J Cerebrovasc Endovasc Neurosurg.
2023 Dec;25(4):434-439. 10.7461/jcen.2023.E2022.11.001.
Flow diversion of a middle cerebral artery pseudoaneurysm secondary to a gunshot wound: A case report
- Affiliations
-
- 1Harvard Medical School, Boston, Massachusetts, USA
- 2Neurosurgical Service, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA
- 3Department of Neurosurgery, MedStar Washington Hospital Center, Washington, DC, USA
- KMID: 2549449
- DOI: http://doi.org/10.7461/jcen.2023.E2022.11.001
Abstract
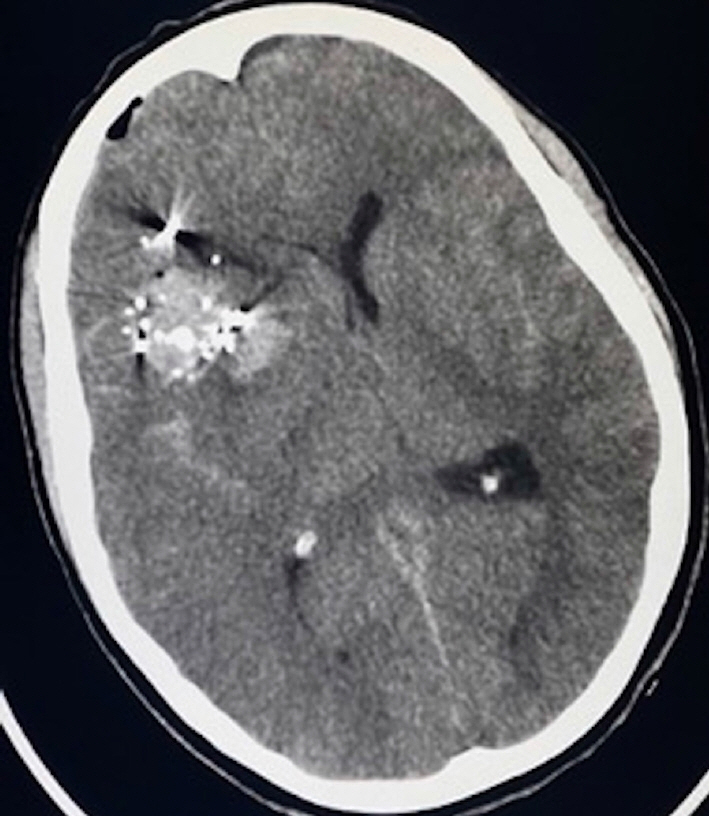
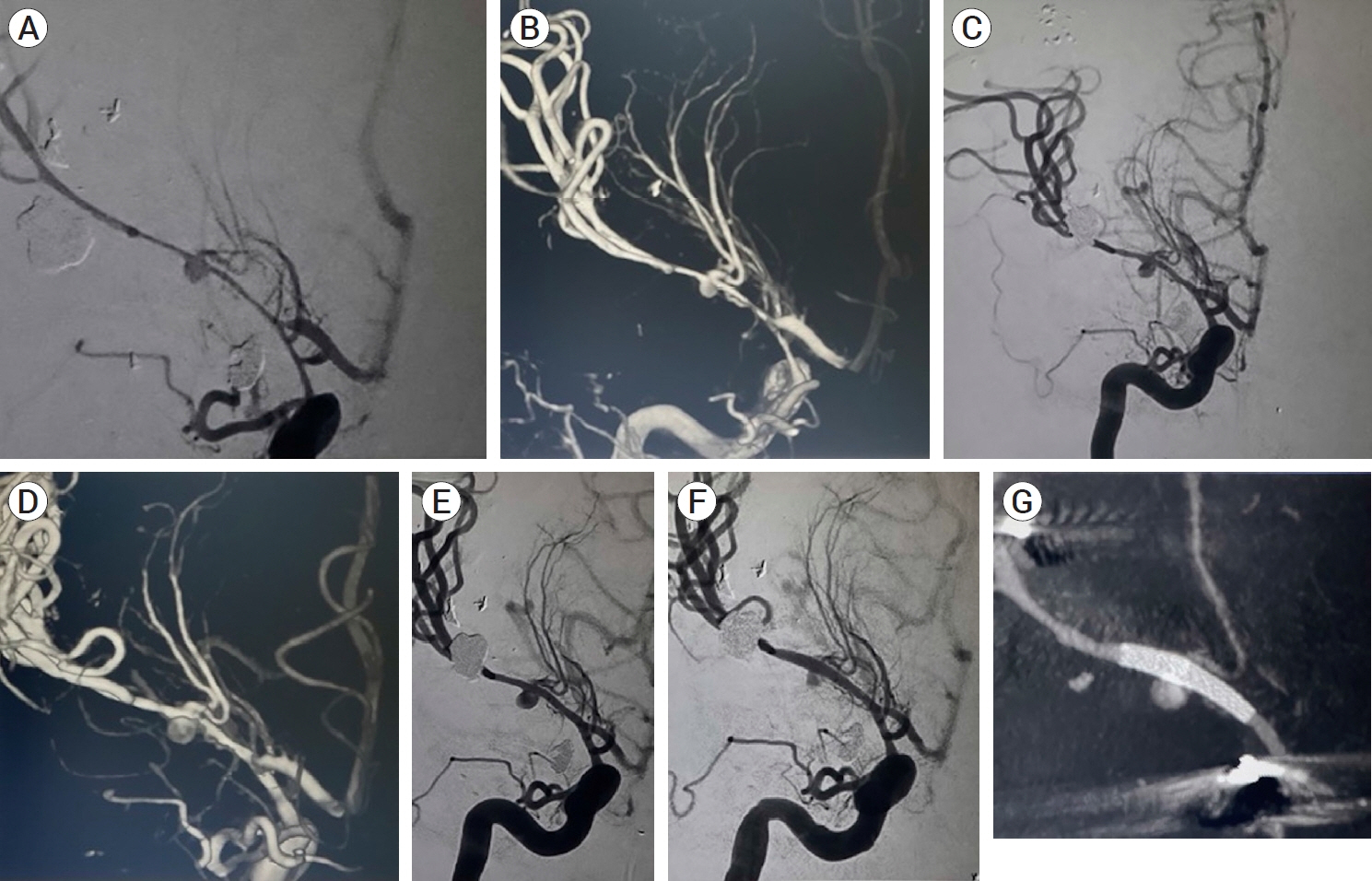
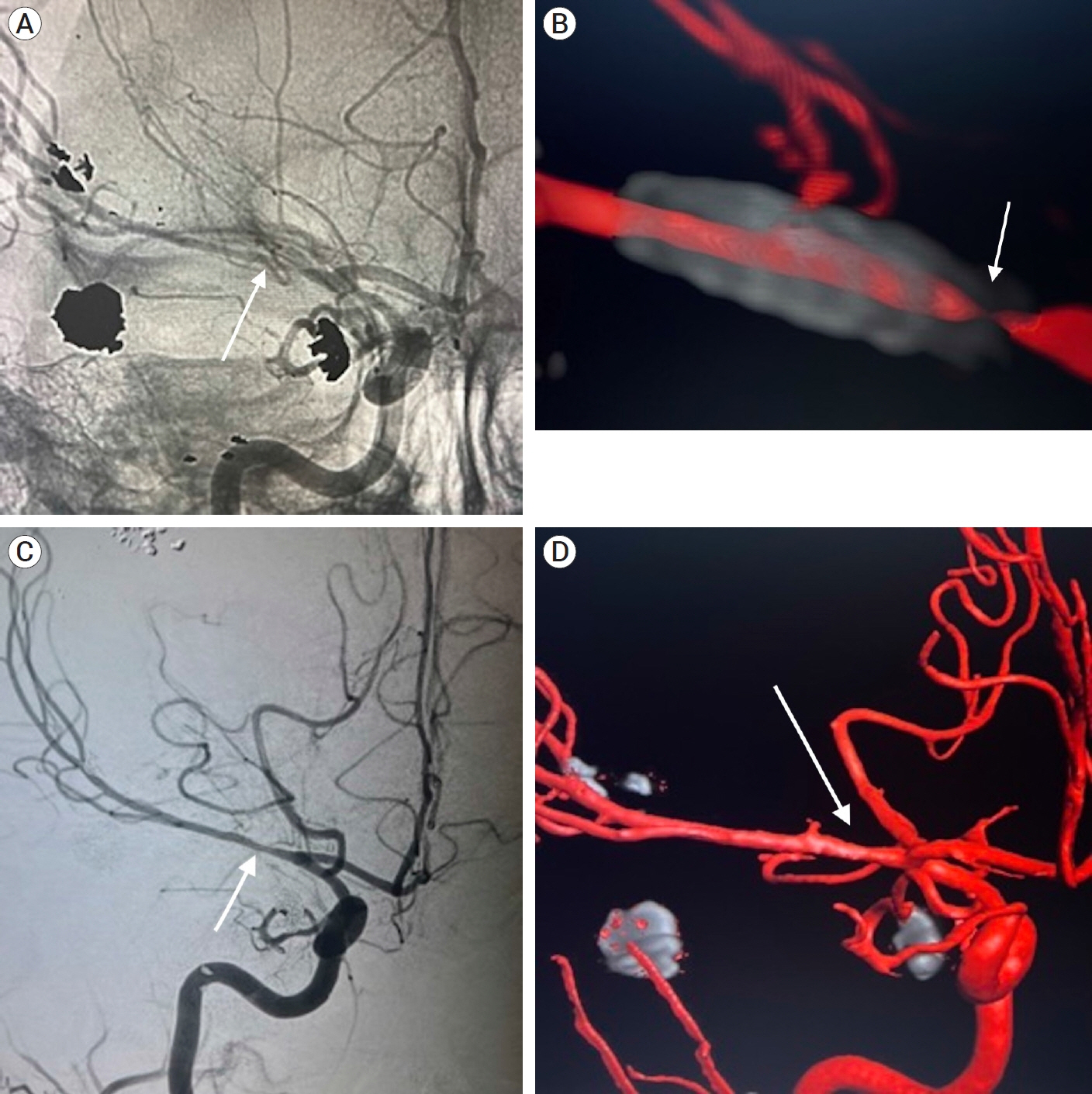
- Pseudoaneurysms are rare but devastating complications of penetrating head traumas. They require rapid surgical or endovascular intervention due to their high risk of rupture; however, complex presentations may limit treatment options. Our objective is to report a case of severe vasospasm, flow diversion, and in-stent stenosis complicating the treatment of a middle cerebral artery pseudoaneurysm following a gunshot wound. A 33-year-old woman presented with multiple calvarial and bullet fragments within the right frontotemporal lobes and a large right frontotemporal intraparenchymal hemorrhage with significant cerebral edema. She underwent an emergent right hemicraniectomy for decompression, removal of bullet fragments, and evacuation of hemorrhage. Once stable enough for diagnostic cerebral angiography, she was found to have an M1 pseudoaneurysm with severe vasospasm that precluded endovascular treatment until the vasospasm resolved. The pseudoaneurysm was treated with flow diversion and in-stent stenosis was found at 4-month follow-up angiography that resolved by 8 months post-embolization. We report the successful flow diversion of an middle cerebral artery (MCA) pseudoaneurysm complicated by severe vasospasm and later in-stent stenosis. The presence of asymptomatic stenosis is believed to be reversible intimal hyperplasia and a normal aspect of endothelial healing. We suggest careful observation and dual-antiplatelet therapy as a justified approach.
Keyword
Figure
Reference
-
1. Aljuboori Z, Meyer K, Ding D, James R. Endovascular treatment of a traumatic middle cerebral artery pseudoaneurysm with the pipeline flex embolization device. World Neurosurg. 2020; Jan. 133:201–4.2. Anderson E, Chalouhi N, Dumont A, Tjoumakaris S, Zanaty M, Rosenwasser R, et al. Management of head and neck pseudoaneurysms: A review of 33 consecutive cases. The Scientific World Journal. 2014; 2014:419803.3. Cohen JE, Gomori JM, Segal R, Spivak A, Margolin E, Sviri G, et al. Results of endovascular treatment of traumatic intracranial aneurysms. Neurosurgery. 2008; Sep. 63(3):476–85. discussion 485. –6.4. Cooper JB, Greisman JD, Dakay K, Kaur G, Al-Mufti F, Gandhi CD, et al. Incidence of neo-intimal hyperplasia in anterior circulation aneurysms following pipeline flow diversion. J Stroke Cerebrovasc Dis. 2021; Jul. 30(7):105794.5. Elias AE, Chaudhary N, Pandey AS, Gemmete JJ. Intracranial endovascular balloon test occlusion: Indications, methods, and predictive value. Neuroimaging Clin N Am. 2013; Nov. 23(4):695–702.6. Ghorbani M, Shojaei H, Bavand K, Azar M. Surpass streamline flow-diverter embolization device for treatment of iatrogenic and traumatic internal carotid artery injuries. AJNR Am J Neuroradiol. 2018; Jun. 39(6):1107–11.7. Ghorbani M, Wipplinger C, Griessenauer CJ, Shojaei H, Abdolhoseinpour H. Successful endoluminal reconstruction of a pseudoaneurysm of the internal carotid artery following a transorbital stab injury. Clin Neurol Neurosurg. 2020; Jul. 194:105838.8. Horiuchi T, Nakagawa F, Miyatake M, Iwashita T, Tanaka Y, Hongo K. Traumatic middle cerebral artery aneurysm: Case report and review of the literature. Neurosurg Rev. 2007; Jul. 30(3):263–7. discussion 267.9. Larson PS, Reisner A, Morassutti DJ, Abdulhadi B, Harpring JE. Traumatic intracranial aneurysms. Neurosurg Focus. 2000; Jan. 8(1):1–6.10. Lee H, Perry JJ, English SW, Alkherayf F, Joseph J, Nobile S, et al. Clinical prediction of delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. J Neurosurg. 2018; Jun. 1–8.11. Luecking H, Doerfler A, Goelitz P, Hoelter P, Engelhorn T, Lang S. Two- to five-year follow-up of 78 patients after treatment with the flow redirection endoluminal device. Interv Neuroradiol. 2020; Feb. 26(1):38–44.12. Mohri M, Ichinose T, Uchiyama N, Misaki K, Nambu I, Takabatake Y, et al. Hyperperfusion syndrome after trapping with high-flow bypass for a giant paraclinoid internal carotid artery aneurysm. World Neurosurg. 2018; Jul. 115:143–6.13. Rajah G, Garling RJ, Rangel-Castilla L. Large traumatic skull base internal carotid artery pseudoaneurysm managed with endovascular flow diversion: 2-dimensional operative video. Oper Neurosurg (Hagerstown). 2018; Dec. 15(6):e84.14. Sastry RA, Koch MJ, Grannan BL, Stapleton CJ, Butler WE, Patel AB. Flow diversion of a recurrent, iatrogenic basilar tip aneurysm in a pediatric patient: Case report. J Neurosurg Pediatr. 2018; Jan. 21(1):90–3.15. Scullen T, Mathkour M, Carr JR, Dumont AS, Amenta PS. Iatrogenic middle cerebral artery ruptured pseudoaneurysm successfully treated with a pipeline embolization device. Ochsner J. 2021; Summer. 21(2):190–3.16. Shi Y, Gao Y, Liu Y, Cui W, Zhou G, Wang L, et al. Treatment of traumatic intracranial pseudoaneurysms: A single-center experience. Front Neurol. 2021; Jun. 12:690284.17. Tan S, Zhou X, Lu Y, Lai L, Huang X, Li B, et al. Low-profile visualized intraluminal support stent for the endovascular treatment of traumatic intracranial internal carotid artery pseudoaneurysms. Neurosurg Rev. 2022; Jun. 45(3):2231–7.18. Tunthanathip T, Phuenpathom N, Sae-Heng S, Oearsakul T, Sakarunchai I, Kaewborisutsakul A. Traumatic cerebrovascular injury: Clinical characteristics and illustrative cases. Neurosurg Focus. 2019; Nov. 47(5):e4.19. Weidauer S, Lanfermann H, Raabe A, Zanella F, Seifert V, Beck J. Impairment of cerebral perfusion and infarct patterns attributable to vasospasm after aneurysmal subarachnoid hemorrhage. Stroke. 2007; Jun. 38(6):1831–6.20. Zanaty M, Chalouhi N, Jabbour P, Starke RM, Hasan D. The unusual angiographic course of intracranial pseudoaneurysms. Asian J Neurosurg. 2015; Oct-Dec. 10(4):327–30.21. Zheng Y, Lu Z, Shen J, Xu F. Intracranial pseudoaneurysms: Evaluation and management. Front Neurol. 2020; Jul. 7. 11:582.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful treatment of visceral pseudoaneurysm after pancreatectomy using flow-diverting stent device
- Symptomatic Post Endarterectomy Common Carotid Artery Pseudoaneurysm Treated with Combination of Flow Diverter Implantation and Carotid Stenting
- A Case Report of Ureteral Injury by Gunshot Wound
- Management of a Gunshot Wound at the Temporal Region: Case Report
- Fracture of the Humeral Shaft Secondary to High-Velocity Gunshot (Machine Gun) Injury: A Case Report