Ann Clin Microbiol.
2023 Sep;26(3):75-82. 10.5145/ACM.2023.26.3.5.
A survey of physicians’ perceptions of diagnostic tests for Clostridioides difficile infection
- Affiliations
-
- 1Department of Laboratory Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 2Ewha Education and Research Center for Infection, Ewha Womans University Medical Center, Seoul, Korea
- 3Department of Internal Medicine, Inje University College of Medicine, Seoul, Korea
- 4Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Korea
- 6Department of Laboratory Medicine, Inje University College of Medicine, Seoul,c
- KMID: 2550658
- DOI: http://doi.org/10.5145/ACM.2023.26.3.5
Abstract
- Background
This study aimed to investigate perceptions of Clostridioides difficile infection (CDI) diagnostic tests among physicians who prescribe CDI diagnostic tests as part of providing direct patient care.
Methods
In August 2018, we provided a 12-question survey of gastroenterologists (the most common referral source for CDI testing) to 35 medical institutions in Korea, asking them about their perceptions of CDI diagnosis and testing.
Results
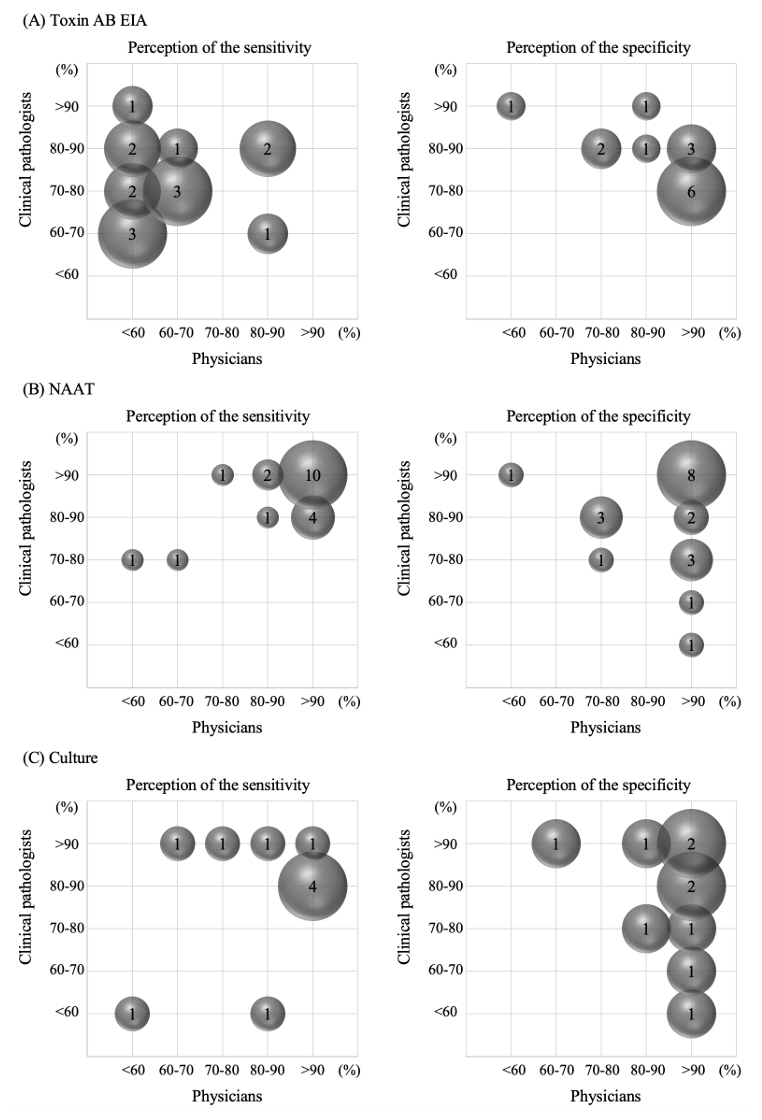
A comparison of the perceptions of physicians and clinical pathologists (CPs) found that physicians had a lower perceived sensitivity of the toxin AB enzyme immunoassay test. For nucleic acid amplification tests, physicians exhibited a perception of higher assay sensitivity and specificity than CPs. The specificity of culture tests was generally perceived as high by physicians, whereas CPs regarding expressed mixed opinions. All but one physician and one CPs found the algorithmic test useful. Concerning the CDI isolation criteria, physicians commenced patient isolation by concurrently assessing both test results and clinical symptoms, rather than exclusively relying upon test results. Among CPs, 84.6% said they could rely on symptoms to determine when to release a patient from isolation, while 46.2% of physicians said they would rely on test results.
Conclusion
This study provides useful information on the status of laboratory diagnosis of CDI in Korea and what needs to be improved, which will help to standardize and improve laboratory diagnosis of CDI in Korea.
Figure
Reference
-
1. Leffler DA and Lamont JT. Clostridium difficile infection. N Engl J Med 2015;372:1539-48. .2. Bagdasarian N, Rao K, Malani PN. Diagnosis and treatment of Clostridium difficile in adults: a systematic review. JAMA 2015;313:398-408. .3. Biswas R, Dudani H, Lakhera P, Pal AK, Kurbah P, Bhatia D, et al. Challenges and future solutions for detection of Clostridioides difficile in adults. Ann Gastroenterol 2023;36:369-77. .4. Crobach MJT, Baktash A, Duszenko N, Kuijper EJ. Diagnostic guidance for C. difficile infections. Adv Exp Med Biol 2018;1050:27-44. .5. Chung HS, Park JS, Shin BM, Yoo HM, Kim H, Cho J, et al. Nationwide survey for current status of laboratory diagnosis of Clostridioides difficile Infection in Korea. J Korean Med Sci 2022;37:e38. .6. Chung HS, Park JS, Shin BM. Laboratory diagnosis of Clostridium difficile infection in Korea: the first national survey. Ann Lab Med 2019;39:317-21. .7. Crobach MJT, Planche T, Eckert C, Barbut F, Terveer EM, Dekkers OM, et al. European Society of Clinical Microbiology and Infectious Diseases: update of the diagnostic guidance document for Clostridium difficile infection. Clin Microbiol Infect 2016;22:S63-81. .8. McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis 2018;66:987-94. .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Stewardship on the Extra-Analytical Phase to Secure Quality Assurance of Diagnostic Tests for Clostridioides difficile Infection
- Which is the Preferred Regimen for Non-Severe Clostridioides difficile Infection in Korea, Vancomycin or Metronidazole?
- Management of Clostridioides difficile infection in patients with inflammatory bowel disease
- Laboratory diagnosis of Clostridioides difficile infection: guidelines and status of practice in Korea
- Clostridioides Infection in Patients with Inflammatory Bowel Disease