J Neurocrit Care.
2023 Dec;16(2):101-106. 10.18700/jnc.230034.
A case report of pitfall of fever and altered mental status: cerebral malaria due to Plasmodium falciparum in an adult traveler returning from Congo
- Affiliations
-
- 1Department of Neurology, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea
- 2Department of Critical Care Medicine, Hallym University Kangdong Sacred Heart Hospital, Seoul, Korea
- KMID: 2549487
- DOI: http://doi.org/10.18700/jnc.230034
Abstract
- Background
Cerebral malaria, caused by Plasmodium falciparum, can lead to severe neurological complications. It is more frequently observed in children than in adults. Because cerebral malaria is rare and has no specific symptoms or neurologic findings, it is not easy to diagnose.
Case report
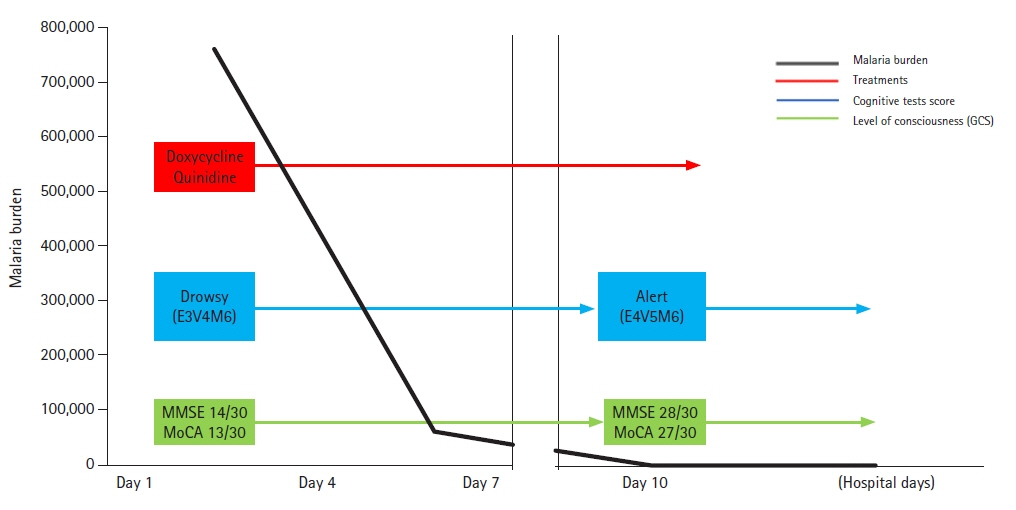
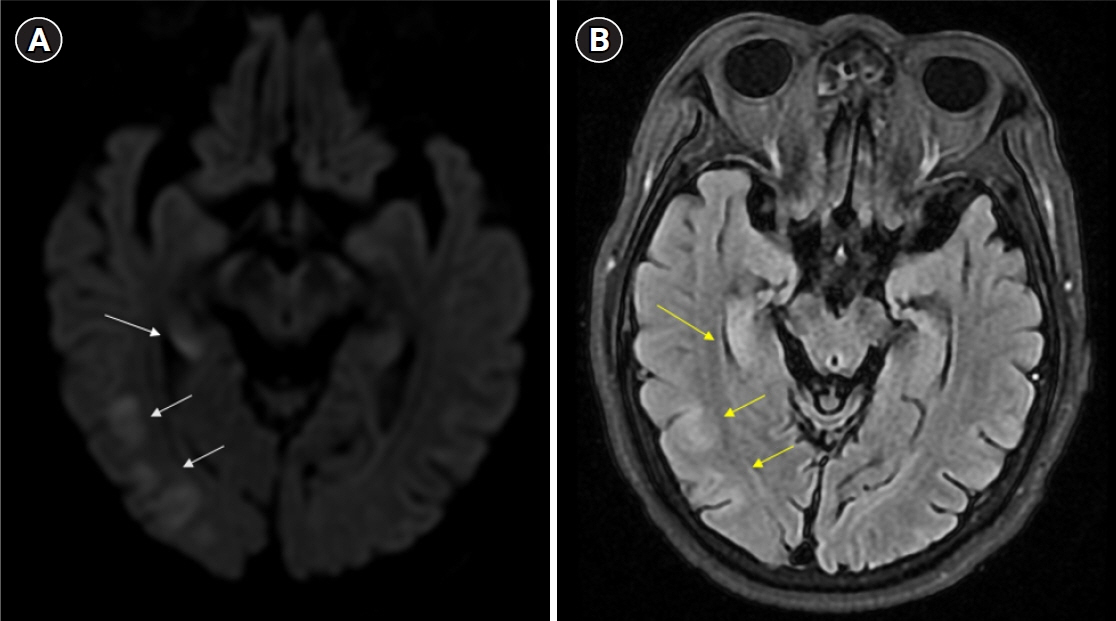
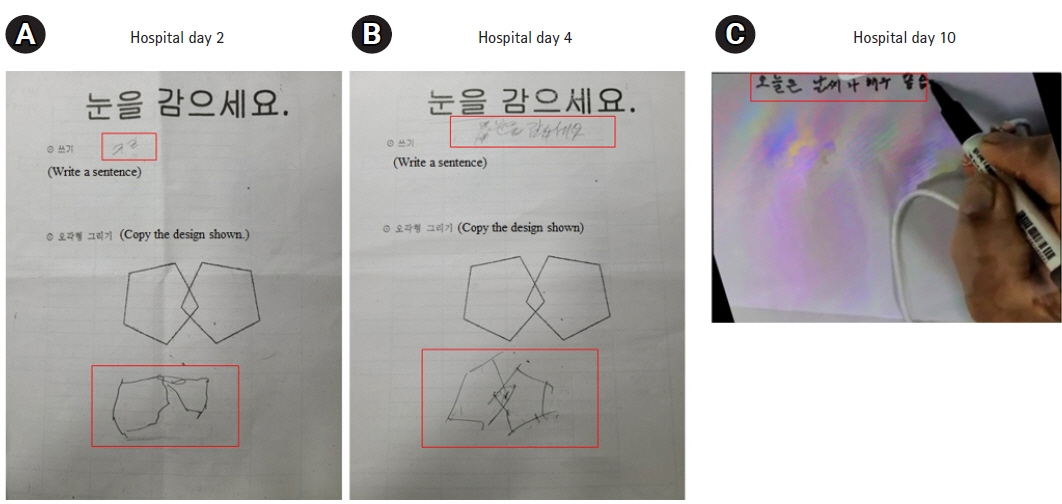
We report a case of a 61-year-old male who returned from the Democratic Republic of the Congo with fever, fatigue, and confusion. With considering cerebral malaria, a peripheral blood smear confirmed P. falciparum infection (initial parasite load, 760,800/μL; ring form, 100%). Cerebrospinal fluid analyses showed high protein level (103.2 mg/dL). Electroencephalograms showed background slowing activity. Brain magnetic resonance imaging showed signal changes and cerebral swelling. The initial doxycycline and quinidine treatment for malaria was successful without sequalae.
Conclusion
Physicians must have high suspicion about the symptoms and the necessity for screening in individuals traveling to malaria-endemic regions when experiencing changes in consciousness.
Keyword
Figure
Reference
-
1. Roberson MT, Smith AT. Cerebral malaria in a patient with recent travel to the Congo presenting with delirium: a case report. Clin Pract Cases Emerg Med. 2020; 4:533–6.2. Marsh K, English M, Crawley J, Peshu N. The pathogenesis of severe malaria in African children. Ann Trop Med Parasitol. 1996; 90:395–402.3. Idro R, Marsh K, John CC, Newton CR. Cerebral malaria: mechanisms of brain injury and strategies for improved neurocognitive outcome. Pediatr Res. 2010; 68:267–74.4. Breman JG. The ears of the hippopotamus: manifestations, determinants, and estimates of the malaria burden. Am J Trop Med Hyg. 2001; 64(1-2 Suppl):1–11.5. van Hensbroek MB, Palmer A, Jaffar S, Schneider G, Kwiatkowski D. Residual neurologic sequelae after childhood cerebral malaria. J Pediatr. 1997; 131(1 Pt 1):125–9.6. Storm J, Craig AG. Pathogenesis of cerebral malaria: inflammation and cytoadherence. Front Cell Infect Microbiol. 2014; 4:100.7. Sein KK, Maeno Y, Thuc HV, Anh TK, Aikawa M. Differential sequestration of parasitized erythrocytes in the cerebrum and cerebellum in human cerebral malaria. Am J Trop Med Hyg. 1993; 48:504–11.8. Schiess N, Villabona-Rueda A, Cottier KE, Huether K, Chipeta J, Stins MF. Pathophysiology and neurologic sequelae of cerebral malaria. Malar J. 2020; 19:266.9. Mohanty S, Benjamin LA, Majhi M, Panda P, Kampondeni S, Sahu PK, et al. Magnetic resonance imaging of cerebral malaria patients reveals distinct pathogenetic processes in different parts of the brain. mSphere. 2017; 2:e00193–17.10. Misra UK, Kalita J, Prabhakar S, Chakravarty A, Kochar D, Nair PP. Cerebral malaria and bacterial meningitis. Ann Indian Acad Neurol. 2011; 14(Suppl 1):S35–9.11. Gure TR, Langa KM, Fisher GG, Piette JD, Plassman BL. Functional limitations in older adults who have cognitive impairment without dementia. J Geriatr Psychiatry Neurol. 2013; 26:78–85.12. Kumral E, Bayam FE, Köken B, Erdoğan CE. Clinical and neuroimaging determinants of minimally conscious and persistent vegetative states after acute stroke. J Neurocrit Care. 2019; 12:37–45.13. Kampondeni SD, Potchen MJ, Beare NA, Seydel KB, Glover SJ, Taylor TE, et al. MRI findings in a cohort of brain injured survivors of pediatric cerebral malaria. Am J Trop Med Hyg. 2013; 88:542–6.14. Karimi M, Nazari S, Shirani F, Alivirdiloo V, Siahposht-Khachaki A, Edalatkhah S, et al. Neuroprotective effects of chloroquine on neurological scores, blood-brain barrier permeability, and brain edema after traumatic brain injury in male rats. J Neurocrit Care. 2023; 16:18–27.15. Clark DJ, Bond C, Andrews A, Muller DJ, Sarkisian A, Opoka RO, et al. Admission clinical and EEG features associated with mortality and long-term neurologic and cognitive outcomes in pediatric cerebral malaria. Neurology. 2023; 101:e1307–18.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Cerebral Infarcts Following Acute Plasmodium vivax Infection
- Retinal Hemorrhage in an Adult with P. vivax Malaria
- Mixed Infection with Plasmodium falciparum and Plasmodium ovale in a Returned Traveller: the First Case in Korea
- Blackwater Fever Followed by Severe Falciparum Malaria in a Child
- Two Cases of Cerebral Malaria Treated with Therapeutic Erythrocytapheresie