yoldas H, Karagoz I, Ogun MN, Velioglu Y, Yildiz I, Bilgi M, et al. Novel mortality markers for critically Ill patients. J Intensive Care Med. 2020; 35:383–5.
Article18. Yan Q, Ertao Z, Zhimei Z, Weigang D, Jianjun P, Jianhui C, et al. Systemic immune-inflammation index (SII): a more promising inflammation-based prognostic marker for patients with synchronic colorectal peritoneal carcinomatosis. J Cancer. 2020; 11:5264–72.
Article19. Fest J, Ruiter R, Ikram MA, Voortman T, Van Eijck CHJ, Stricker BH. Reference values for white blood-cell-based inflammatory markers in the Rotterdam Study: a population-based prospective cohort study. Sci Rep. 2018; 8:10566.
Article20. Tseliou E, Terrovitis JV, Kaldara EE, Ntalianis AS, Repasos E, Katsaros L, et al. Red blood cell distribution width is a significant prognostic marker in advanced heart failure, independent of hemoglobin levels. Hellenic J Cardiol. 2014; 55:457–61.21. Scharte M, Fink MP. Red blood cell physiology in critical illness. Crit Care Med. 2003; 31(12 Suppl):S651–7.
Article22. Allen LA, Felker GM, Mehra MR, Chiong JR, Dunlap SH, Ghali JK, et al. Validation and potential mechanisms of red cell distribution width as a prognostic marker in heart failure. J Card Fail. 2010; 16:230–8.
Article23. Lorente L, Martín MM, Abreu-González P, Solé-Violán J, Ferreres J, Labarta L, et al. Red blood cell distribution width during the first week is associated with severity and mortality in septic patients. PLoS One. 2014; 9:e105436.
Article24. Qiu L, Chen C, Li SJ, Wang C, Guo F, Peszel A, et al. Prognostic values of red blood cell distribution width, platelet count, and red cell distribution width-to-platelet ratio for severe burn injury. Sci Rep. 2017; 7:13720.
Article25. Tang XD, Qiu L, Wang F, Liu S, Lü XW, Chen XL. Diagnostic value of procalcitonin and red blood cell distribution width at admission on the prognosis of patients with severe burns: A retrospective analysis. Int Wound J;2023. doi: 10.1111/iwj.14263. [Epub ahead of print].26. Lai H, Cai Z, Wu S, Zhang W, Chen J, Wu G. An increase in admission RDW value is associated with excess short-term mortality rates in patients with severe burns. Appl Biochem Biotechnol. 2023; 195:3217–28.
Article27. Folkestad T, Brurberg KG, Nordhuus KM, Tveiten CK, Guttormsen AB, Os I, et al. Acute kidney injury in burn patients admitted to the intensive care unit: a systematic review and meta-analysis. Crit Care. 2020; 24:2.
Article28. Colpaert K, Hoste EA. Acute kidney injury in burns: a story of volume and inflammation. Crit Care. 2008; 12:192.
Article29. Wang B, Lu H, Gong Y, Ying B, Cheng B. The association between red blood cell distribution width and mortality in critically Ill patients with acute kidney injury. Biomed Res Int. 2018; 2018:9658216.
Article30. Zhu J, Zeng C, Zhang L, Shu S, Liu Y, Chen G, et al. Red blood cell distribution width and neutrophil-to-lymphocyte ratio in predicting adverse outcomes of acute kidney injury in hospitalized patients. Kidney Dis (Basel). 2020; 6:371–81.
Article31. Ogura A, Tsurumi A, Que YA, Almpani M, Zheng H, Tompkins RG, et al. Associations between clinical characteristics and the development of multiple organ failure after severe burns in adult patients. Burns. 2019; 45:1775–82.
Article32. Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective estimates of the probability of death from burn injuries. N Engl J Med. 1998; 338:362–6.
Article33. Covington DS, Wainwright DJ, Parks DH. Prognostic indicators in the elderly patient with burns. J Burn Care Rehabil. 1996; 17:222–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Initial Red Cell Distribution Width for Predicting Mortality in Severe Trauma Patients Admitted to the Emergency Department
- Red cell distribution width predicts incident dipstick albuminuria in Korean adults without chronic kidney disease
- A Case of Severe Acute Hepatitis A Complicated with Pure Red Cell Aplasia
- Serum Lactate, Creatinine and Urine Output: Early Predictors of Mortality after Initial Fluid Resuscitation in Severe Burn Patients
- A new hematologic predictor of major adverse events after cardiac surgery: red cell distribution width to lymphocyte ratio