J Korean Neurosurg Soc.
2024 Jan;67(1):60-72. 10.3340/jkns.2023.0128.
A Single-Center Experience of Robotic-Assisted Spine Surgery in Korea : Analysis of Screw Accuracy, Potential Risk Factor of Screw Malposition and Learning Curve
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Busan, Korea
- 2Department of Neurosurgery, School of Medicine, Pusan National University, Yangsan, Korea
- 3Department of Neurosurgery, Spine and Spinal Cord Institute, Severance Hospital, Seoul, Korea
- 4Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2550460
- DOI: http://doi.org/10.3340/jkns.2023.0128
Abstract
Objective
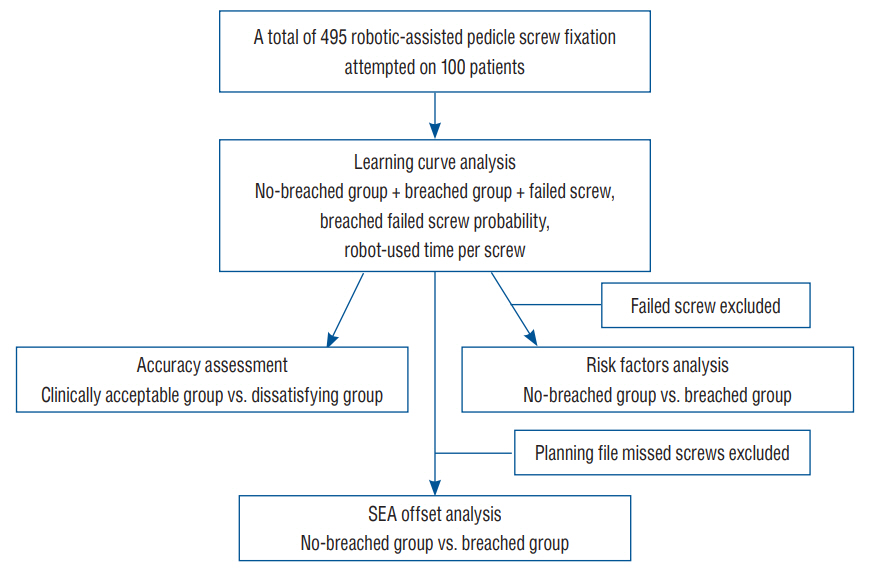
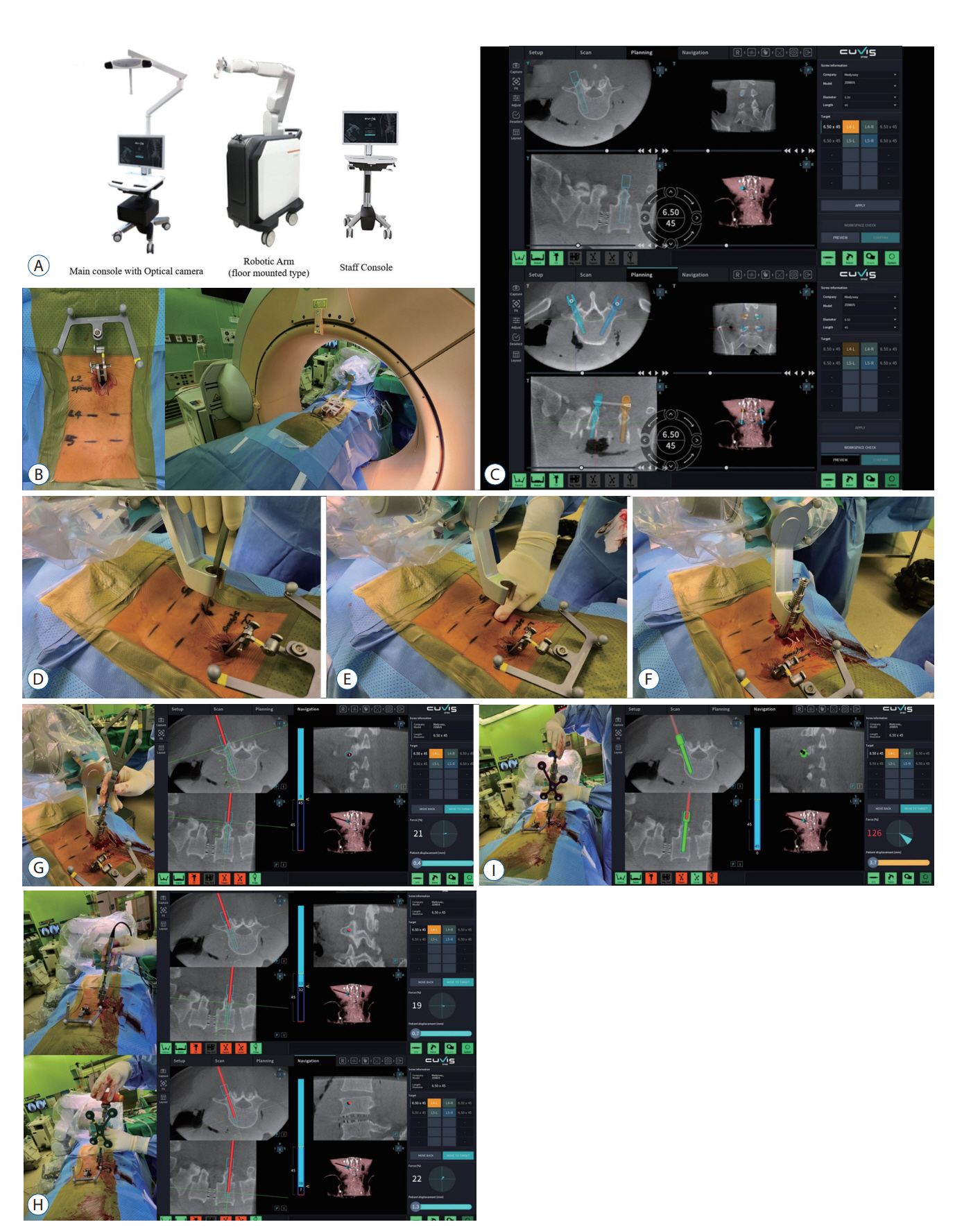
: Recently, robotic-assisted spine surgery (RASS) has been considered a minimally invasive and relatively accurate method. In total, 495 robotic-assisted pedicle screw fixation (RAPSF) procedures were attempted on 100 patients during a 14-month period. The current study aimed to analyze the accuracy, potential risk factors, and learning curve of RAPSF.
Methods
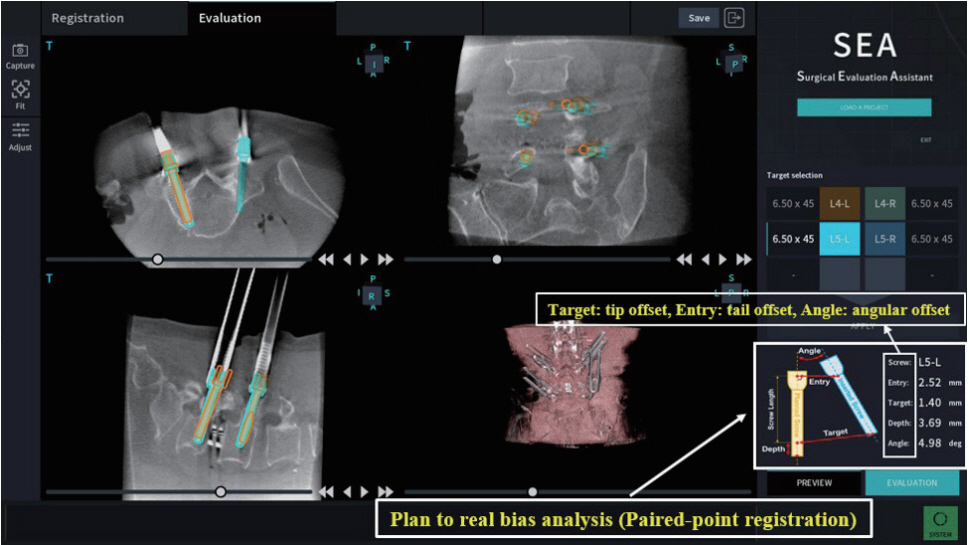
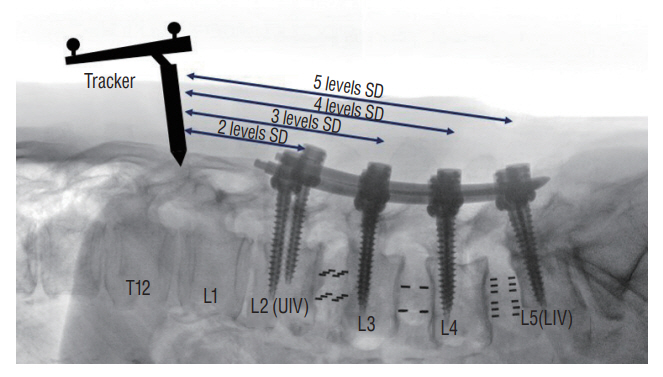
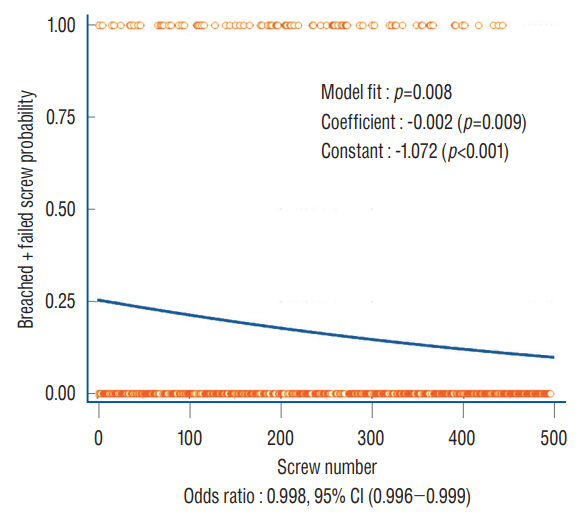
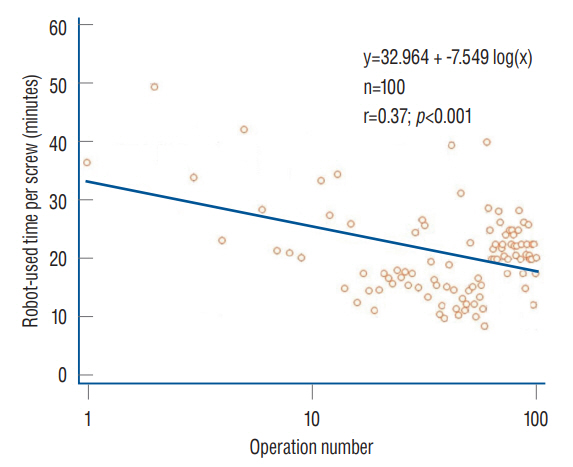
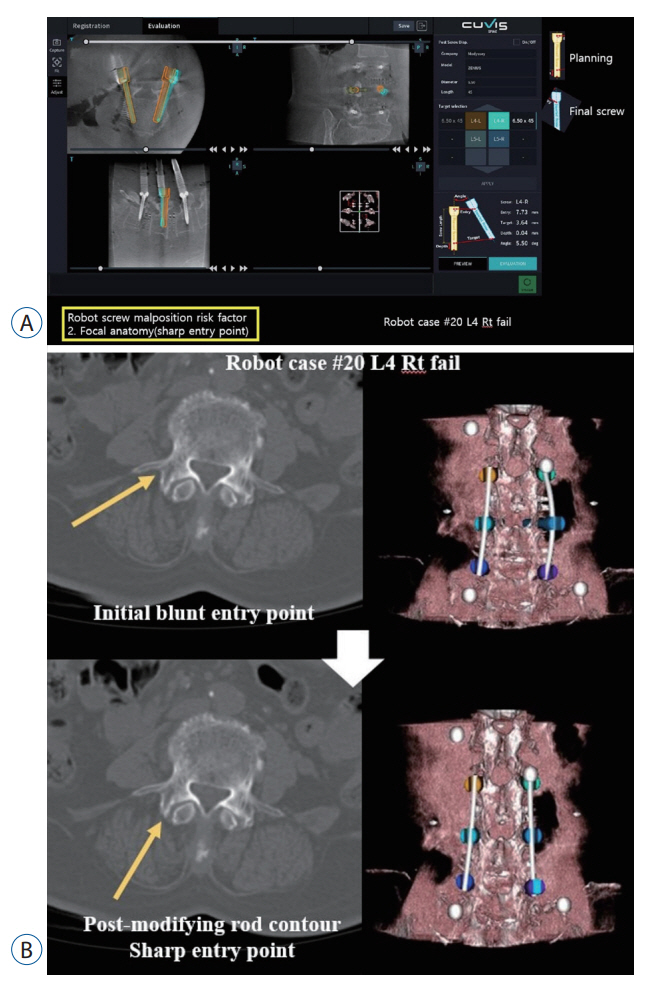
: This retrospective study evaluated the position of RAPSF using the Gertzbein and Robbins scale (GRS). The accuracy was analyzed using the ratio of the clinically acceptable group (GRS grades A and B), the dissatisfying group (GRS grades C, D, and E), and the Surgical Evaluation Assistant program. The RAPSF was divided into the no-breached group (GRS grade A) and breached group (GRS grades B, C, D, and E), and the potential risk factors of RAPSF were evaluated. The learning curve was analyzed by changes in robot-used time per screw and the occurrence tendency of breached and failed screws according to case accumulation.
Results
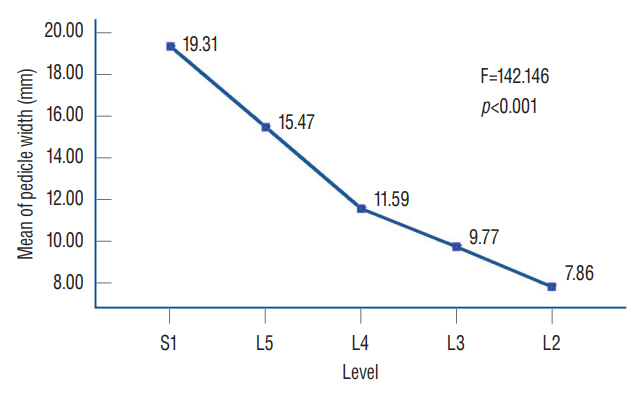
: The clinically acceptable group in RAPSF was 98.12%. In the analysis using the Surgical Evaluation Assistant program, the tip offset was 2.37±1.89 mm, the tail offset was 3.09±1.90 mm, and the angular offset was 3.72°±2.72°. In the analysis of potential risk factors, the difference in screw fixation level (p=0.009) and segmental distance between the tracker and the instrumented level (p=0.001) between the no-breached and breached group were statistically significant, but not for the other factors. The mean difference between the no-breach and breach groups was statistically significant in terms of pedicle width (p<0.001) and tail offset (p=0.042). In the learning curve analysis, the occurrence of breached and failed screws and the robot-used time per screw screws showed a significant decreasing trend.
Conclusion
: In the current study, RAPSF was highly accurate and the specific potential risk factors were not identified. However, pedicle width was presumed to be related to breached screw. Meanwhile, the robot-used time per screw and the incidence of breached and failed screws decreased with the learning curve.
Keyword
Figure
Reference
-
References
1. Ahern DP, Gibbons D, Schroeder GD, Vaccaro AR, Butler JS. Image-guidance, robotics, and the future of spine surgery. Clin Spine Surg. 33:179–184. 2020.
Article2. Attar A, Ugur HC, Uz A, Tekdemir I, Egemen N, Genc Y. Lumbar pedicle: surgical anatomic evaluation and relationships. Eur Spine J. 10:10–15. 2001.
Article3. Avrumova F, Morse KW, Heath M, Widmann RF, Lebl DR. Evaluation of K-wireless robotic and navigation assisted pedicle screw placement in adult degenerative spinal surgery: learning curve and technical notes. J Spine Surg. 7:141–154. 2021.
Article4. Broadbent E, Kuo IH, Lee YI, Rabindran J, Kerse N, Stafford R, et al. Attitudes and reactions to a healthcare robot. Telemed J E Health. 16:608–613. 2010.
Article5. Bydon M, Chen SG, Neal MD, Krishna C, Biedermann AJ, Paul TC, et al. Initiation of a robotic program in spinal surgery: experience at a three-site medical center. Mayo Clin Proc. 96:1193–1202. 2021.6. Castro E Melo JAGME, Faria Araújo NM. Impact of the fourth industrial revolution on the health sector: a qualitative study. Healthc Inform Res. 26:328–334. 2020.
Article7. Cook SD, Salkeld SL, Whitecloud TS 3rd, Barbera J. Biomechanical evaluation and preliminary clinical experience with an expansive pedicle screw design. J Spinal Disord. 13:230–236. 2000.
Article8. D’Souza M, Gendreau J, Feng A, Kim LH, Ho AL, Veeravagu A. Robotic-assisted spine surgery: history, efficacy, cost, and future trends. Robot Surg. 6:9–23. 2019.9. Fan Y, Peng Du J, Liu JJ, Zhang JN, Liu SC, Hao DJ. Radiological and clinical differences among three assisted technologies in pedicle screw fixation of adult degenerative scoliosis. Sci Rep. 8:890. 2018.
Article10. Gao S, Lv Z, Fang H. Robot-assisted and conventional freehand pedicle screw placement: a systematic review and meta-analysis of randomized controlled trials. Eur Spine J. 27:921–930. 2018.
Article11. Gosrisirikul C, Don Chang K, Raheem AA, Rha KH. New era of robotic surgical systems. Asian J Endosc Surg. 11:291–299. 2018.
Article12. Ho C, Tsakonas E, Tran K, Cimon K, Severn M, Mierzwinski-Urban M, et al. Robot-assisted surgery compared with open surgery and laparoscopic surgery. CADTH Technol Overv. 2:e2203. 2012.13. Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res. 472:1839–1844. 2014.
Article14. Huang M, Tetreault TA, Vaishnav A, York PJ, Staub BN. The current state of navigation in robotic spine surgery. Ann Transl Med. 9:86. 2021.
Article15. Jiang B, Pennington Z, Azad T, Liu A, Ahmed AK, Zygourakis CC, et al. Robot-assisted versus freehand instrumentation in short-segment lumbar fusion: experience with real-time image-guided spinal robot. World Neurosurg. 136:e635–e645. 2020.
Article16. Khan A, Meyers JE, Siasios I, Pollina J. Next-generation robotic spine surgery: first report on feasibility, safety, and learning curve. Oper Neurosurg (Hagerstown). 17:61–69. 2019.
Article17. Kim HJ, Lee SH, Chang BS, Lee CK, Lim TO, Hoo LP, et al. Monitoring the quality of robot-assisted pedicle screw fixation in the lumbar spine by using a cumulative summation test. Spine (Phila Pa 1976). 40:87–94. 2015.
Article18. Kuo LJ, Lin YK, Chang CC, Tai CJ, Chiou JF, Chang YJ. Clinical outcomes of robot-assisted intersphincteric resection for low rectal cancer: comparison with conventional laparoscopy and multifactorial analysis of the learning curve for robotic surgery. Int J Colorectal Dis. 29:555–562. 2014.
Article19. Laudato PA, Pierzchala K, Schizas C. Pedicle screw insertion accuracy using O-arm, robotic guidance, or freehand technique: a comparative study. Spine (Phila Pa 1976). 43:E373–E378. 2018.20. Li HM, Zhang RJ, Shen CL. Accuracy of pedicle screw placement and clinical outcomes of robot-assisted technique versus conventional freehand technique in spine surgery from nine randomized controlled trials: a meta-analysis. Spine (Phila Pa 1976). 45:E111–E119. 2020.21. Lieberman IH, Kisinde S, Hesselbacher S. Robotic-assisted pedicle screw placement during spine surgery. JBJS Essent Surg Tech. 10:e0020. 2020.
Article22. Lien SB, Liou NH, Wu SS. Analysis of anatomic morphometry of the pedicles and the safe zone for through-pedicle procedures in the thoracic and lumbar spine. Eur Spine J. 16:1215–1222. 2007.
Article23. Lopez IB, Benzakour A, Mavrogenis A, Benzakour T, Ahmad A, Lemée JM. Robotics in spine surgery: systematic review of literature. Int Orthop. 47:447–456. 2023.
Article24. Lynn G, Mukherjee DP, Kruse RN, Sadasivan KK, Albright JA. Mechanical stability of thoracolumbar pedicle screw fixation: the effect of crosslinks. Spine. 25:31S–35S. 2000.
Article25. Mahomed S. Healthcare, artificial intelligence and the Fourth Industrial Revolution: ethical, social and legal considerations. S Afr J Bioeth Law. 11:93–95. 2018.
Article26. Peng YN, Tsai LC, Hsu HC, Kao CH. Accuracy of robot-assisted versus conventional freehand pedicle screw placement in spine surgery: a systematic review and meta-analysis of randomized controlled trials. Ann Transl Med. 8:824. 2020.
Article27. Pennington Z, Judy BF, Zakaria HM, Lakomkin N, Mikula AL, Elder BD, et al. Learning curves in robot-assisted spine surgery: a systematic review and proposal of application to residency curricula. Neurosurg Focus. 52:E3. 2022.
Article28. Ringel F, Stüer C, Reinke A, Preuss A, Behr M, Auer F, et al. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomized comparison to conventional freehand screw implantation. Spine (Phila Pa 1976). 37:E496–E501. 2012.29. Schatlo B, Martinez R, Alaid A, von Eckardstein K, Akhavan-Sigari R, Hahn A, et al. Unskilled unawareness and the learning curve in robotic spine surgery. Acta Neurochir (Wien). 157:1819–1823. discussion 1823. 2015.
Article30. Shin MH, Ryu KS, Park CK. Accuracy and safety in pedicle screw placement in the thoracic and lumbar spines : comparison study between conventional C-arm fluoroscopy and navigation coupled with O-arm® guided methods. J Korean Neurosurg Soc. 52:204–209. 2012.
Article31. Siddiqui MI, Wallace DJ, Salazar LM, Vardiman AB. Robot-assisted pedicle screw placement: learning curve experience. World Neurosurg. 130:e417–e422. 2019.
Article32. Tiwari A, Pandey S, Naik DC. A study of height and width of typical lumbar pedicles in relation to mechanical load. Int J Med Sci Public Health. 4:275. 2015.
Article33. Toossi N, Vardiman AB, Benech CA, Kanaly CW, Maltenfort MG, Backes DM, et al. Factors affecting the accuracy of pedicle screw placement in robot-assisted surgery: a multicenter study. Spine (Phila Pa 1976). 47:1613–1619. 2022.
Article34. Vardiman AB, Wallace DJ, Crawford NR, Riggleman JR, Ahrendtsen LA, Ledonio CG. Pedicle screw accuracy in clinical utilization of minimally invasive navigated robot-assisted spine surgery. J Robot Surg. 14:409–413. 2020.
Article35. Vo CD, Jiang B, Azad TD, Crawford NR, Bydon A, Theodore N. Robotic spine surgery: current state in minimally invasive surgery. Global Spine J. 10(2 Suppl):34S–40S. 2020.
Article36. Yi M, Song J, Zhang Y, Lin W, Yao M, Fan Y, et al. Risk factor analysis of the accuracy and safety of planned and actual screw paths with robot-assisted technology. Available at : https://doi.org/10.21203/rs.3.rs-2220116/v1.
Article37. Zhang JN, Fan Y, Hao DJ. Risk factors for robot-assisted spinal pedicle screw malposition. Sci Rep. 9:3025. 2019.
Article38. Zhang Q, Fan MX, Han XG, Liu YJ, He D, Liu B, et al. Risk factors of unsatisfactory robot-assisted pedicle screw placement: a case-control study. Neurospine. 18:839–844. 2021.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robotic spine systems: overcoming surgeon experience in pedicle screw accuracy: a prospective study
- Risk Factors of Unsatisfactory Robot-Assisted Pedicle Screw Placement: A Case-Control Study
- Learning Curve for Robot-Assisted Percutaneous Pedicle Screw Placement in Thoracolumbar Surgery
- Robotic-Assisted Spine Surgery: Role in Training the Next Generation of Spine Surgeons
- Learning Curve of ROSA ONE Spine System for Transpedicular Screw Placement