Acute Crit Care.
2018 Aug;33(3):135-145. 10.4266/acc.2018.00164.
Changes in the Characteristics and Long-term Mortality Rates of Intensive Care Unit Patients from 2003 to 2010: A Nationwide Population-Based Cohort Study Performed in the Republic of Korea
- Affiliations
-
- 1Department of Internal Medicine, Kangwon National University Hospital, Chuncheon, Korea.
- 2Department of Internal Medicine, Kangwon National University School of Medicine, Chuncheon, Korea. medfman@gmail.com
- 3Division of Allergy and Clinical Immunology, Kangwon National University School of Medicine, Chuncheon, Korea.
- 4Department of Statistics, Kangwon National University, Chuncheon, Korea.
- 5Department of Neurology, Kangwon National University School of Medicine, Chuncheon, Korea.
- KMID: 2436325
- DOI: http://doi.org/10.4266/acc.2018.00164
Abstract
- BACKGROUND
There are few studies on intensive care unit (ICU) patients in the Republic of Korea. We analyzed the characteristics and mortality changes of all ICU patients over the last 8 years.
METHODS
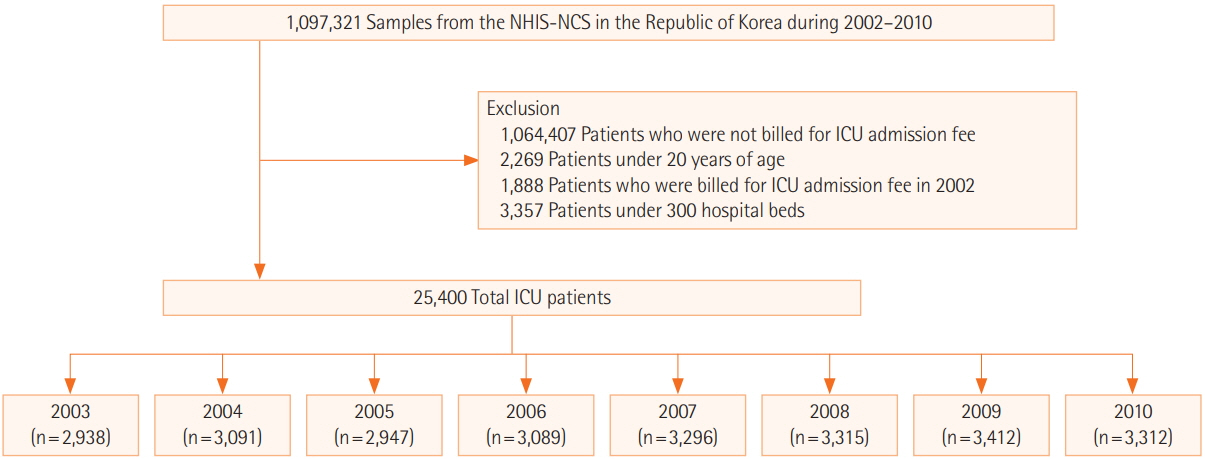
This study used the cohort of the National Health Insurance Corporation, which provides medical care to all residents of the Republic of Korea. The cohort consists of patients aged 20 years or older between 2003 and 2010 with a history of ICU admission. We analyzed changes in sex, age, household income, number of hospital beds, emergency admissions, and reasons for admission using the Cochran-Armitage trend test. The adjusted hazard ratios (HRs) of mortality according to these variables and year of admission were calculated by Cox proportional hazards regression.
RESULTS
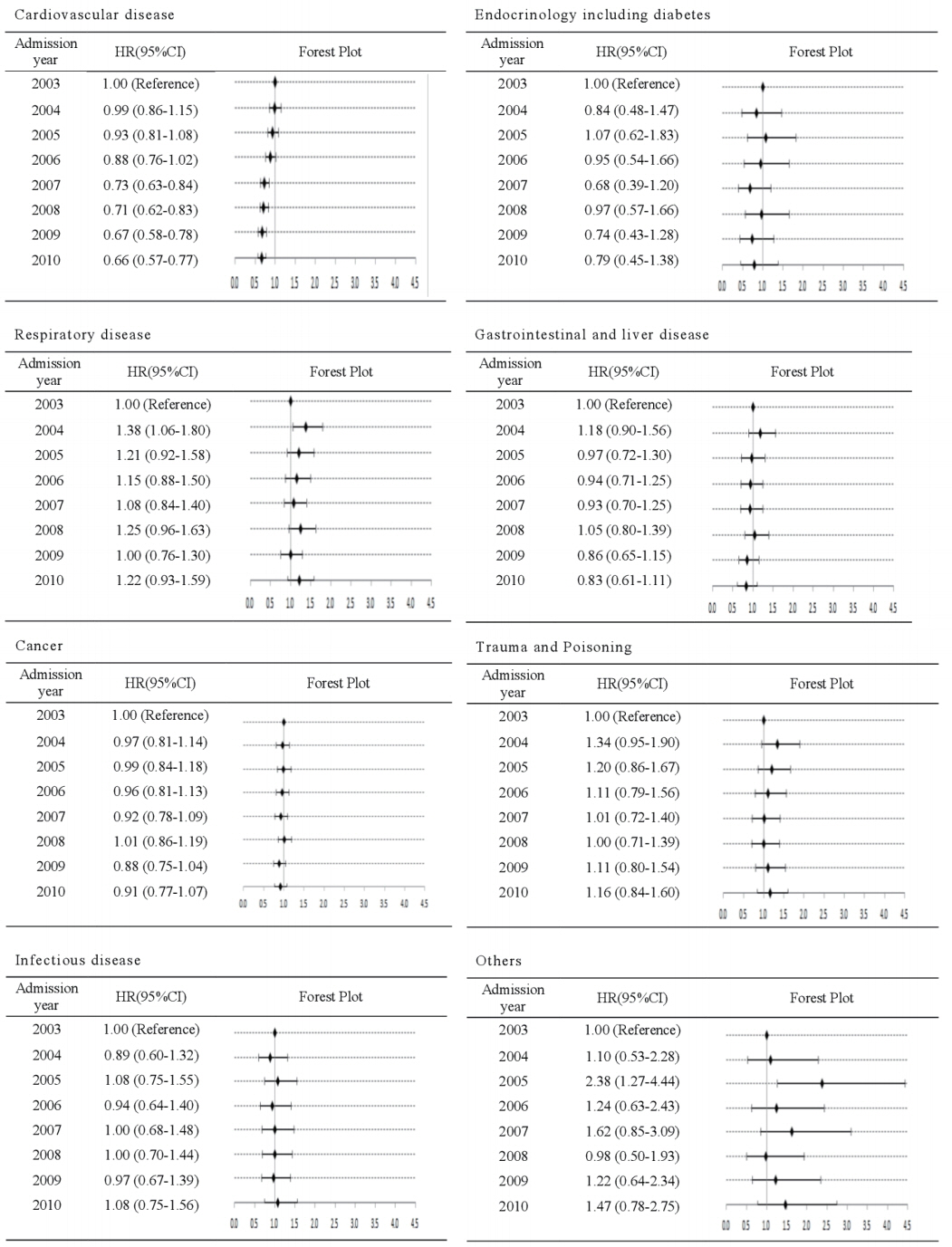
The proportion of patients aged ≥70 years increased over that period, as did their average age (by 3.6 years). During the 8-year study period, the 3-year mortality rate was 32.91%-35.83%. The overall mortality was higher in males and older patients, in those with a lower household income and higher Charlson Comorbidity Index (CCI) score, those admitted to a hospital with a smaller number of beds, and those admitted via the emergency room. There was no significant change in crude mortality rate over the 8-year study period; however, the adjusted HR showed a decreasing trend.
CONCLUSIONS
Patients admitted to the ICU were older and had higher CCI score. Nevertheless, there was a temporal trend toward a decrease in the HR of long-term mortality.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Critical Care Research Using “Big Data”: A Reality in the Near Future
Kwangha Lee
Acute Crit Care. 2018;33(4):269-270. doi: 10.4266/acc.2018.00346.Long-term mortality of patients discharged from the hospital after successful critical care in the ICU in Korea: a retrospective observational study in a single tertiary care teaching hospital
Se Hee Na, Cheung Soo Shin, Gwan Ho Kim, Jae Hoon Kim, Jong Seok Lee
Korean J Anesthesiol. 2020;73(2):129-136. doi: 10.4097/kja.d.18.00275.
Reference
-
1. Bagshaw SM, Webb SA, Delaney A, George C, Pilcher D, Hart GK, et al. Very old patients admitted to intensive care in Australia and New Zealand: a multi-centre cohort analysis. Crit Care. 2009; 13:R45.
Article2. Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017; 389:1323–35.
Article3. Milbrandt EB, Kersten A, Rahim MT, Dremsizov TT, Clermont G, Cooper LM, et al. Growth of intensive care unit resource use and its estimated cost in Medicare. Crit Care Med. 2008; 36:2504–10.
Article4. Molina JA, Seow E, Heng BH, Chong WF, Ho B. Outcomes of direct and indirect medical intensive care unit admissions from the emergency department of an acute care hospital: a retrospective cohort study. BMJ Open. 2014; 4:e005553.
Article5. Halpern NA, Pastores SM. Critical care medicine in the United States 2000-2005: an analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010; 38:65–71.
Article6. Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985-2000: an analysis of bed numbers, use, and costs. Crit Care Med. 2004; 32:1254–9.
Article7. Wallace DJ, Angus DC, Seymour CW, Barnato AE, Kahn JM. Critical care bed growth in the United States: a comparison of regional and national trends. Am J Respir Crit Care Med. 2015; 191:410–6.
Article8. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHISNSC), South Korea. Int J Epidemiol. 2017; 46:e15.
Article9. Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014; 311:1308–16.
Article10. Zimmerman JE, Kramer AA, Knaus WA. Changes in hospital mortality for United States intensive care unit admissions from 1988 to 2012. Crit Care. 2013; 17:R81.
Article11. Mahmood K, Eldeirawi K, Wahidi MM. Association of gender with outcomes in critically ill patients. Crit Care. 2012; 16:R92.
Article12. Fuchs L, Chronaki CE, Park S, Novack V, Baumfeld Y, Scott D, et al. ICU admission characteristics and mortality rates among elderly and very elderly patients. Intensive Care Med. 2012; 38:1654–61.
Article13. Schnegelsberg A, Mackenhauer J, Nibro HL, Dreyer P, Koch K, Kirkegaard H. Impact of socioeconomic status on mortality and unplanned readmission in septic intensive care unit patients. Acta Anaesthesiol Scand. 2016; 60:465–75.
Article14. Christensen S, Johansen MB, Christiansen CF, Jensen R, Lemeshow S. Comparison of Charlson comorbidity index with SAPS and APACHE scores for prediction of mortality following intensive care. Clin Epidemiol. 2011; 3:203–11.
Article15. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–83.
Article16. Sjoding MW, Prescott HC, Wunsch H, Iwashyna TJ, Cooke CR. Longitudinal changes in ICU admissions among elderly patients in the United States. Crit Care Med. 2016; 44:1353–60.
Article17. Koch K, Nørgaard M, Schønheyder HC, Thomsen RW, Søgaard M; Danish Collaborative Bacteremia Network. Effect of socioeconomic status on mortality after bacteremia in workingage patients: a Danish population-based cohort study. PLoS One. 2013; 8:e70082.
Article18. Hutchings A, Raine R, Brady A, Wildman M, Rowan K. Socioeconomic status and outcome from intensive care in England and Wales. Med Care. 2004; 42:943–51.
Article19. Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993; 270:2957–63.
Article20. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–29.21. Lemeshow S, Teres D, Klar J, Avrunin JS, Gehlbach SH, Rapoport J. Mortality Probability Models (MPM II) based on an international cohort of intensive care unit patients. JAMA. 1993; 270:2478–86.
Article22. Ho KM, Knuiman M, Finn J, Webb SA. Estimating long-term survival of critically ill patients: the PREDICT model. PLoS One. 2008; 3:e3226.
Article23. Johnston JA, Wagner DP, Timmons S, Welsh D, Tsevat J, Render ML. Impact of different measures of comorbid disease on predicted mortality of intensive care unit patients. Med Care. 2002; 40:929–40.
Article24. Jhun HJ, Kim H, Cho SI. Time trend and age-period-cohort effects on acute myocardial infarction mortality in Korean adults from 1988 to 2007. J Korean Med Sci. 2011; 26:637–41.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prior Lifestyle and Survival Outcomes After Intensive Care Unit Admission
- A Comprehensive Analysis of 5-Year Outcomes in Patients with Cancer Admitted to Intensive Care Units
- Impact of Intensivist and Nursing Staff on Critically Ill Patient Mortality: A Retrospective Analysis of the Korean NHIS Cohort Data, 2011–2015
- Trend of Intensive Care Unit Admission in Neurology-Neurosurgery Adult Patients in South Korea : A Nationwide Population-Based Cohort Study
- Short-term and long-term outcomes of critically ill patients with solid malignancy: a retrospective cohort study