J Korean Neurosurg Soc.
2024 Jan;67(1):84-93. 10.3340/jkns.2023.0082.
Trend of Intensive Care Unit Admission in Neurology-Neurosurgery Adult Patients in South Korea : A Nationwide Population-Based Cohort Study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Interdepartment of Critical Care Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Anesthesiology and Pain Medicine, College of Medicine, Seoul National University, Seoul, Korea
- KMID: 2550462
- DOI: http://doi.org/10.3340/jkns.2023.0082
Abstract
Objective
: We aimed to examine trends in critically ill neurology-neurosurgery (NNS) patients who were admitted to the intensive care unit (ICU) in South Korea and identify risk factors for in-hospital mortality after ICU admission in NNS patients.
Methods
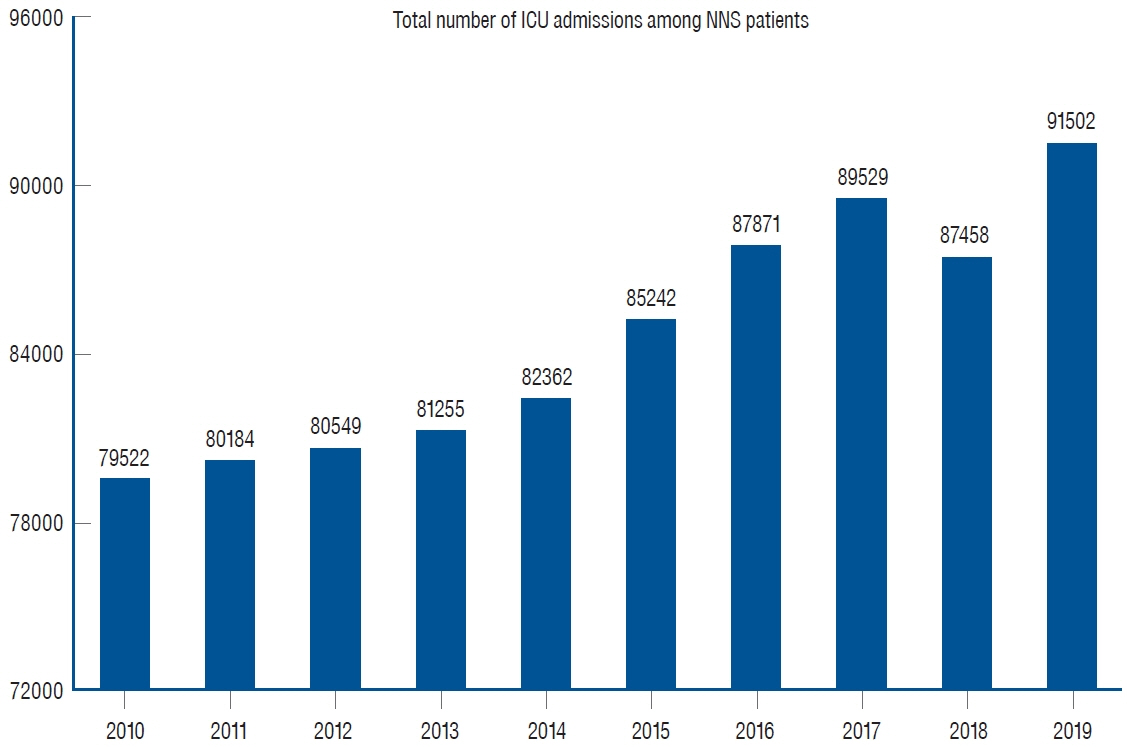
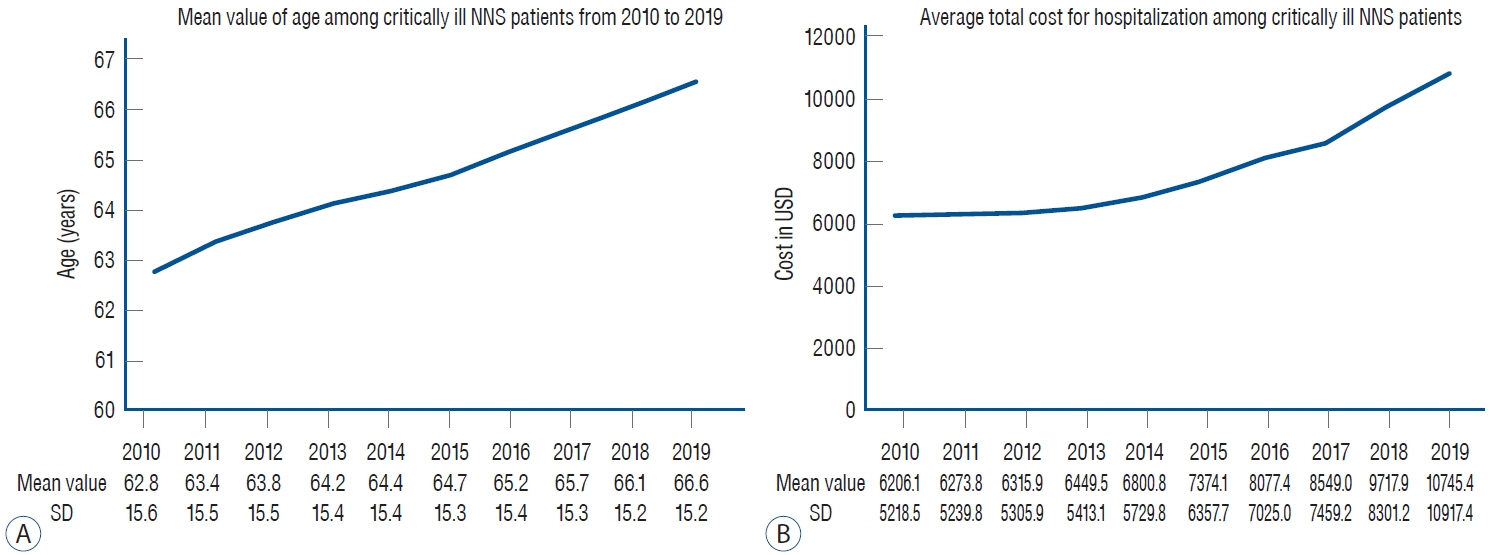
: This nationwide population-based retrospective cohort study enrolled adult NNS adult patients admitted to the ICU from 2010 to 2019 extracted from the National Health Insurance Service in South Korea. The critically ill NNS patients were defined as those whose main admission departments were neurology or neurosurgery at ICU admission. The number of ICU admission, age, and total cost for hospitalization from 2010 to 2019 in critically ill NNS patients were examined as trend information. Moreover, multivariable logistic regression modeling was used to identify risk factors for in-hospital mortality among critically ill NNS patients.
Results
: We included 845474 ICU admission cases for 679376 critically ill NNS patients in South Korea between January 1, 2010 to December 31, 2019. The total number of ICU admissions among NNS patients was 79522 in 2010, which increased to 91502 in 2019. The mean age rose from 62.8 years (standard deviation [SD], 15.6) in 2010 to 66.6 years (SD, 15.2) in 2019, and the average total cost for hospitalization per each patient consistently increased from 6206.1 USD (SD, 5218.5) in 2010 to 10745.4 USD (SD, 10917.4) in 2019. In-hospital mortality occurred in 75455 patients (8.9%). Risk factors strongly associated with increased in-hospital mortality were the usage of mechanical ventilator (adjusted odds ratio [aOR], 19.83; 95% confidence interval [CI], 19.42–20.26; p<0.001), extracorporeal membrane oxygenation (aOR, 3.49; 95% CI, 2.42–5.02; p<0.001), and continuous renal replacement therapy (aOR, 6.47; 95% CI, 6.02–6.96; p<0.001). In addition, direct admission to ICU from the emergency room (aOR, 1.38; 95% CI, 1.36–1.41; p<0.001) and brain cancer as the main diagnosis (aOR, 1.30; 95% CI, 1.22–1.39; p<0.001) are also potential risk factors for increased in-hospital mortality.
Conclusion
: In South Korea, the number of ICU admissions increased among critically ill NNS patients from 2010 to 2019. The average age and total costs for hospitalization also increased. Some potential risk factors are found to increase in-hospital mortality among critically ill NNS patients.
Keyword
Figure
Reference
-
References
1. Algahtani R, Merenda A. Multimorbidity and critical care neurosurgery: minimizing major perioperative cardiopulmonary complications. Neurocrit Care. 34:1047–1061. 2021.
Article2. Baek JY, Lee E, Jung HW, Jang IY. Geriatrics fact sheet in Korea 2021. Ann Geriatr Med Res. 25:65–71. 2021.
Article3. Beer R, Pfausler B, Schmutzhard E. Infectious intracranial complications in the neuro-ICU patient population. Curr Opin Crit Care. 16:117–122. 2010.
Article4. Damian MS, Ben-Shlomo Y, Howard R, Bellotti T, Harrison D, Griggs K, et al. The effect of secular trends and specialist neurocritical care on mortality for patients with intracerebral haemorrhage, myasthenia gravis and Guillain-Barré syndrome admitted to critical care : an analysis of the Intensive Care National Audit & Research Centre (ICNARC) national United Kingdom database. Intensive Care Med. 39:1405–1412. 2013.
Article5. Dao Trong P, Olivares A, El Damaty A, Unterberg A. Adverse events in neurosurgery: a comprehensive single-center analysis of a prospectively compiled database. Acta Neurochir (Wien). 165:585–593. 2023.
Article6. Depauw PRAM, Groen RJM, Van Loon J, Peul WC, Malbrain MLNG, De Waele JJ. The significance of intra-abdominal pressure in neurosurgery and neurological diseases: a narrative review and a conceptual proposal. Acta Neurochir (Wien). 161:855–864. 2019.
Article7. Farmanfarma KK, Mohammadian M, Shahabinia Z, Hassanipour S, Salehiniya H. Brain cancer in the world: an epidemiological review. WCRJ. 6:e1356. 2019.8. Jo KW, Kim H, Yoo DS, Hyun DK, Cheong JH, Park HK, et al. Current status of neurosurgical and neurointensive care units in Korea : a brief report on nationwide survey results. J Korean Neurosurg Soc. 63:519–531. 2020.
Article9. Kay HF, Chotai S, Wick JB, Stonko DP, McGirt MJ, Devin CJ. Preoperative and surgical factors associated with postoperative intensive care unit admission following operative treatment for degenerative lumbar spine disease. Eur Spine J. 25:843–849. 2016.
Article10. Kouchit Y, Morand L, Martis N. Mortality and its risk factors in critically ill patients with connective tissue diseases: a meta-analysis. Eur J Intern Med. 98:83–92. 2022.
Article11. Lamba N, Wen PY, Aizer AA. Epidemiology of brain metastases and leptomeningeal disease. Neuro Oncol. 23:1447–1456. 2021.
Article12. Lee HJ, Son YJ. Factors associated with in-hospital mortality after continuous renal replacement therapy for critically ill patients: a systematic review and meta-analysis. Int J Environ Res Public Health. 17:8781. 2020.
Article13. Malaiyandi D, Shutter L. Neurocritical care past, present, and future. Crit Care Clin. 39:xiii–xiv. 2023.
Article14. Miller KD, Ostrom QT, Kruchko C, Patil N, Tihan T, Cioffi G, et al. Brain and other central nervous system tumor statistics, 2021. CA Cancer J Clin. 71:381–406. 2021.
Article15. Moheet AM, Livesay SL, Abdelhak T, Bleck TP, Human T, Karanjia N, et al. Standards for neurologic critical care units: a statement for healthcare professionals from the Neurocritical Care Society. Neurocrit Care. 29:145–160. 2018.
Article16. Mucksavage J, Kim KS. Challenges in ICU care: the patient with Parkinson's disease. Crit Care Nurs Q. 43:205–215. 2020.17. Paul G, Paul BS, Gautam PL, Singh G, Kaushal S. Parkinson's disease in intensive care unit: an observational study of frequencies, causes, and outcomes. Ann Indian Acad Neurol. 22:79–83. 2019.
Article18. Pham X, Ray J, Neto AS, Laing J, Perucca P, Kwan P, et al. Association of neurocritical care services with mortality and functional outcomes for adults with brain injury: a systematic review and meta-analysis. JAMA Neurol. 79:1049–1058. 2022.
Article19. Prust ML, Mbonde A, Rubinos C, Shrestha GS, Komolafe M, Saylor D, et al. Providing neurocritical care in resource-limited settings: challenges and opportunities. Neurocrit Care. 37:583–592. 2022.
Article20. Raj R, Bendel S, Reinikainen M, Hoppu S, Laitio R, Ala-Kokko T, et al. Costs, outcome and cost-effectiveness of neurocritical care: a multicenter observational study. Crit Care. 22:225. 2018.
Article21. Ropper AH. Neurological intensive care. Ann Neurol. 32:564–569. 1992.
Article22. Sanaiha Y, Bailey K, Downey P, Seo YJ, Aguayo E, Dobaria V, et al. Trends in mortality and resource utilization for extracorporeal membrane oxygenation in the United States: 2008-2014. Surgery. 165:381–388. 2019.
Article23. Sondag L, Schreuder FHBM, Boogaarts HD, Rovers MM, Vandertop WP, Dammers R, et al. Neurosurgical intervention for supratentorial intracerebral hemorrhage. Ann Neurol. 88:239–250. 2020.
Article24. Suarez JI. Outcome in neurocritical care: advances in monitoring and treatment and effect of a specialized neurocritical care team. Crit Care Med. 34(9 Suppl):S232–S238. 2006.
Article25. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted inhospital mortality. J Clin Epidemiol. 57:1288–1294. 2004.
Article26. Venkatasubba Rao CP, Suarez JI, Martin RH, Bauza C, Georgiadis A, Calvillo E, et al. Global survey of outcomes of neurocritical care patients: analysis of the PRINCE study part 2. Neurocrit Care. 32:88–103. 2020.
Article27. Vincent JL, Marshall JC, Namendys-Silva SA, François B, Martin-Loeches I, Lipman J, et al. Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit. Lancet Respir Med. 2:380–386. 2014.
Article28. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 370:1453–1457. 2007.
Article29. Wahba AJ, Cromwell DA, Hutchinson PJ, Mathew RK, Phillips N. Patterns and outcomes of neurosurgery in England over a five-year period: a national retrospective cohort study. Int J Surg. 99:106256. 2022.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prior Lifestyle and Survival Outcomes After Intensive Care Unit Admission
- Changes in the Characteristics and Long-term Mortality Rates of Intensive Care Unit Patients from 2003 to 2010: A Nationwide Population-Based Cohort Study Performed in the Republic of Korea
- Impact of Socioeconomic Status on 30-Day and 1-Year Mortalities after Intensive Care Unit Admission in South Korea: A Retrospective Cohort Study
- Can the intensivists predict the outcomes of critically ill patients on the appropriateness of intensive care unit admission for limited intensive care unit resources ?
- Discrepancy between the Demand and Supply of Intensive Care Unit Beds in South Korea from 2011 to 2019: A Cross-Sectional Analysis