Ann Clin Microbiol.
2023 Dec;26(4):89-97. 10.5145/ACM.2023.26.4.89.
Clinical manifestations, diagnosis, and antimicrobial resistance of group A streptococci infections
- Affiliations
-
- 1Institute of Medical Science, Gyeongsang National University, Jinju, Korea
- 2Department of Laboratory Medicine, Gyeongsang National University College of Medicine, Jinju, Korea
- 3Department of Laboratory Medicine, Gyeongsang National University Changwon Hospital, Changwon, Korea
- KMID: 2550660
- DOI: http://doi.org/10.5145/ACM.2023.26.4.89
Abstract
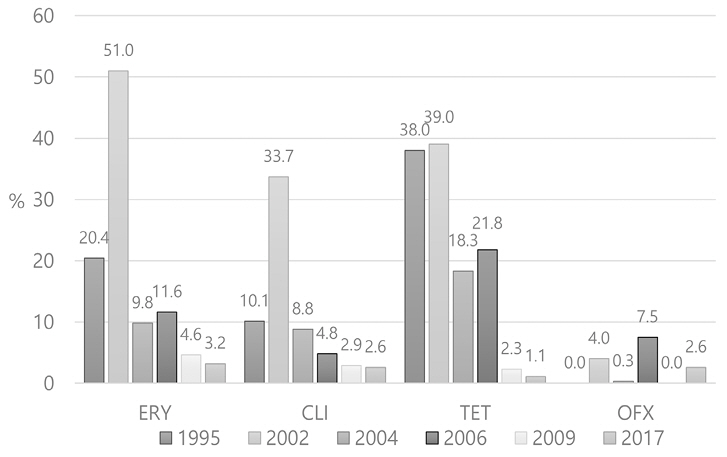
- Group A streptococci (GAS) cause diverse diseases ranging from mild to severe illnesses, and the global burden of GAS infections is enormous. Serological typing has been replaced by emm genotyping for the epidemiological study of GAS. Acute bacterial pharyngitis is a common illness, which requires either throat culture or rapid Ag test for diagnosis. Moreover, molecular point-of-care tests have been introduced owing to their higher sensitivity. Optimal diagnosis of bacterial pharyngitis is necessary for the adequate use of antibiotics. Although antimicrobial resistance (AMR) to erythromycin or clindamycin does not seem serious in Korea, it is very high in China, being reported at over 90%. Antibiotic surveillance and relevant education are necessary for primary clinical physicians and pediatricians. It is necessary to monitor AMR and develop a system for reporting the appearance of highly virulent diseases, such as necrotizing fasciitis or streptococcal toxic-shock syndrome, to the government authority.
Keyword
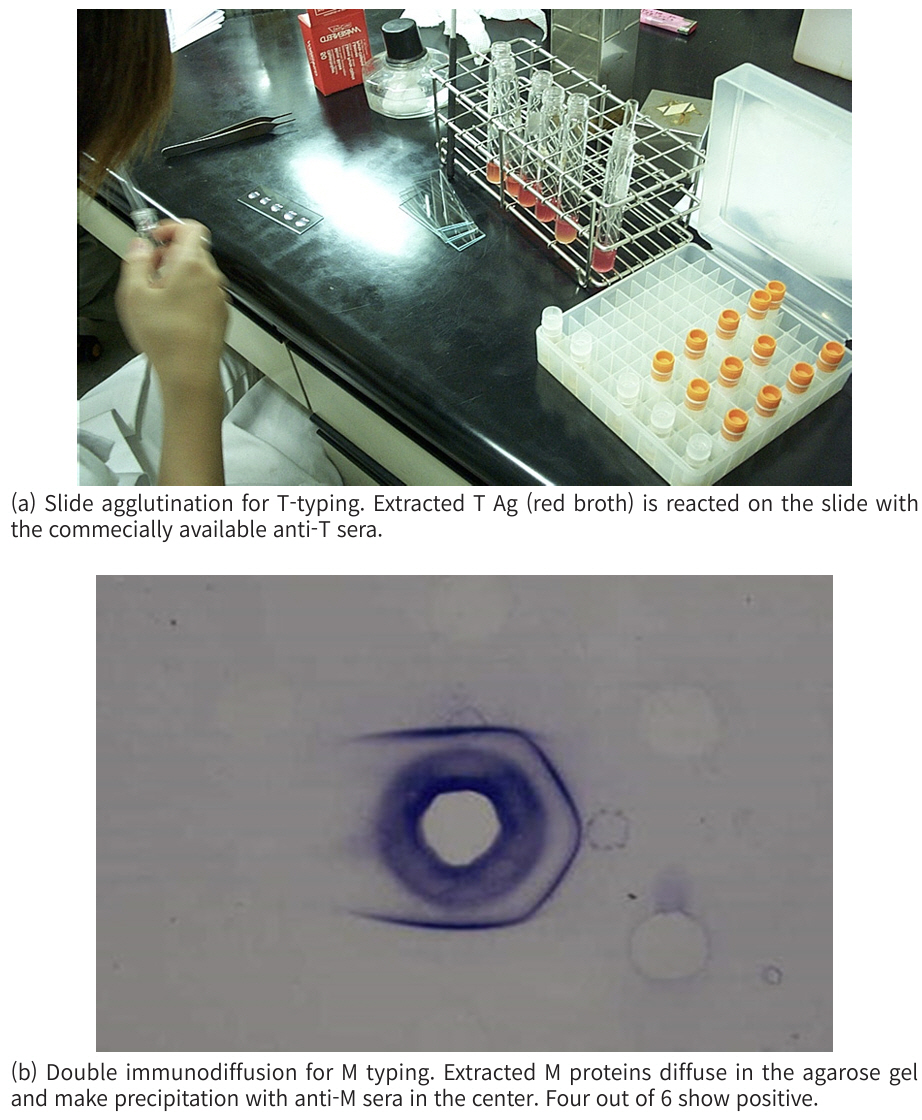
Figure
Reference
-
1. Watkins DA, Johnson CO, Colquhoun SM, Karthikeyan G, Beaton A, Bukhman G, et al. Global, regional, and national burden of rheumatic heart disease, 1990–2015. N Engl J Med 2017;377;713-22. .2. Lv M, Jiang S, Liao D, Lin Z, Chen H, Zhang J. Global burden of rheumatic heart disease and its association with socioeconomic development status, 1990–2019. Eur J Prev Cardiol 2022;29:1425-34. .3. Luo R, Sickler J, Vahidnia F, Lee YC, Frogner B, Thompson M. Diagnosis and management of group A streptococcal pharyngitis in the United States, 2011–2015. BMC Infect Dis 2019; 19:1-9. .4. Kim J, Park J, Kim BY, Kim DS. The trend of acute respiratory tract infections and antibiotic prescription rates in outpatient settings using health insurance data. Korean J Physiol Pharmacol 2017;27:186-94. .5. Kalra MG, Higgins KE, Perez ED. Common questions about streptococcal pharyngitis. Am Fam Physician 2016;94:24-31. .6. Kim S, Lee S, Park H, Kim S. Predominance of emm4 and antibiotic resistance of Streptococcus pyogenes in acute pharyngitis in a southern region of Korea. Int J Med Microbiol 2019;68:1053-8. .7. Johnson DR, Kaplan EL, VanGheem A, Facklam RR, Beall B. Characterization of group A streptococci (Streptococcus pyogenes): correlation of M-protein and emm-gene type with T-protein agglutination pattern and serum opacity factor. J Med Microbiol 2006;55:157-64. .8. Kim S and Lee NY. Epidemiological usefulness of anti-opacity factor antibody screening in schoolchildren. J Clin Microbiol 2001;39:1316-8. .9. Brouwer S, Rivera-Hernandez T, Curren BF, Harbison-Price N, De Oliveira DM, Jespersen MG, et al. Pathogenesis, epidemiology and control of Group A Streptococcus infection. Nat Rev Microbiol 2023;21:431-47. .10. Pastural É, McNeil SA, MacKinnon-Cameron D, Ye L, Langley JM, Stewart R, et al. Safety and immunogenicity of a 30-valent M protein-based group a streptococcal vaccine in healthy adult volunteers: a randomized, controlled phase I study. Vaccine 2020;38:1384-92. .11. Dale JB, Penfound TA, Chiang EY, Walton WJ. New 30-valent M protein-based vaccine evokes cross-opsonic antibodies against non-vaccine serotypes of group A streptococci. Vaccine 2011;29:8175-8. .12. Hosier DM, Craenen JM, Teske DW, Wheller JJ. Resurgence of acute rheumatic fever. Am J Dis Child 1987;141:730-3. .13. Rush CM, Govan BL, Sikder S, Williams NL, Ketheesan N. Animal models to investigate the pathogenesis of rheumatic heart disease. Front Pediatr 2014;2:116. .14. Bruun T, Kittang B, De Hoog B, Aardal S, Flaatten H, Langeland N, et al. Necrotizing soft tissue infections caused by Streptococcus pyogenes and Streptococcus dysgalactiae subsp. equisimilis of groups C and G in western Norway. Clin Microbiol Infect 2013;19:E545-50. .15. Ikebe T, Tominaga K, Shima T, Okuno R, Kubota H, Ogata K, et al. Increased prevalence of group A streptococcus isolates in streptococcal toxic shock syndrome cases in Japan from 2010 to 2012. Epidemiol Infect 2015;143:864-72. .16. Schmitz M, Roux X, Huttner B, Pugin J. Streptococcal toxic shock syndrome in the intensive care unit. Ann Intensive Care 2018;8:1-10.17. Cordery R, Purba AK, Begum L, Mills E, Mosavie M, Vieira A, et al. Frequency of transmission, asymptomatic shedding, and airborne spread of Streptococcus pyogenes in schoolchildren exposed to scarlet fever: a prospective, longitudinal, multicohort, molecular epidemiological, contact-tracing study in England, UK. Lancet Microbe 2022;3:e366-75. .18. Kim SJ. Distribution and upper limit of normal antistreptolysin O concentrations of school. Korean J Infect Dis 1997;233-8. .19. Bennett J, Moreland NJ, Williamson DA, Carapetis J, Crane J, Whitcombe AL, et al. Comparison of group A streptococcal titres in healthy children and those with pharyngitis and skin infections. J Infect 2022;84:24-30. .20. Lacey JA, Marcato AJ, Chisholm RH, Campbell PT, Zachreson C, Price DJ, et al. Evaluating the role of asymptomatic throat carriage of Streptococcus pyogenes in impetigo transmission in remote Aboriginal communities in Northern Territory, Australia: a retrospective genomic analysis. Lancet Microbe 2023;4:E524-33. .21. Keeley AJ, Groves D, Armitage EP, Senghore E, Jagne YJ, Sallah HJ, et al. Streptococcus pyogenes colonization in children aged 24–59 months in the Gambia: impact of live attenuated influenza vaccine and associated serological responses. J Infect Dis 2023;228:957-65. .22. Kim SJ. Optimal site of throat swab for the isolation of beta-hemolytic streptococci. J Korean Med Sci 1993;8:453-7. .23. Pires R, Rolo D, Mato R, Feio de Almeida J, Johansson C, Henriques-Normark B, et al. Resistance to bacitracin in Streptococcus pyogenes from oropharyngeal colonization and noninvasive infections in Portugal was caused by two clones of distinct virulence genotypes. FEMS Microbiol Lett 2009;296:235-40. .24. Berry GJ, Miller CR, Prats MM, Marquez C, Oladipo OO, Loeffelholz MJ, et al. Comparison of the Alere i Strep A test and the BD Veritor system in the detection of group A streptococcus and the hypothetical impact of results on antibiotic utilization. J Clin Microbiol 2018;56:e01310-7. .25. Cohen JF, Bertille N, Cohen R, Chalumeau M. Rapid antigen detection test for group A streptococcus in children with pharyngitis. Cochrane Database Syst Rev 2016;7:CD010502. .26. Close RM, Sutcliffe CG, Galdun P, Reid A, Askew MR, Davidson AM, et al. Point-of-care molecular diagnostics for the detection of group A streptococcus in non-invasive skin and soft tissue infections: a validation study. Diagn Microbiol Infect Dis 2022;103:115729. .27. May L, Sickler J, Robbins EM, Tang S, Chugh K, Tran N. The impact of point-of-care polymerase chain reaction testing on prescribing practices in primary care for management of Strep A: a retrospective before–after study. Open Forum Infect Dis 2022;9:ofac147. .28. Ebell MH, Smith MA, Barry HC, Ives K, Carey M. Does this patient have strep throat? JAMA 2000;284:2912-8. .29. Jo SA, Ma SH, Kim S. Diagnostic impact of clinical manifestations of group A Streptococcal pharyngitis. Infect Chemother 2021;53:553.30. Kim SJ, Chung MA, Chung HJ, Kim YJ, Maeng KY. Distribution and upper limit of normal antistreptolysin O concentrations according to age. Korean J Infect Dis 1998;392-6. .31. McMillan DJ, Drèze PA, Vu T, Bessen DE, Guglielmini J, Steer AC, et al. Updated model of group A streptococcus M proteins based on a comprehensive worldwide study. Clin Microbiol Infect 2013;19:E222-9. .32. Rafei R, Iaali RA, Osman M, Dabboussi F, Hamze M. A global snapshot on the prevalent macrolide-resistant emm types of Group A streptococcus worldwide, their phenotypes and their resistance marker genotypes during the last two decades: a systematic review. Infect Genet Evol 2022;99:105258. .33. Choi JH, Yang NR, Lee WJ, Lee H, Choi EH, Lee HJ. Distribution of emm types among group A streptococcus isolates from children in Korea. Diagn Microbiol Infect Dis 2015;82:26-31. .34. Kim HN, Kim J, Jang WS, Nam J, Lim CS. Performance evaluation of three rapid antigen tests for the diagnosis of group A Streptococci. BMJ Open 2019;9:e025438. .35. Cho YN, Park SE, Cho EY, Cho HK, Park JY, Kang HM, et al. Distribution of emm genotypes in group A streptococcus isolates of Korean children from 2012 to 2019. J Microbiol Immunol Infect 2022;55:671-7. .36. Li Y, Rivers J, Mathis S, Li Z, McGee L, Chochua S, et al. Continued increase of erythromycin nonsusceptibility and clindamycin nonsusceptibility among invasive group A streptococci driven by genomic clusters, United States, 2018–2019. Clin Infect Dis 2023;76:e1266-9. .37. Wajima T, Morozumi M, Chiba N, Shouji M, Iwata S, Sakata H, et al. Associations of macrolide and fluoroquinolone resistance with molecular typing in Streptococcus pyogenes from invasive infections, 2010–2012. Int J Antimicrob Agents 2013;42:447-9. .38. Lu B, Fang Y, Fan Y, Chen X, Wang J, Zeng J, et al. High prevalence of macrolide-resistance and molecular characterization of Streptococcus pyogenes isolates circulating in China from 2009 to 2016. Front Microbiol 2017;8:1052. .39. Li H, Zhou L, Zhao Y, Ma L, Liu X, Hu J. Molecular epidemiology and antimicrobial resistance of group a streptococcus recovered from patients in Beijing, China. BMC Infect Dis 2020;20:1-9. .40. Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 2012;55:e86-102. .41. McGuire E, Li A, Collin SM, Decraene V, Cook M, Padfield S, et al. Time to negative throat culture following initiation of antibiotics for pharyngeal group A streptococcus: a systematic review and meta-analysis up to October 2021 to inform public health control measures. Euro Surveill 2023;28:2200573. .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial Resistance and Treatment Update of Skin and Soft Tissue Infections
- Antimicrobial Susceptibility of beta-emolytic Streptococci Isolated during the Period of 1999
- Antimicrobial Resistance and Serotypes in the Clinical Isolates of Group B Streptococci
- Species-Specific Difference in Antimicrobial Susceptibility Among Viridans Group Streptococci
- Survey of Antimicrobial Resistance of Pharyngeal alpha-Hemolytic Streptococci among School Children