J Cerebrovasc Endovasc Neurosurg.
2023 Dec;25(4):420-428. 10.7461/jcen.2023.E2023.07.004.
Correlation between contrast leakage period of procedural rupture and clinical outcomes in endovascular coiling for cerebral aneurysms
- Affiliations
-
- 1Department of Neurosurgery, Inje University Busan Paik Hospital, Busan, Korea
- 2Department of Neurosurgery, Inje University Haeundae Paik Hospital, Busan, Korea
- 3Department of Radiology, Inje University Busan Paik Hospital, Busan, Korea
- KMID: 2549447
- DOI: http://doi.org/10.7461/jcen.2023.E2023.07.004
Abstract
Objective
Intraprocedural rupture (IPR) is a fatal complication of endovascular coiling for cerebral aneurysms. We hypothesized that contrast leakage period may be related to poor clinical outcomes. This study aimed to retrospectively evaluate the relationship between clinical outcomes and contrast leakage period.
Methods
Data from patients with cerebral aneurysms treated via endovascular coiling between January 2010 and October 2018 were retrospectively assessed. The enrolled patient’s demographic data, the aneurysm related findings, endovascular treatment and IPR related findings, rescue treatment, and clinical outcome were analyzed.
Results
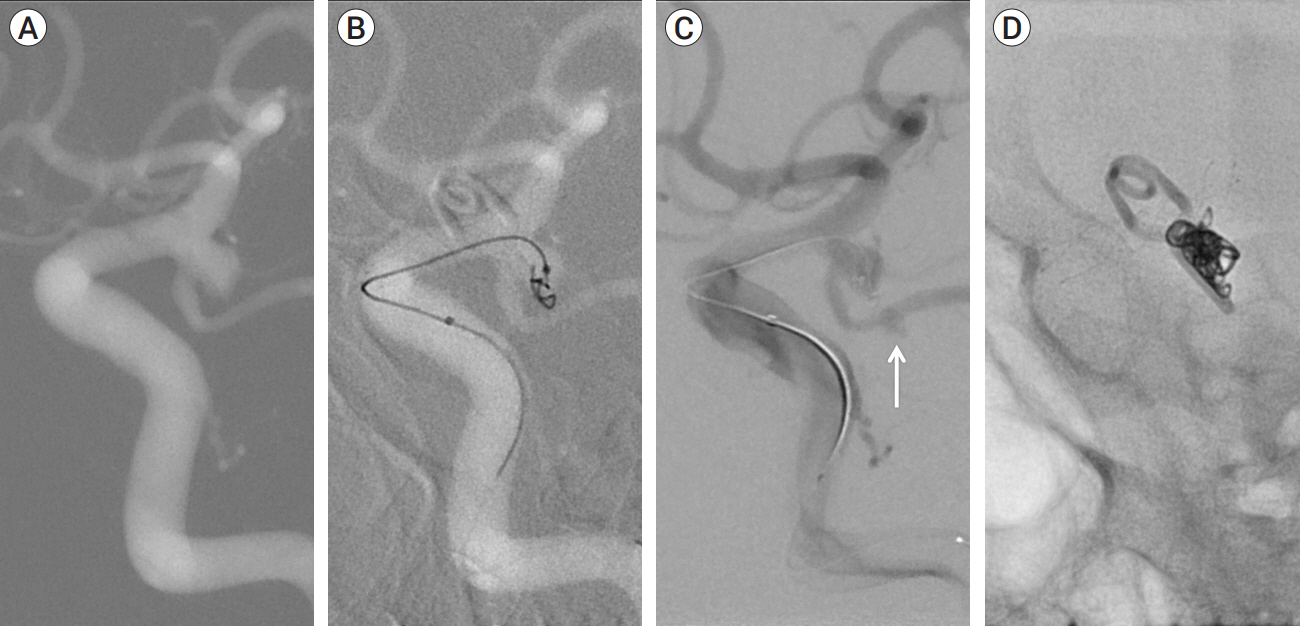
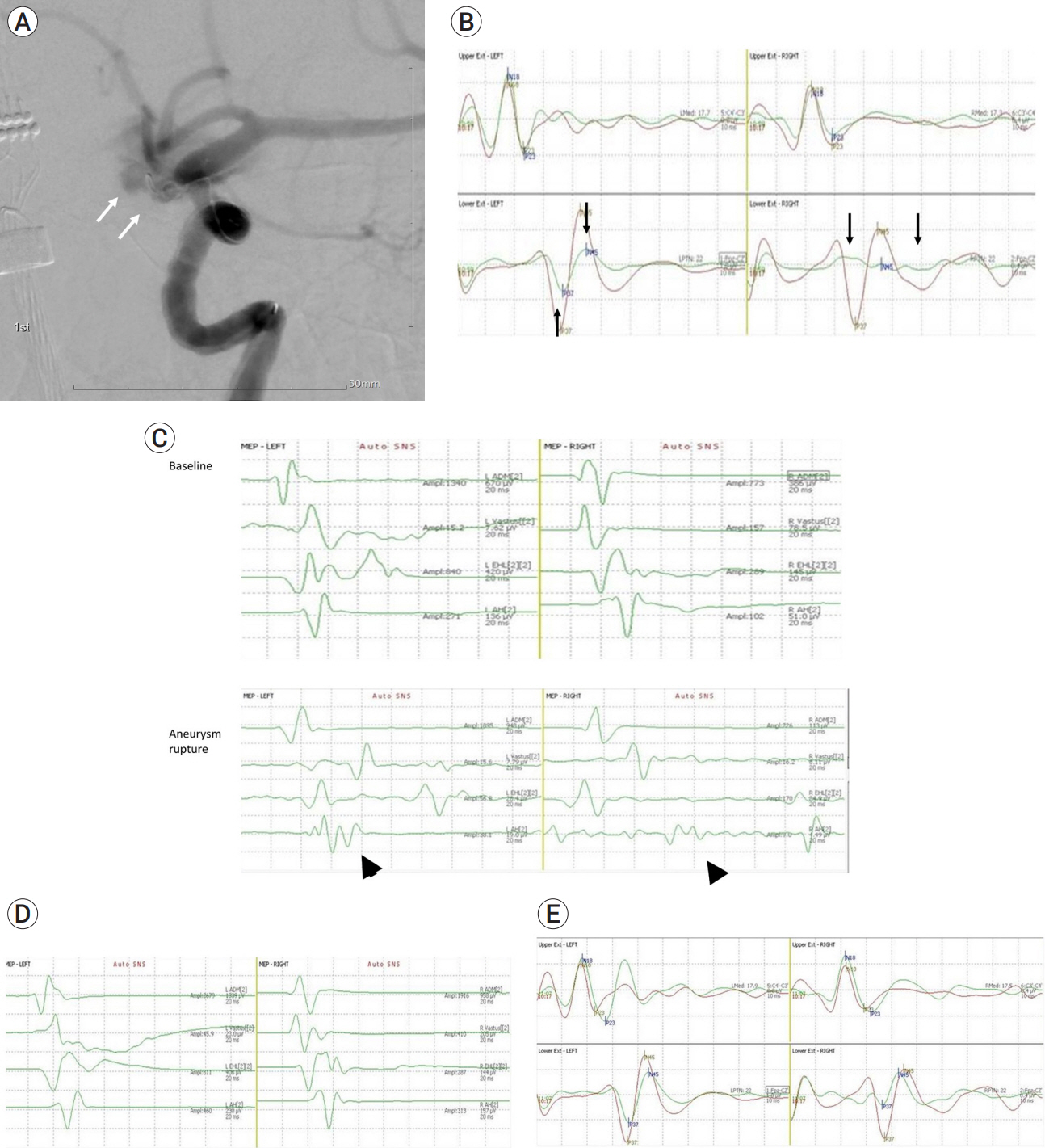
In total, 2,859 cerebral aneurysms were treated using endovascular coiling during the study period, with IPR occurring in 18 (0.63 %). IPR occurred during initial frame coiling (n=4), coil packing (n=5), stent deployment (n=7), ballooning (n=1), and microcatheter removal after coiling (n=1). Tear sites included the dome (n=14) and neck (n=4). All IPRs were controlled and treated with coil packing, with or without stenting. Flow arrest of the proximal balloon was not observed. Temporary focal neurological deficits developed in two patients (11.1%). At clinical follow-up, 14 patients were classified as modified Rankin Scale (mRS) 0, three as mRS 2, and one as mRS 4. The mean contrast leakage period of IPR was 11.2 min (range: 1-31 min). Cerebral aneurysms with IPR were divided into late (n=9, mean time: 17.11 min) and early (n=9, mean time: 5.22 min) control groups based on the criteria of 10 min of contrast leakage period. No significant between-group differences regarding clinical outcomes were observed after IPR (p=1).
Conclusions
In our series, all patients with IPR were controlled with further coil packing or stenting without proximal balloon occlusion within 31 min of contrast leakage. There was no difference in clinical outcomes when the long contrast leakage period group and short contrast leakage period group were compared.
Figure
Reference
-
1. Cho SH, Denewer M, Park W, Ahn JS, Kwun BD, Lee DH, et al. Intraprocedural rupture of unruptured cerebral aneurysms during coil embolization: A single-center experience. World Neurosurg. 2017; Sep. 105:177–83.2. Choi HH, Ha EJ, Lee JJ, Yoo DH, Cho WS, Kim JE, et al. Comparison of clinical outcomes of intracranial aneurysms: Procedural rupture versus spontaneous rupture. AJNR Am J Neuroradiol. 2017; Nov. 38(11):2126–30.3. Elijovich L, Higashida RT, Lawton MT, Duckwiler G, Giannotta S, Johnston SC. Predictors and outcomes of intraprocedural rupture in patients treated for ruptured intracranial aneurysms: The CARAT study. Stroke. 2008; May. 39(5):1501–6.4. Fan L, Lin B, Xu T, Xia N, Shao X, Tan X, et al. Predicting intraprocedural rupture and thrombus formation during coiling of ruptured anterior communicating artery aneurysms. J Neurointerv Surg. 2017; Apr. 9(4):370–5.5. Guglielmi G, Viñuela F, Sepetka I, Macellari V. Electrothrombosis of saccular aneurysms via endovascular approach. Part 1: Electrochemical basis, technique, and experimental results. J Neurosurg. 1991; Jul. 75(1):1–7.6. Kang DH, Goh DH, Baik SK, Park J, Kim YS. Morphological predictors of intraprocedural rupture during coil embolization of ruptured cerebral aneurysms: Do small basal outpouchings carry higher risk? J Neurosurg. 2014; Sep. 121(3):605–12.7. Kawabata S, Imamura H, Adachi H, Tani S, Tokunaga S, Funatsu T, et al. Risk factors for and outcomes of intraprocedural rupture during endovascular treatment of unruptured intracranial aneurysms. J Neurointerv Surg. 2018; Apr. 10(4):362–6.8. Kim ST, Baek JW, Lee WH, Lee KS, Kwon WH, Pyo S, et al. Causes of early rebleeding after coil embolization of ruptured cerebral aneurysms. Clin Neurol Neurosurg. 2018; Nov. 174:108–16.9. Kocur D, Przybyłko N, Bażowski P, Baron J. Rupture during coiling of intracranial aneurysms: Predictors and clinical outcome. Clin Neurol Neurosurg. 2018; Feb. 165:81–7.10. Lee KM, Jo KI, Jeon P, Kim KH, Kim JS, Hong SC. Predictor and prognosis of procedural rupture during coil embolization for unruptured intracranial aneurysm. J Korean Neurosurg Soc. 2016; Jan. 59(1):6–10.11. Lee S, Kim DY, Kim SB, Kim W, Kang MR, Kim HJ, et al. Predictive value of neurophysiologic monitoring during neurovascular intervention for postoperative new neurologic deficits. Neuroradiology. 2019; Feb. 61(2):207–15.12. Mitchell PJ, Muthusamy S, Dowling R, Yan B. Does small aneurysm size predict intraoperative rupture during coiling in ruptured and unruptured aneurysms? J Stroke Cerebrovasc Dis. 2013; Nov. 22(8):1298–303.13. Nuwer MR, Emerson RG, Galloway G, Legatt AD, Lopez J, Minahan R, et al. Evidence-based guideline update: intraoperative spinal monitoring with somatosensory and transcranial electrical motor evoked potentials*. J Clin Neurophysiol. 2012; Feb. 29(1):101–8.14. Park YK, Yi HJ, Choi KS, Lee YJ, Chun HJ. Intraprocedural rupture during endovascular treatment of intracranial aneurysm: Clinical results and literature review. World Neurosurg. 2018; Jun. 114:e605–15.15. Phillips JL, Chalouhi N, Jabbour P, Starke RM, Bovenzi CD, Rosenwasser RH, et al. Somatosensory evoked potential changes in neuroendovascular procedures: Incidence and association with clinical outcome in 873 patients. Neurosurgery. 2014; Nov. 75(5):560–7. discussion 566-7; quiz 567.16. Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, et al. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003; Jun. 34(6):1398–403.17. Wilent WB, Belyakina O, Korsgaard E, Tjoumakaris SI, Gooch MR, Jabbour P, et al. Intraoperative vascular complications during 2278 cerebral endovascular procedures with multimodality IONM: Relationship between signal change, complication, intervention and postoperative outcome. J Neurointerv Surg. 2021; Apr. 13(4):378–83.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Analysis of Procedural Complications of Endovascular Aneurysm Coiling with GDC
- Comprehension of Two Modalities: Endovascular Coiling and Microsurgical Clipping in Treatment of Intracranial Aneurysms
- Practical Feasibility and Packing Density of Endovascular Coiling Using Target(R) Nano(TM) Coils in Small Cerebral Aneurysms
- Treatment of the Posterior Circulation Aneurysms
- The Merits of Endovascular Coil Surgery for Patients with Unruptured Intracranial Aneurysms