J Korean Assoc Oral Maxillofac Surg.
2023 Dec;49(6):339-346. 10.5125/jkaoms.2023.49.6.339.
Dental trauma trends in emergency care: a comparative analysis before, during, and after COVID-19
- Affiliations
-
- 1Department of Conservative Dentistry, Section of Dentistry, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2550297
- DOI: http://doi.org/10.5125/jkaoms.2023.49.6.339
Abstract
Objectives
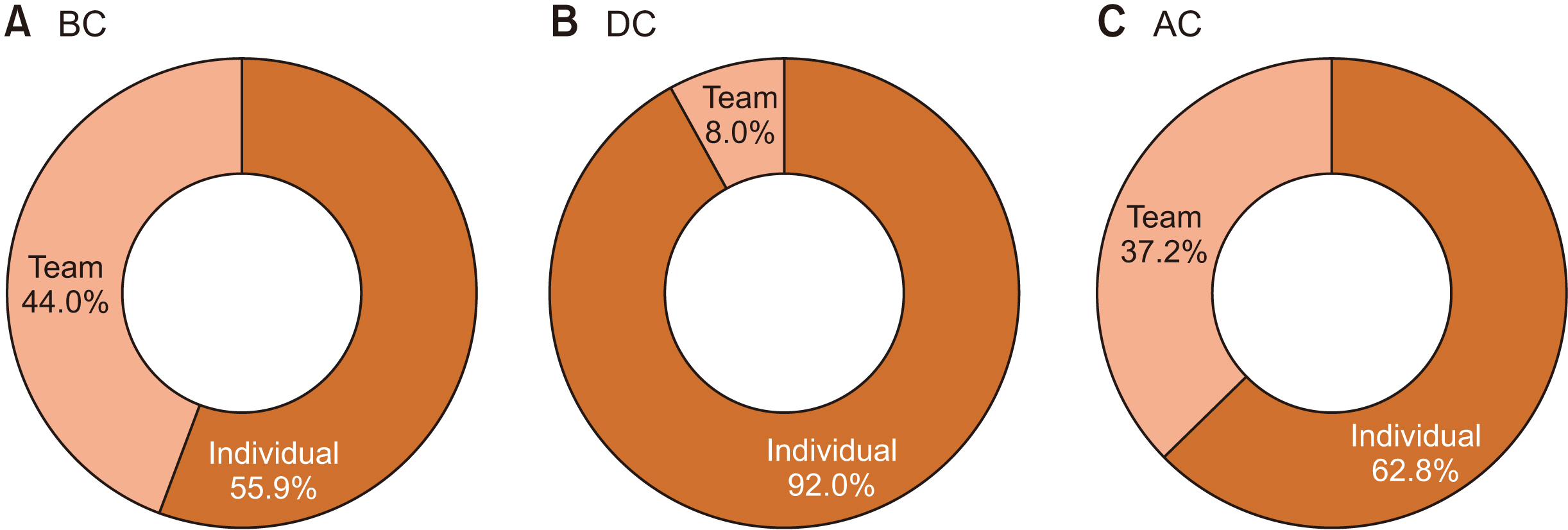
This analysis details the characteristics of dental trauma in South Korea during the coronavirus disease 2019 (COVID-19) (DC) pandemic and compares them in patients before and after COVID-19 (BC and AC, respectively).
Materials and Methods
Data were collected from medical records of patients who visited Seoul National University Bundang Hospital’s Emergency Dental Care Center during three 12-month periods: BC, DC, and AC (BC from March 1, 2019 to February 29, 2020; DC from March 1, 2020 to February 28, 2021; AC from March 1, 2022 to February 28, 2023). A retrospective review was conducted to investigate patient age, sex, time of visit, cause, and diagnosis. The study included 1,544 patients: 660 BC, 374 DC, and 510 AC.
Results
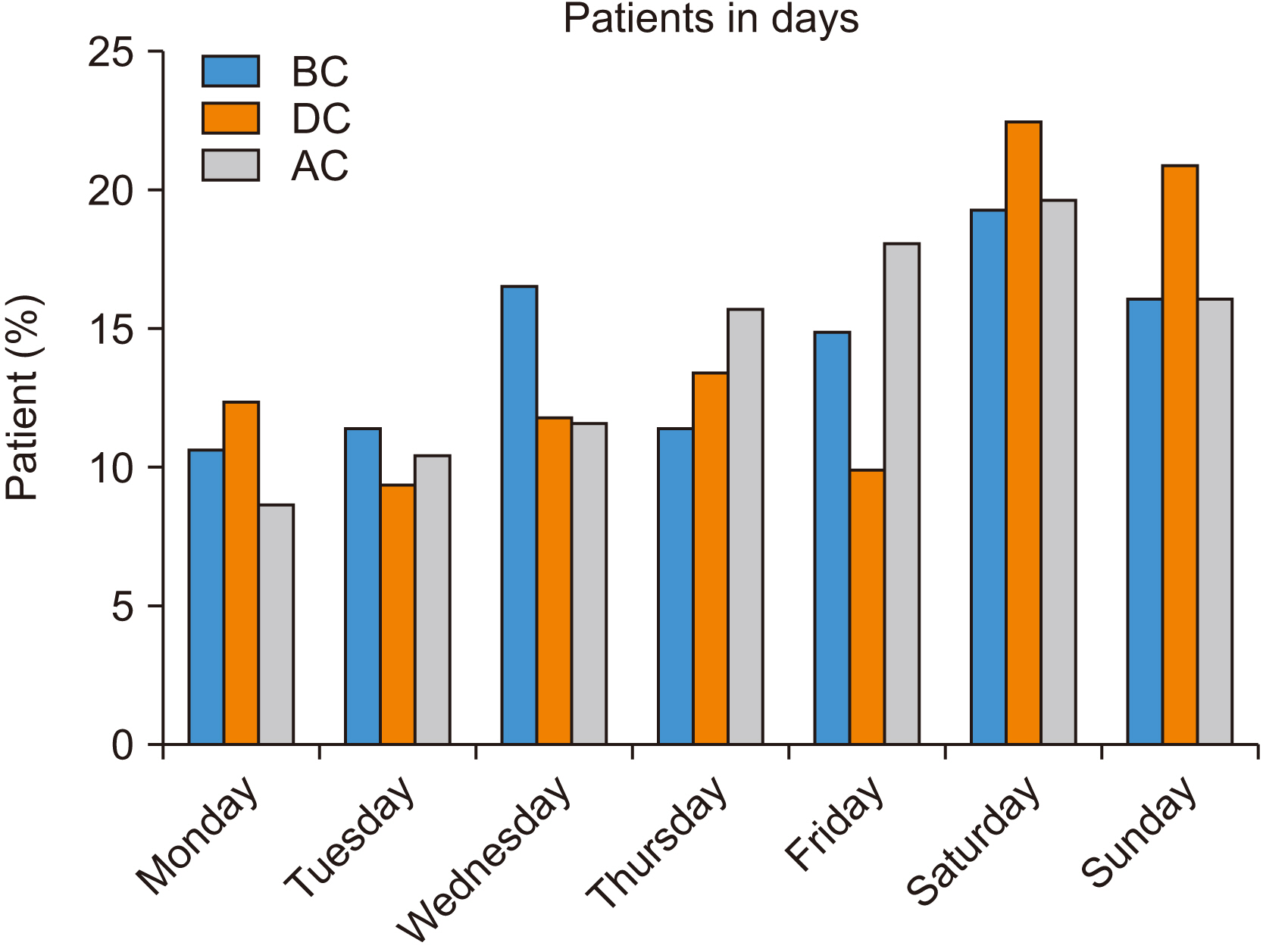
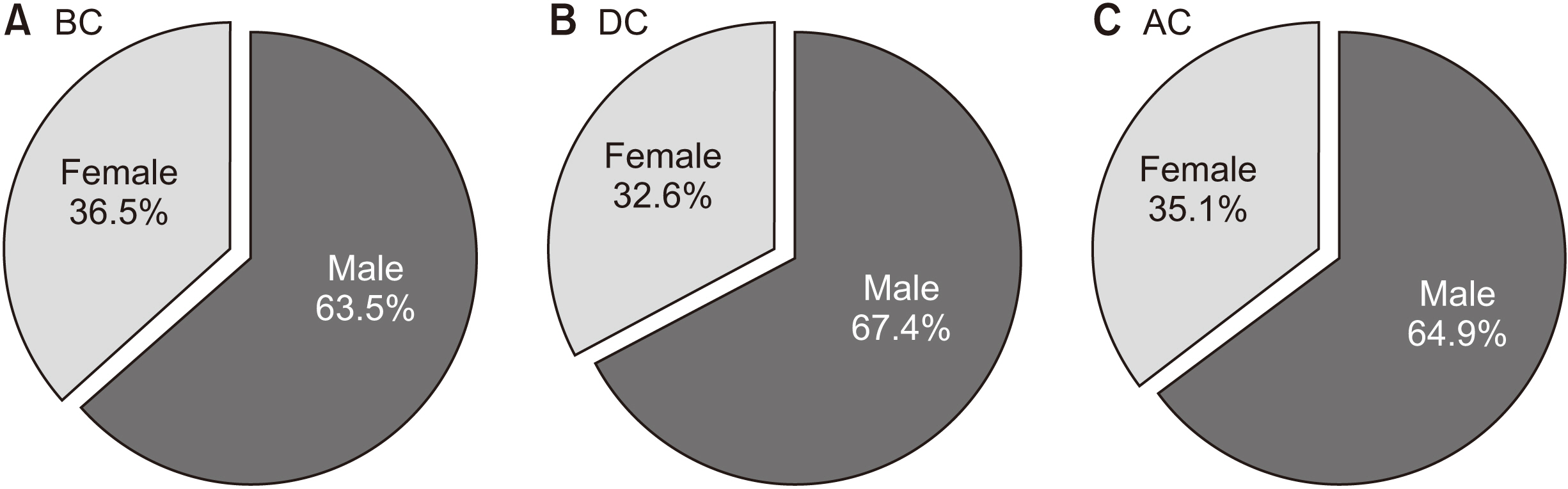
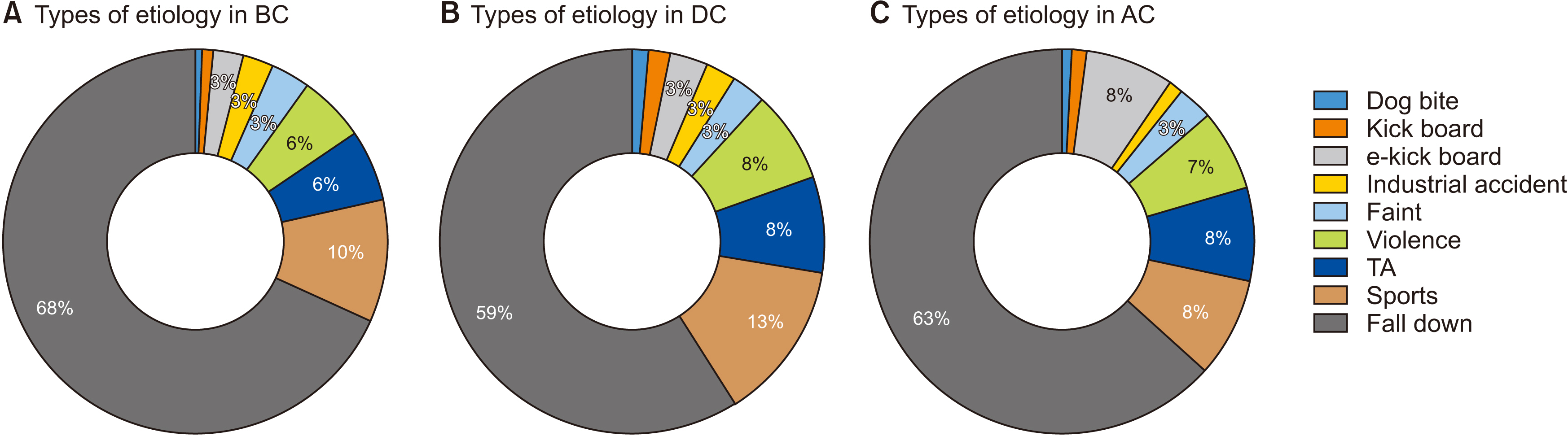
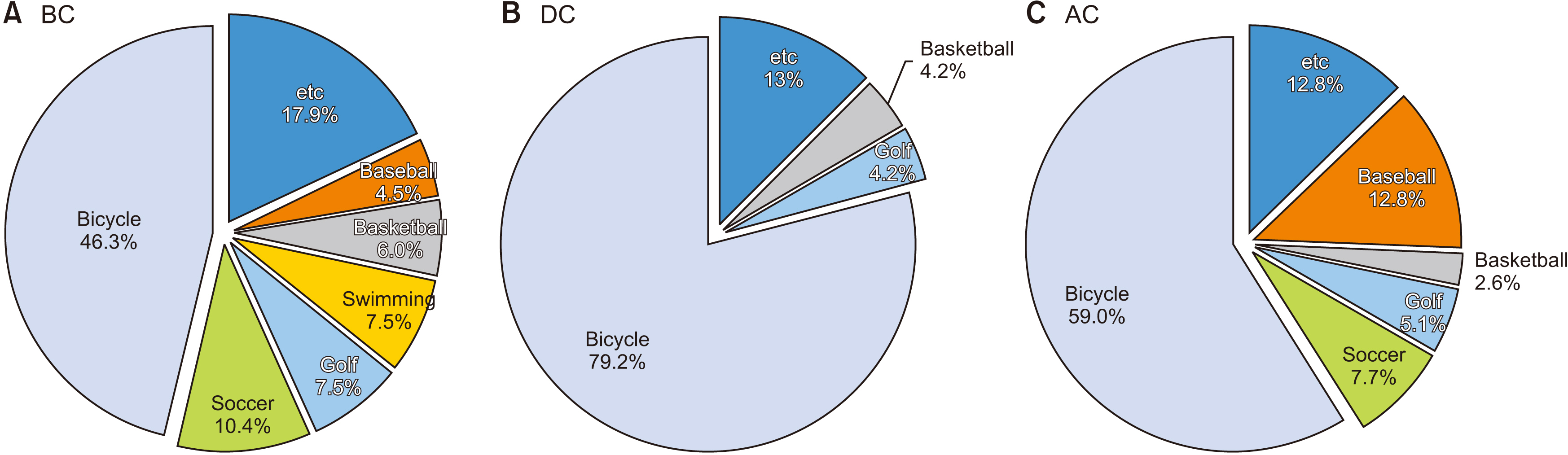
Significant difference in age and sex was not observed among the three periods; 1-9 years of age was the largest group (38.3% in BC, 29.6% in DC, and 27.8% in AC), and the percentage of male patients was greater than of female patients (male proportion as 63.5% in BC, 67.4% in DC, and 64.9% in AC). The number of patients generally peaked at a Saturday night in spring (for BC: May, Saturday, 18:00-19:59; for DC: March, Saturday, 18:00-19:59; for AC: April as the second most (October as the most peaked), Saturday, 20:00-21:59). The primary etiology of the dental trauma was identical in the three periods: falls, followed by sports. The most frequent diagnosis was laceration, followed by tooth avulsion and jaw fracture.
Conclusion
Significant differences were not found between the characteristics and patterns of dental trauma in the BC, DC, and AC periods. However, due to the pandemic and social distancing, activities decreased and associated dental trauma-related incidents declined.
Figure
Reference
-
References
1. Sirin DA, Ozcelik F. 2021; The relationship between COVID-19 and the dental damage stage determined by radiological examination. Oral Radiol. 37:600–9. https://doi.org/10.1007/s11282-020-00497-0. DOI: 10.1007/s11282-020-00497-0. PMID: 33389600. PMCID: PMC7778567.2. Han E, Tan MMJ, Turk E, Sridhar D, Leung GM, Shibuya K, et al. 2020; Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. 396:1525–34. https://doi.org/10.1016/s0140-6736(20)32007-9. DOI: 10.1016/S0140-6736(20)32007-9. PMID: 32979936.3. Korea Disease Control and Prevention Agency (KDCA). 2020. Updates on COVID-19 in Republic of Korea: change to social distancing level 1 (October 12) [Internet]. KDCA;Cheongju: Available from: https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&act=view&list_no=710834. cited 2020 Dec 14.4. Woolley J, Djemal S. 2021; Traumatic dental injuries during the COVID-19 pandemic. Prim Dent J. 10:28–32. https://doi.org/10.1177/2050168420980994. DOI: 10.1177/2050168420980994. PMID: 33722141.5. Huang C, Yang Y, Wang Z, Wang W, Liu Y, Zhang M. 2022; A retrospective study of emergent traumatic dental injuries in permanent teeth in Xiʼan, China. Medicine (Baltimore). 101:e32588. https://doi.org/10.1097/md.0000000000032588. DOI: 10.1097/MD.0000000000032588. PMID: 36596078. PMCID: PMC9803479.6. Madi M, Kumar M, Varchas P, Vineetha R, Pentapati KC. 2021; Changing trends in the outpatient dental visits during the COVID - 19 pandemic in a tertiary care hospital. Saudi J Biol Sci. 28:4437–41. https://doi.org/10.1016/j.sjbs.2021.04.038. DOI: 10.1016/j.sjbs.2021.04.038. PMID: 33903794. PMCID: PMC8059255.7. Maffia F, Fontanari M, Vellone V, Cascone P, Mercuri LG. 2020; Impact of COVID-19 on maxillofacial surgery practice: a worldwide survey. Int J Oral Maxillofac Surg. 49:827–35. https://doi.org/10.1016/j.ijom.2020.04.015. DOI: 10.1016/j.ijom.2020.04.015. PMID: 32414678. PMCID: PMC7196383.8. Puglia FA, Hills A, Dawoud B, Magennis P. Chiu GA; Collaborators. 2021; Management of oral and maxillofacial trauma during the first wave of the COVID-19 pandemic in the United Kingdom. Br J Oral Maxillofac Surg. 59:867–74. https://doi.org/10.1016/j.bjoms.2020.12.021. DOI: 10.1016/j.bjoms.2020.12.021. PMID: 34325945. PMCID: PMC7836223.9. Salzano G, Audino G, Vaira LA, Trevisiol L, et al. DellʼAversana Orabona G. DʼAgostino A. 2021; Have there been any changes in the epidemiology and etiology of maxillofacial trauma during the COVID-19 pandemic? An Italian multicenter study. J Craniofac Surg. 32:1445–7. https://doi.org/10.1097/scs.0000000000007253. DOI: 10.1097/SCS.0000000000007253. PMID: 33229987. PMCID: PMC8162046.10. Bae JH, Kim YK, Choi YH. 2011; Clinical characteristics of dental emergencies and prevalence of dental trauma at a university hospital emergency center in Korea. Dent Traumatol. 27:374–8. https://doi.org/10.1111/j.1600-9657.2011.01013.x. DOI: 10.1111/j.1600-9657.2011.01013.x. PMID: 21615683.11. Guo H, Zhou Y, Liu X, Tan J. 2020; The impact of the COVID-19 epidemic on the utilization of emergency dental services. J Dent Sci. 15:564–7. https://doi.org/10.1016/j.jds.2020.02.002. DOI: 10.1016/j.jds.2020.02.002. PMID: 32296495. PMCID: PMC7156222.12. Kim MY, Park JW, Choi YH. 2018; Clinical characteristics of dental emergencies and dental trauma at an emergency center. J Korean Acad Sports Dent. 1:11–5.13. Shin KY, Kim SN, Lee DK, Yim CJ. 1990; A clinical study of the incidence and prognosis of the traumatic tooth injury. J Korean Assoc Oral Maxillofac Surg. 16:74–84.14. Shin SH, Choo SH. 2022; Exploring the influencing factors on change in use of sharing mobility by the COVID-19 pandemic: focused on residents in new towns. J Korean Soc Transp. 40:230–44. https://doi.org/10.7470/jkst.2022.40.2.230. DOI: 10.7470/jkst.2022.40.2.230.15. Jang CS, Lee CY, Kim JW, Yim JH, Kim JY, Kim YH, et al. 2011; A clinical study on the dental emergency patients visiting an university hospital emergency room. J Korean Assoc Oral Maxillofac Surg. 37:439–47. http://doi.org/10.5125/jkaoms.2011.37.6.439. DOI: 10.5125/jkaoms.2011.37.6.439.16. Kim JH, Jung HI, Kim IH, Lee J, Kang CM. 2022; Impact of Coronavirus disease 2019 on dental service utilization of Korean children and adolescents. J Korean Acad Pediatr Dent. 49:206–16. https://doi.org/10.5933/JKAPD.2022.49.2.206. DOI: 10.5933/JKAPD.2022.49.2.206.17. Yeoh M, Lai JB, Ng CH. 2023; Learning from Covid 19 in a level 1 oral and maxillofacial trauma centre - Insights for the future. J Oral Maxillofac Surg Med Pathol. 35:195–200. https://doi.org/10.1016/j.ajoms.2022.09.001. DOI: 10.1016/j.ajoms.2022.09.001. PMID: 36168323. PMCID: PMC9502433.18. Cha DW. 2020; Mobility industry innovation prospects spurred by COVID-19. Future Horiz. 48:24–31.19. Fu XJ, Li WS, Xiang L, Liao LS. 2022; Analysis of 256 pediatric oral and maxillofacial emergency in-patients during the outbreak of COVID-19. Dent Traumatol. 38:367–73. https://doi.org/10.1111/edt.12759. DOI: 10.1111/edt.12759. PMID: 35605156. PMCID: PMC9347499.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Activities and Roles of Trauma Surgeons in the Treatment of COVID-19 Patients
- The Trend of Change in Oral and Maxillofacial Injuries of Pediatric Patients in the COVID-19 Pandemic: a Regional Emergency Medical Center and Dental Hospital Study
- Comparative Analysis of COVID-19 Outbreak and Changes in Neurosurgical Emergency Patients
- Impact of COVID-19 on Dental Trauma in Korea
- The impacts of the COVID-19 pandemic on emergency care utilization in patients with major emergency diseases in Chungnam Province