J Korean Neurosurg Soc.
2024 Jan;67(1):94-102. 10.3340/jkns.2023.0118.
Prediction Model for Unfavorable Outcome in Spontaneous Intracerebral Hemorrhage Based on Machine Learning
- Affiliations
-
- 1Department of Neurosurgery, Qingdao Hospital, University of Health and Rehabilitation Sciences (Qingdao Municipal Hospital), Qingdao, China
- 2Department of Anesthesia Operating Room, Qingdao Hospital, University of Health and Rehabilitation Sciences (Qingdao Municipal Hospital), Qingdao, China
- KMID: 2550463
- DOI: http://doi.org/10.3340/jkns.2023.0118
Abstract
Objective
: The spontaneous intracerebral hemorrhage (ICH) remains a significant cause of mortality and morbidity throughout the world. The purpose of this retrospective study is to develop multiple models for predicting ICH outcomes using machine learning (ML).
Methods
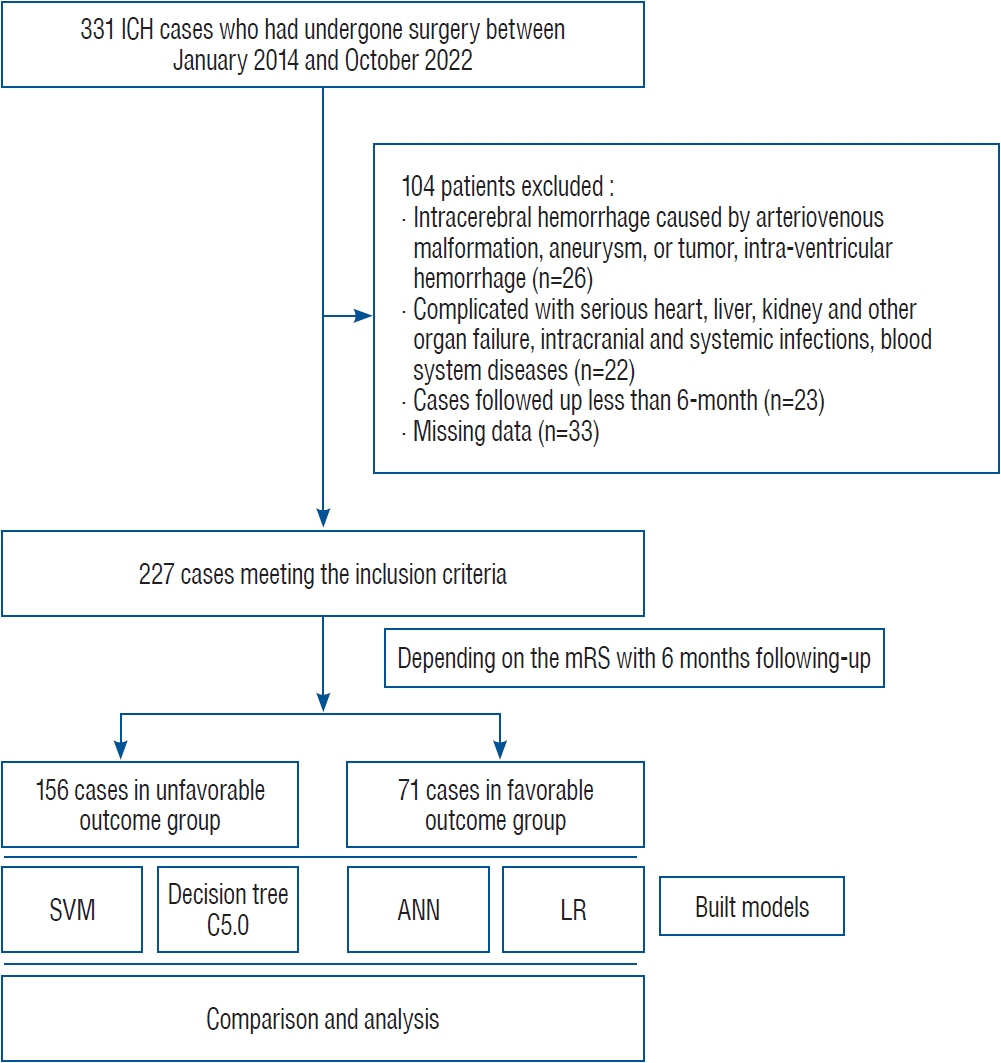
: Between January 2014 and October 2021, we included ICH patients identified by computed tomography or magnetic resonance imaging and treated with surgery. At the 6-month check-up, outcomes were assessed using the modified Rankin Scale. In this study, four ML models, including Support Vector Machine (SVM), Decision Tree C5.0, Artificial Neural Network, Logistic Regression were used to build ICH prediction models. In order to evaluate the reliability and the ML models, we calculated the area under the receiver operating characteristic curve (AUC), specificity, sensitivity, accuracy, positive likelihood ratio (PLR), negative likelihood ratio (NLR), diagnostic odds ratio (DOR).
Results
: We identified 71 patients who had favorable outcomes and 156 who had unfavorable outcomes. The results showed that the SVM model achieved the best comprehensive prediction efficiency. For the SVM model, the AUC, accuracy, specificity, sensitivity, PLR, NLR, and DOR were 0.91, 0.92, 0.92, 0.93, 11.63, 0.076, and 153.03, respectively. For the SVM model, we found the importance value of time to operating room (TOR) was higher significantly than other variables.
Conclusion
: The analysis of clinical reliability showed that the SVM model achieved the best comprehensive prediction efficiency and the importance value of TOR was higher significantly than other variables.
Keyword
Figure
Reference
-
References
1. Alabi RO, Youssef O, Pirinen M, Elmusrati M, Mäkitie AA, Leivo I, et al. Machine learning in oral squamous cell carcinoma: current status, clinical concerns and prospects for future-A systematic review. Artif Intell Med. 115:102060. 2021.
Article2. Alghamdi NS, Zakariah M, Hoang VT, Elahi MM. Neurogenerative disease diagnosis in cepstral domain using MFCC with deep learning. Comput Math Methods Med. 2022:4364186. 2022.
Article3. Cheung RT, Zou LY. Use of the original, modified, or new intracerebral hemorrhage score to predict mortality and morbidity after intracerebral hemorrhage. Stroke. 34:1717–1722. 2003.
Article4. Choi RY, Coyner AS, Kalpathy-Cramer J, Chiang MF, Campbell JP. Introduction to machine learning, neural networks, and deep learning. Transl Vis Sci Technol. 9:14. 2020.5. Ding W, Gu Z, Song D, Liu J, Zheng G, Tu C. Development and validation of the hypertensive intracerebral hemorrhage prognosis models. Medicine (Baltimore). 97:e12446. 2018.
Article6. Garg R, Biller J. Recent advances in spontaneous intracerebral hemorrhage. F1000Res. 8:F1000. 2019.
Article7. Hanley DF, Thompson RE, Rosenblum M, Yenokyan G, Lane K, McBee N, et al. Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): a randomised, controlled, open-label, blinded endpoint phase 3 trial. Lancet. 393:1021–1032. 2019.8. Hersh EH, Gologorsky Y, Chartrain AG, Mocco J, Kellner CP. Minimally invasive surgery for intracerebral hemorrhage. Curr Neurol Neurosci Rep. 18:34. 2018.
Article9. Heschl S, Bernard S, Andrew E, Smith K. Characteristics of paediatric patients with altered conscious state attended by road ambulances in a metropolitan area - an 8 year observational study. Australas Emerg Care. 23:142–146. 2020.
Article10. Hostettler IC, Seiffge DJ, Werring DJ. Intracerebral hemorrhage: an update on diagnosis and treatment. Expert Rev Neurother. 19:679–694. 2019.
Article11. Jussen D, Marticorena S, Sandow N, Vajkoczy P, Horn P. Ultra-early decompressive hemicraniectomy in aneurysmal intracerebral hemorrhage: a retrospective observational study. Minerva Anestesiol. 81:398–404. 2015.12. Kellner CP, Schupper AJ, Mocco J. Surgical evacuation of intracerebral hemorrhage: the potential importance of timing. Stroke. 52:3391–3398. 2021.13. Liu G, Wu J, Dang C, Tan S, Peng K, Guo Y, et al. Machine learning for predicting motor improvement after acute subcortical infarction using baseline whole brain volumes. Neurorehabil Neural Repair. 36:38–48. 2022.
Article14. Liu M, Wang Z, Meng X, Zhou Y, Hou X, Li L, et al. Predictive nomogram for unfavorable outcome of spontaneous intracerebral hemorrhage. World Neurosurg. 164:e1111–e1122. 2022.
Article15. Luzzi S, Elia A, Del Maestro M, Morotti A, Elbabaa SK, Cavallini A, et al. Indication, timing, and surgical treatment of spontaneous intracerebral hemorrhage: systematic review and proposal of a management algorithm. World Neurosurg. 124:e769–e778. 2019.
Article16. Maldaner N, Zeitlberger AM, Sosnova M, Goldberg J, Fung C, Bervini D, et al. Development of a complication- and treatment-aware prediction model for favorable functional outcome in aneurysmal subarachnoid hemorrhage based on machine learning. Neurosurgery. 88:E150–E157. 2021.
Article17. Matheny ME, Resnic FS, Arora N, Ohno-Machado L. Effects of SVM parameter optimization on discrimination and calibration for postprocedural PCI mortality. J Biomed Inform. 40:688–697. 2007.
Article18. Nemoto M, Masuda H, Sakaeyama Y, Okonogi S, Node Y, Ueda K, et al. Clinical characteristics of subarachnoid hemorrhage with an intracerebral hematoma and prognostic factors. J Stroke Cerebrovasc Dis. 27:1160–1166. 2018.
Article19. Polster SP, Carrión-Penagos J, Lyne SB, Gregson BA, Cao Y, Thompson RE, et al. Intracerebral hemorrhage volume reduction and timing of intervention versus functional benefit and survival in the MISTIE III and STICH trials. Neurosurgery. 88:961–970. 2021.
Article20. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 46:3020–3035. 2015.
Article21. Ruiz-Sandoval JL, Aceves-Montoya J, Chiquete E, López-Valencia G, Lara-López A, Sánchez-González M, et al. Hospital arrival and functional outcome after intracerebral hemorrhage. Rev Invest Clin. 74:51–60. 2022.
Article22. Schlunk F, Chang Y, Ayres A, Battey T, Vashkevich A, Raffeld M, et al. Blood pressure burden and outcome in warfarin-related intracerebral hemorrhage. Int J Stroke. 11:898–909. 2016.
Article23. Tozlu C, Edwards D, Boes A, Labar D, Tsagaris KZ, Silverstein J, et al. Machine learning methods predict individual upper-limb motor impairment following therapy in chronic stroke. Neurorehabil Neural Repair. 34:428–439. 2020.
Article24. Wang D, Wang W, Wang A, Zhao X. Association of severity and prognosis with elevated homocysteine levels in patients with intracerebral hemorrhage. Front Neurol. 11:571585. 2020.
Article25. Wang YF, Wu JS, Mao Y, Chen XC, Zhou LF, Zhang Y. The optimal timewindow for surgical treatment of spontaneous intracerebral hemorrhage: result of prospective randomized controlled trial of 500 cases. Acta Neurochir Suppl. 105:141–145. 2008.
Article26. Zhang Y, Xia R, Lv M, Li Z, Jin L, Chen X, et al. Machine-learning algorithm-based prediction of diagnostic gene biomarkers related to immune infiltration in patients with chronic obstructive pulmonary disease. Front Immunol. 13:740513. 2022.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Machine Learning vs. Statistical Model for Prediction Modelling: Application in Medical Imaging Research
- An improved machine learning model for calculation of intraocular lens power during cataract surgery in Republic of Korea: development
- The Application of Machine Learning in Predicting Outcome of Cryotherapy and Immunotherapy for Wart Removal
- Machine learning-based 2-year risk prediction tool in immunoglobulin A nephropathy
- Statistics and Deep Belief Network-Based Cardiovascular Risk Prediction