J Cerebrovasc Endovasc Neurosurg.
2023 Dec;25(4):403-410. 10.7461/jcen.2023.E2023.08.009.
Safe and time-saving treatment method for acute cerebellar infarction: Navigation-guided burr-hole aspiration – 6-years single center experience
- Affiliations
-
- 1Department of Neurosurgery, Institute of Wonkwang Medical Science, Wonkwang University School of Medicine, Iksan, Korea
- KMID: 2549445
- DOI: http://doi.org/10.7461/jcen.2023.E2023.08.009
Abstract
Objective
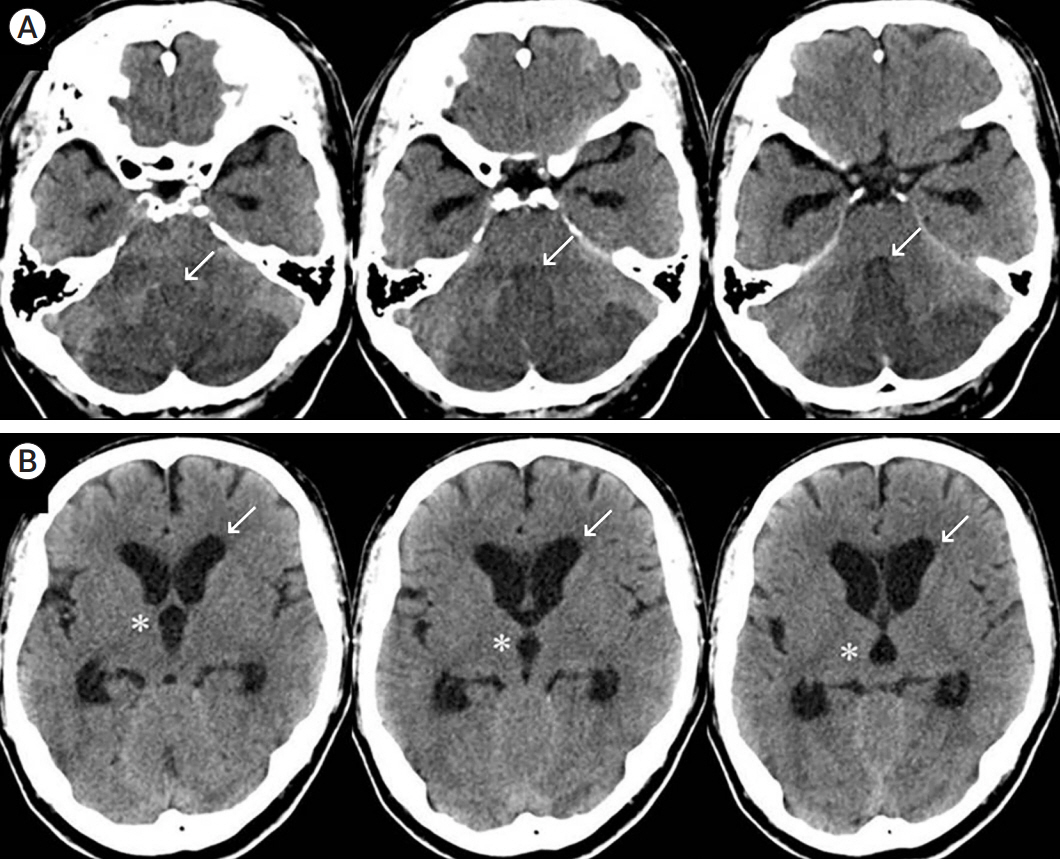
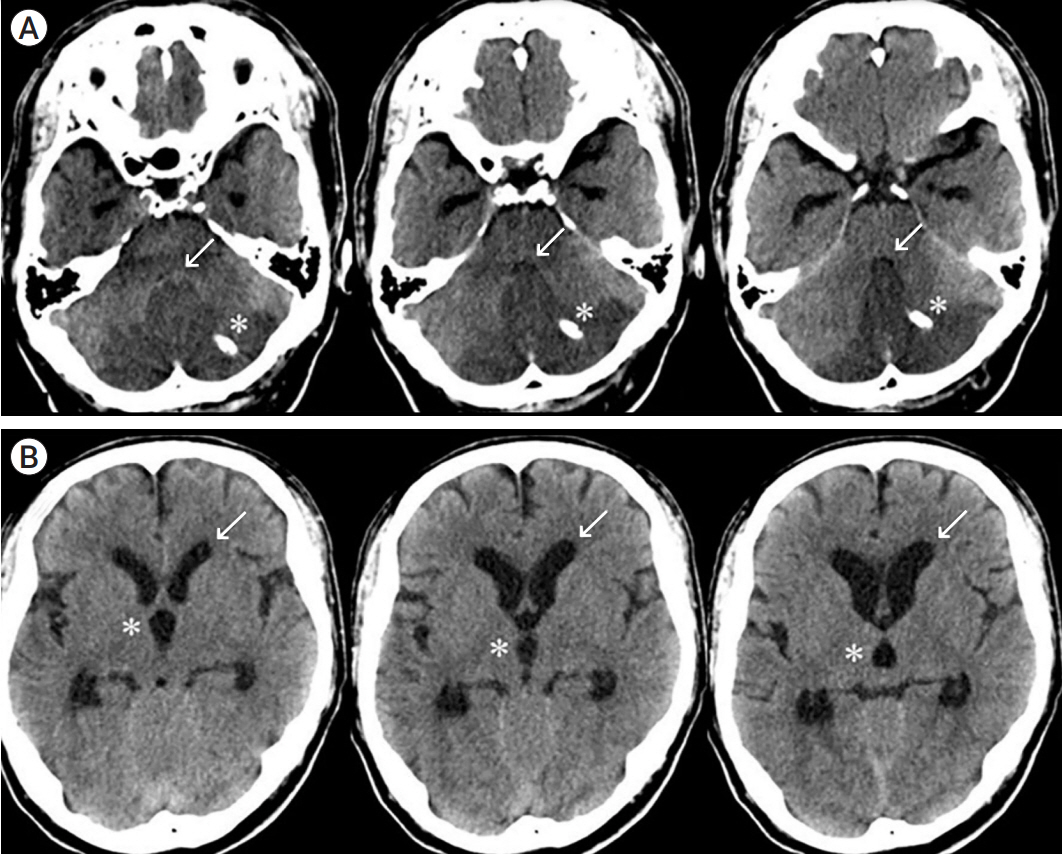
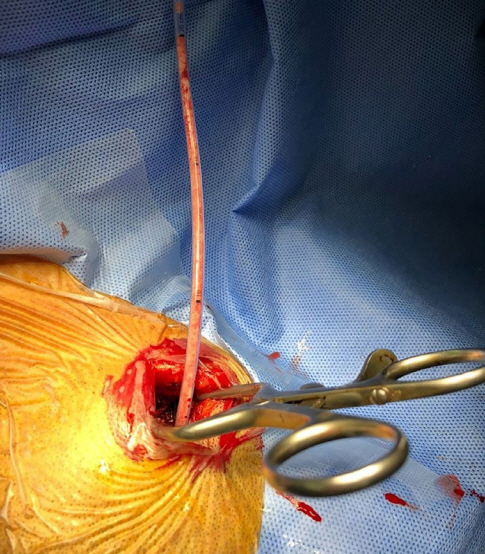
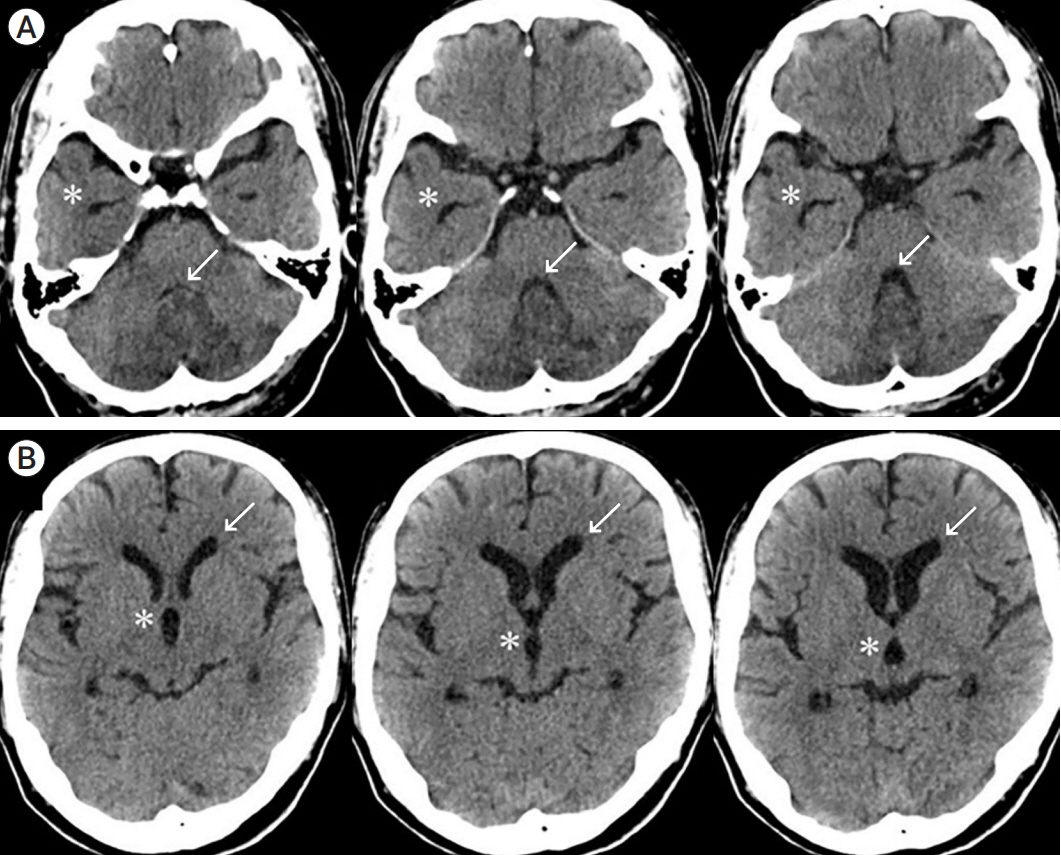
While patients with medically intractable acute cerebellar infarction typically undergo suboccipital craniectomy and removal of the infarcted tissue, this procedure is associated with long operating times and postoperative complications. This study aimed to investigate the effectiveness of minimally invasive navigationguided burr hole aspiration surgery for the treatment of acute cerebellar infarction.
Methods
Between January 2015 and December 2021, 14 patients with acute cerebellar infarction, who underwent navigation-guided burr hole aspiration surgery, were enrolled in this study.
Results
The preoperative mean Glasgow Coma Scale (GCS) score was 12.7, and the postoperative mean GCS score was 14.3. The mean infarction volume was 34.3 cc at admission and 23.5 cc immediately following surgery. Seven days after surgery, the mean infarction volume was 15.6 cc. There were no surgery-related complications during the 6-month follow-up period and no evidence of clinical deterioration. The mean operation time from skin incision to catheter insertion was 28 min, with approximately an additional 13 min for extra-ventricular drainage. The mean Glasgow Outcome Scale score after 6 months was 4.8.
Conclusions
Navigation-guided burr hole aspiration surgery is less time-consuming and invasive than conventional craniectomy, and is a safe and effective treatment option for acute cerebellar infarction in selected cases, with no surgery-related complication.
Keyword
Figure
Reference
-
1. Amar AP. Controversies in the neurosurgical management of cerebellar hemorrhage and infarction. Neurosurg Focus. 2012; Apr. 32(4):e1.2. Datar S, Rabinstein AA. Cerebellar infarction. Neurol Clin. 2014; Nov. 32(4):979–91.3. Hadanny A, Rozovski U, Nossek E, Shapira Y, Strauss I, Kanner AA, et al. Craniectomy versus craniotomy for posterior fossa metastases: Complication profile. World Neurosurg. 2016; May. 89:193–8.4. Jüttler E, Schweickert S, Ringleb PA, Huttner HB, Kohrmann M, Aschoff A. Long-term outcome after surgical treatment for space-occupying cerebellar infarction: Experience in 56 patients. Stroke. 2009; Sep. 40(9):3060–6.5. Khoshnevisan A, Allahabadi NS. Neuronavigation: Principles, clinical applications and potential pitfalls. Iran J Psychiatry. 2012; Spring. 7(2):97–103.6. Kim MJ, Park SK, Song J, Oh SY, Lim YC, Sim SY, et al. Preventive suboccipital decompressive craniectomy for cerebellar infarction: A retrospective-matched case-control study. Stroke. 2016; Oct. 47(10):2565–73.7. Koh MG, Phan TG, Atkinson JL, Wijdicks EF. Neuroimaging in deteriorating patients with cerebellar infarcts and mass effect. Stroke. 2000; Sep. 31(9):2062–7.8. Kwon WK, Park DH, Park KJ, Kang SH, Lee JH, Cho TH, et al. Prognostic factors of clinical outcome after neuronavigation-assisted hematoma drainage in patients with spontaneous intracerebral hemorrhage. Clin Neurol Neurosurg. 2014; Aug. 123:83–9.9. Lee JH, Kim DW, Kang SD. Stereotactic burr hole aspiration surgery for spontaneous hypertensive cerebellar hemorrhage. J Cerebrovasc Endovasc Neurosurg. 2012; Sep. 14(3):170–4.10. Macdonell RA, Kalnins RM, Donnan GA. Cerebellar infarction: Natural history, prognosis, and pathology. Stroke. 1987; Sep. 18(5):849–55.11. MacLullich AM, Edmond CL, Ferguson KJ, Wardlaw JM, Starr JM, Seckl JR, et al. Size of the neocerebellar vermis is associated with cognition in healthy elderly men. Brain Cogn. 2004; Dec. 56(3):344–8.12. Neugebauer H, Witsch J, Zweckberger K, Juttler E. Spaceoccupying cerebellar infarction: complications, treatment, and outcome. Neurosurg Focus. 2013; May. 34(5):e8.13. Raco A, Caroli E, Isidori A, Vangelista T, Salvati M. Management of acute cerebellar infarction: One institution’s experience. Neurosurgery. 2003; Nov. 53(5):1061–5. discussion 1065-6.14. Raz N, Rodrigue KM, Kennedy KM, Dahle C, Head D, Acker JD. Differential age-related changes in the regional metencephalic volumes in humans: A 5-year follow-up. Neurosci Lett. 2003; Oct. 349(3):163–6.15. Zhang SQ, Wang W, Ma XL, Xia YY, Liu AJ. Anticoagulation therapy is harmful to large-sized cerebellar infarction. CNS Neurosci Ther. 2014; Sep. 20(9):867–73.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Stereotactic Burr Hole Aspiration Surgery for Spontaneous Hypertensive Cerebellar Hemorrhage
- Cerebellar Hemorrhage after Burr Hole Drainage of Supratentorial Chronic Subdural Hematoma
- Delayed Cerebellar Hemorrhage after Supratentorial Burr-Hole Drainage
- Results of Surgical Treatment in Nontraumatic Deep Intracerebral Hematomas
- Burr hole drainage using urokinase for treatment of subacute subdural hematoma