J Dent Rehabil Appl Sci.
2023 Sep;39(3):119-132. 10.14368/jdras.2023.39.3.119.
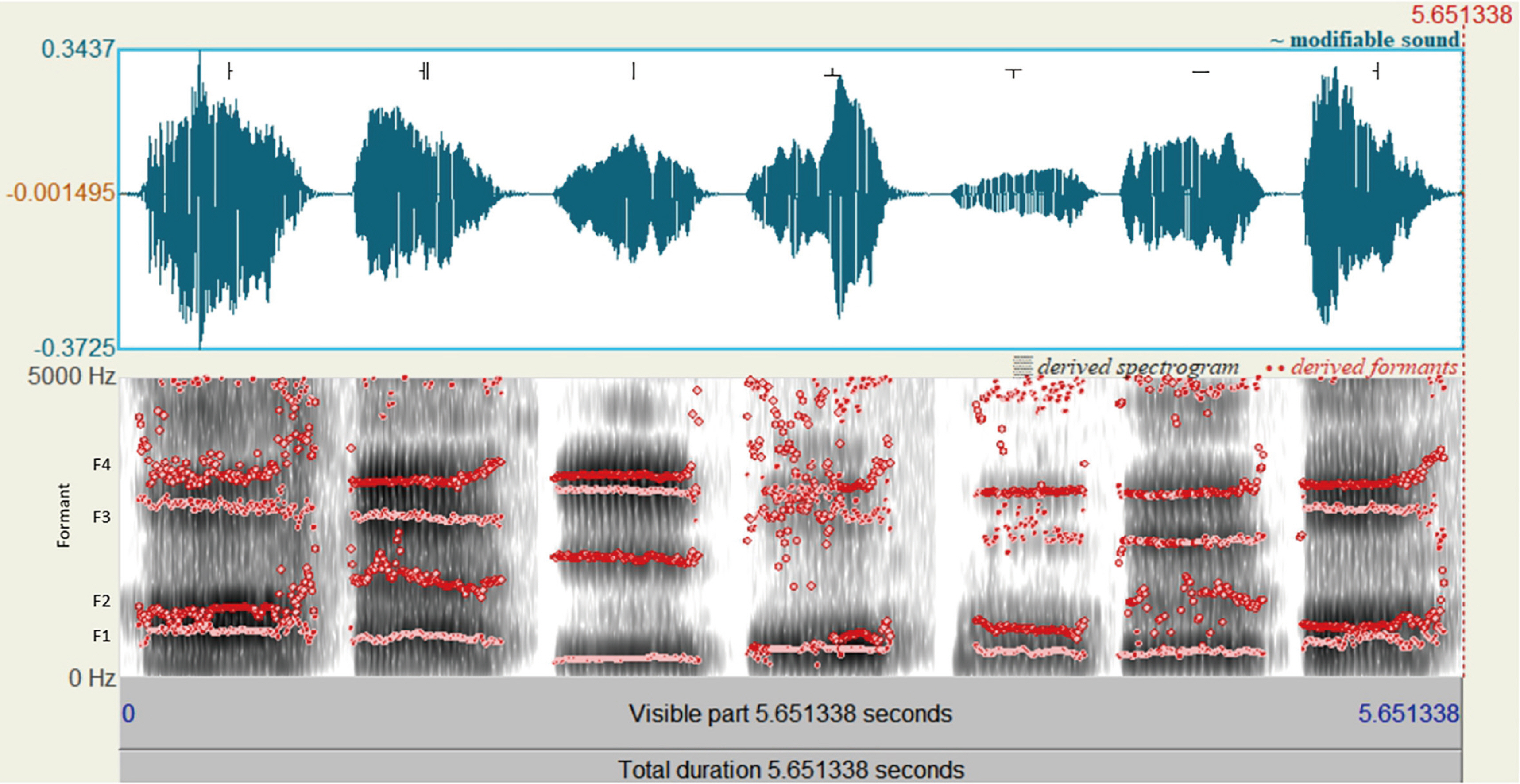
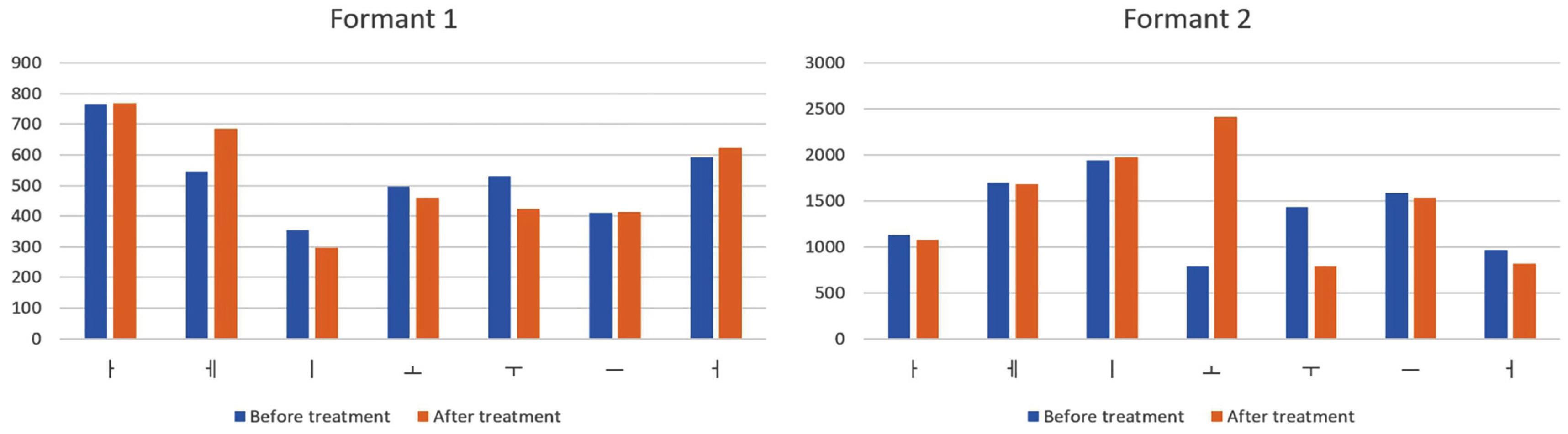
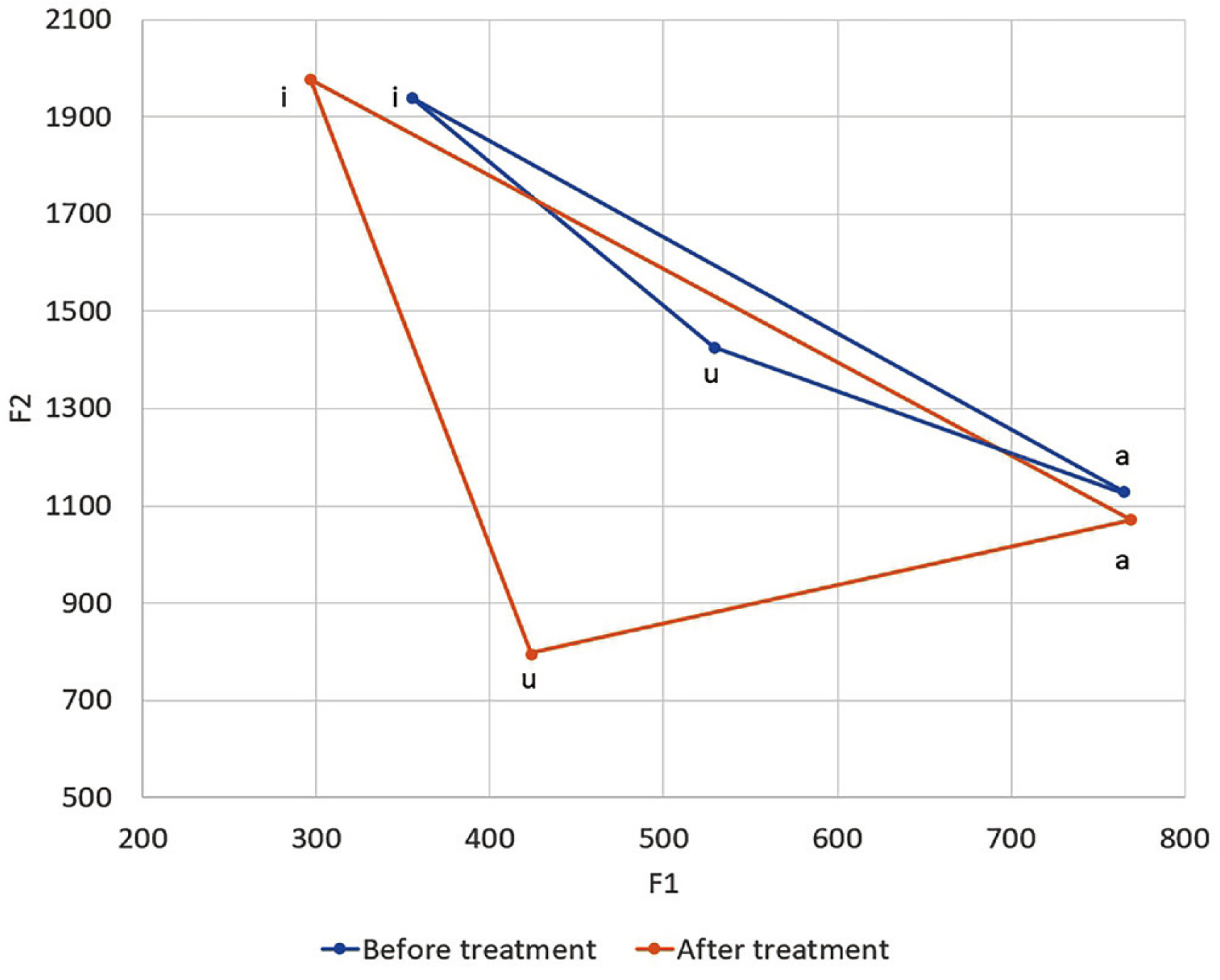
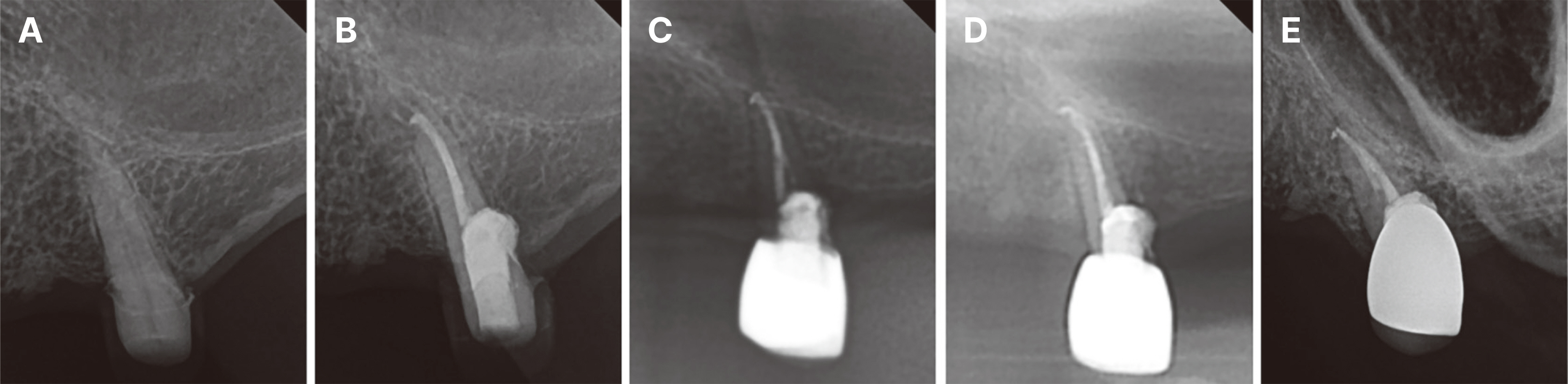
Full mouth rehabilitation accompanied by phonetic analysis of a patient with reduction of vertical dimension of occlusion, and inaccurate pronunciation due to numerous tooth loss: a case report
- Affiliations
-
- 1Division of Prosthodontics, Department of Dentistry, Asan Medical Center, Seoul, Republic of Korea
- 2Division of Prosthodontics, Department of Dentistry, Asan Medical Center, College of Medicine, University of Ulsan, Seoul, Republic of Korea
- KMID: 2549279
- DOI: http://doi.org/10.14368/jdras.2023.39.3.119
Abstract
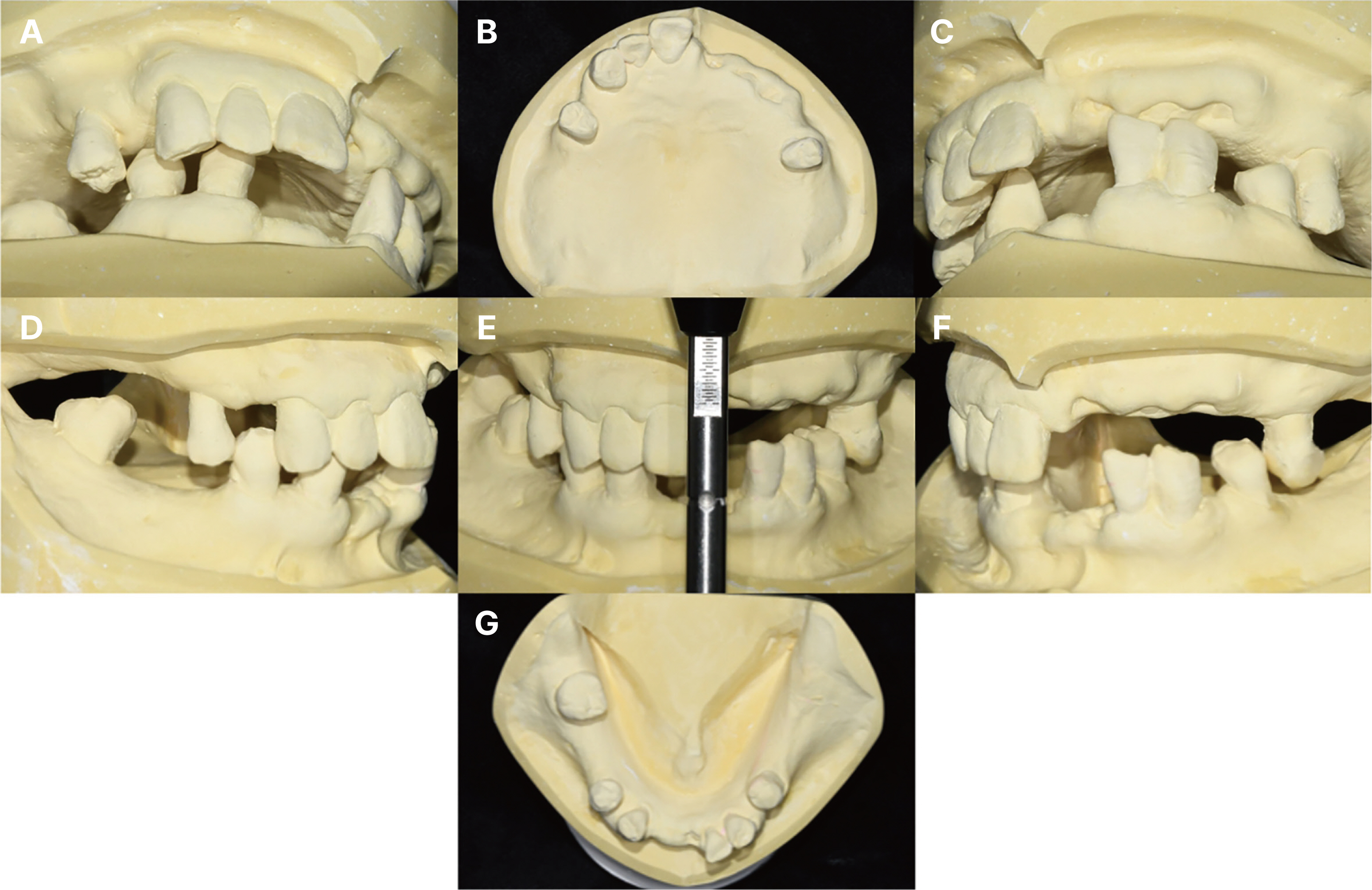
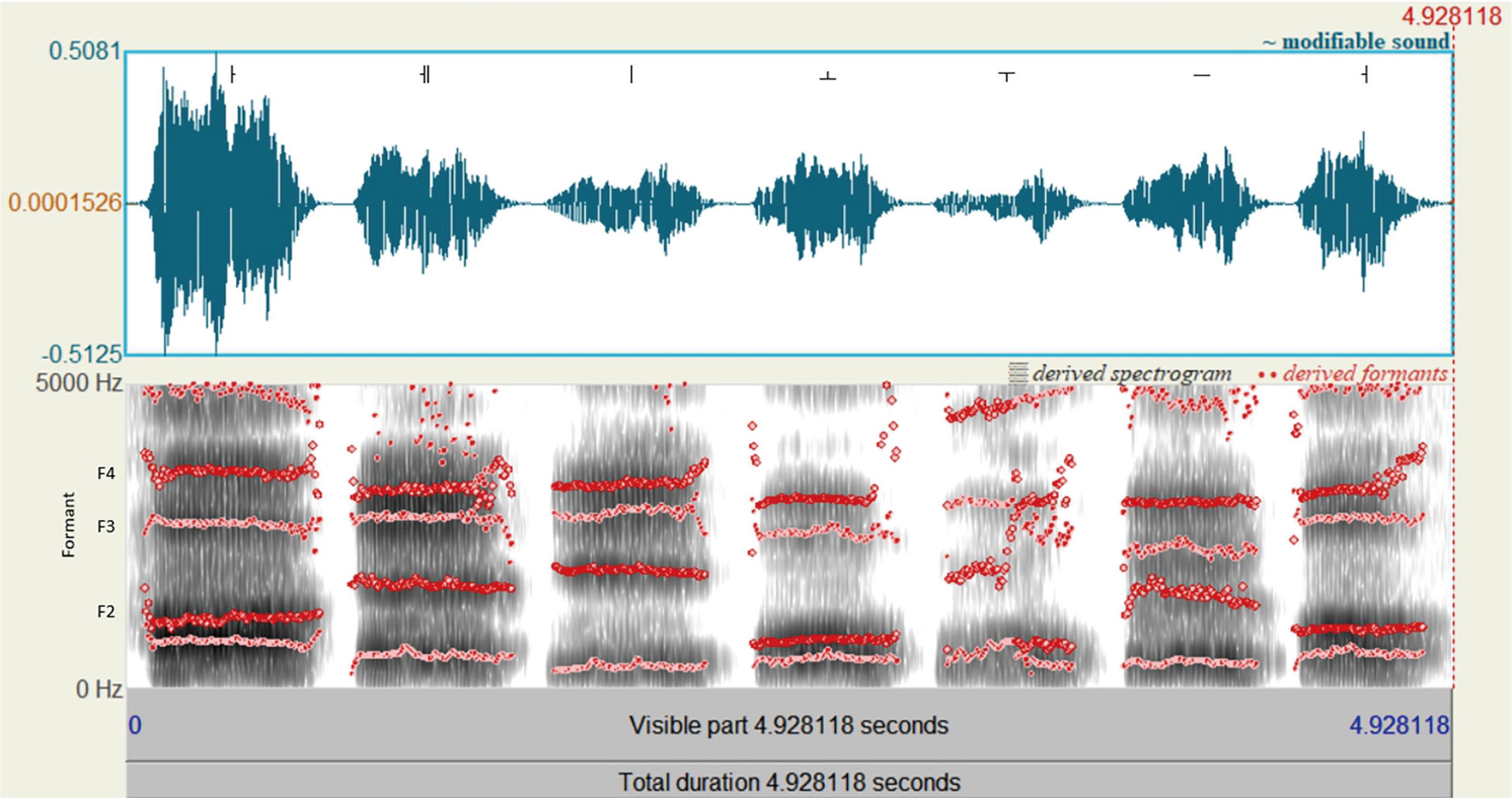
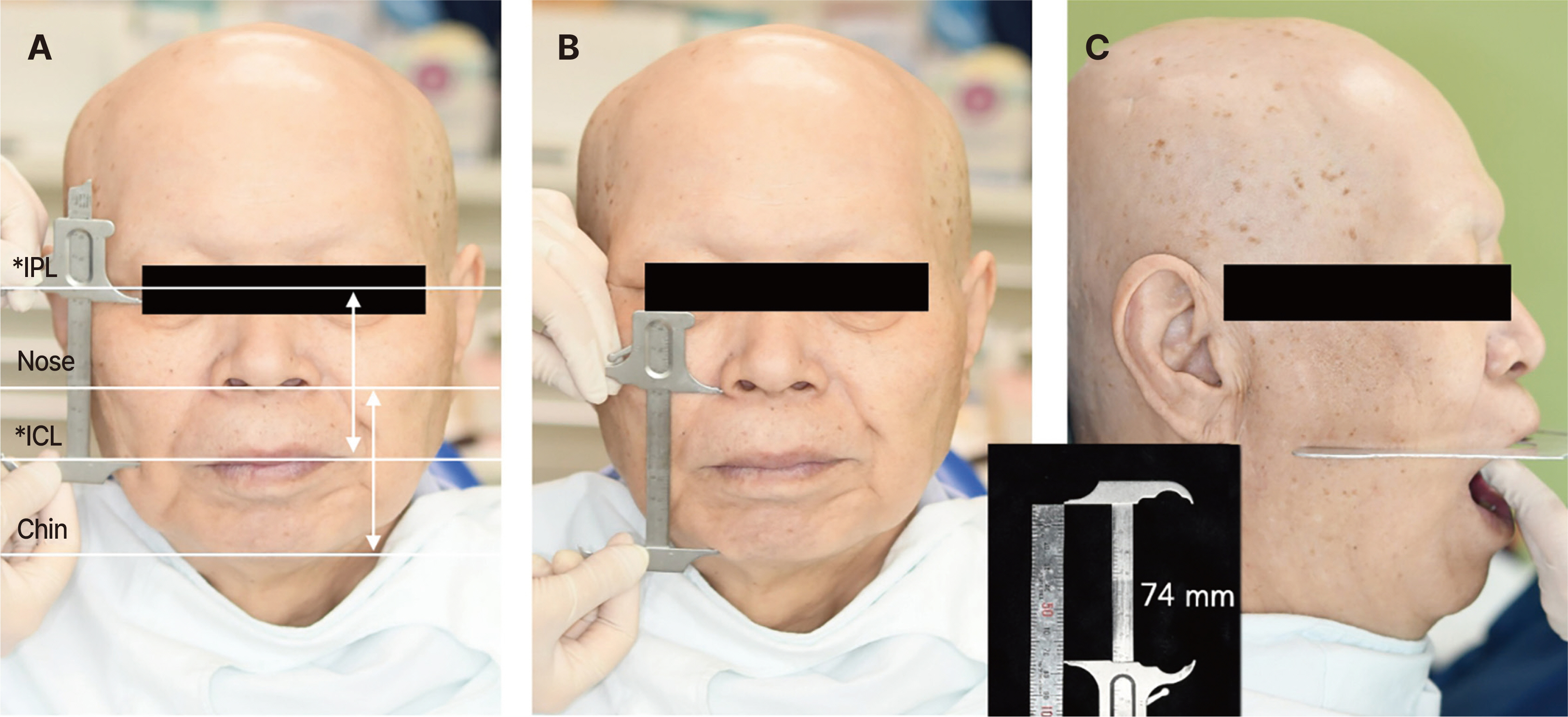
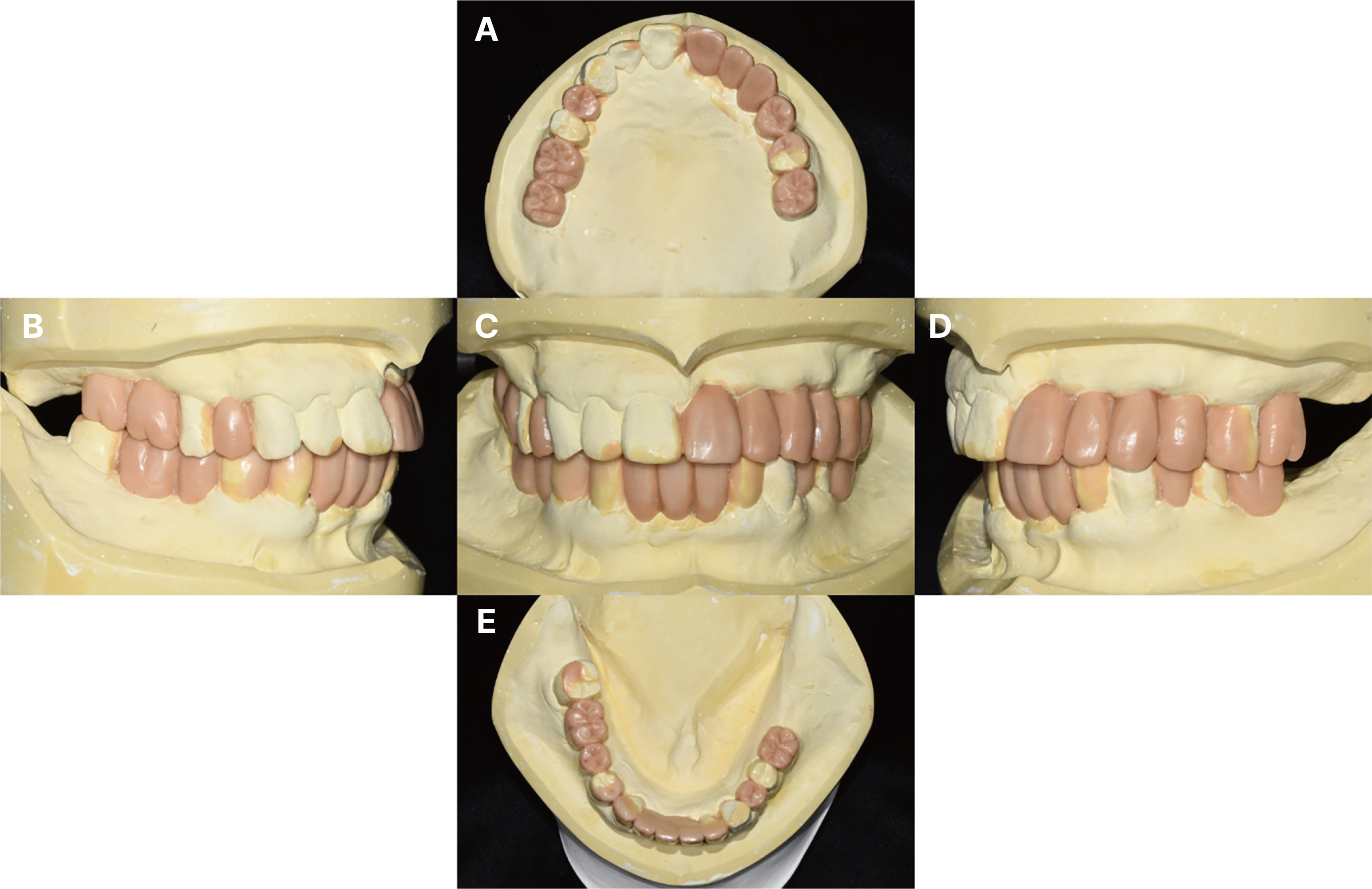
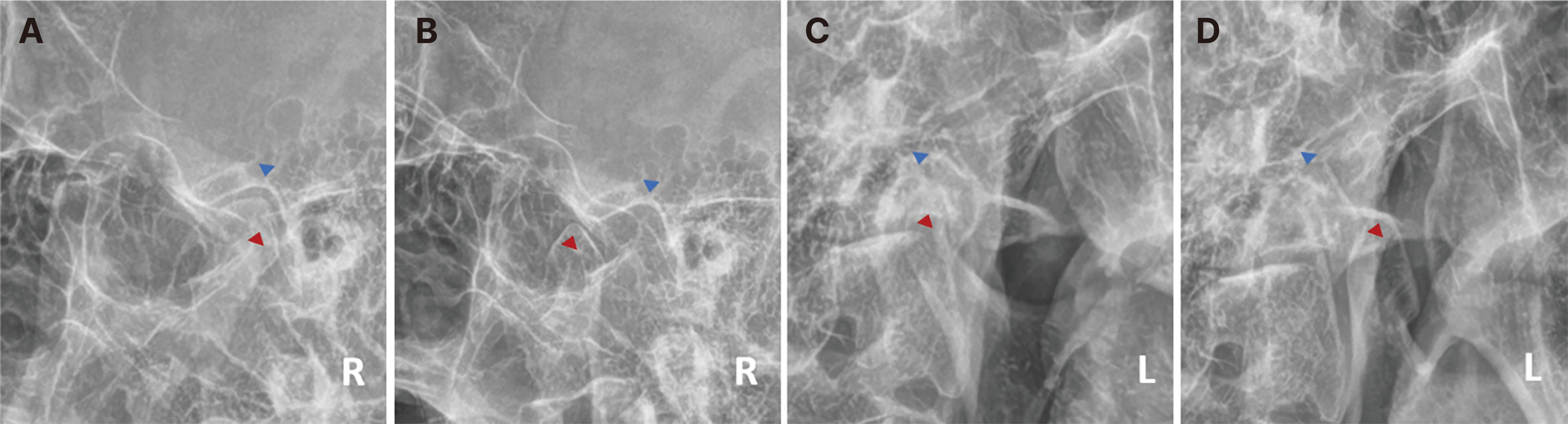
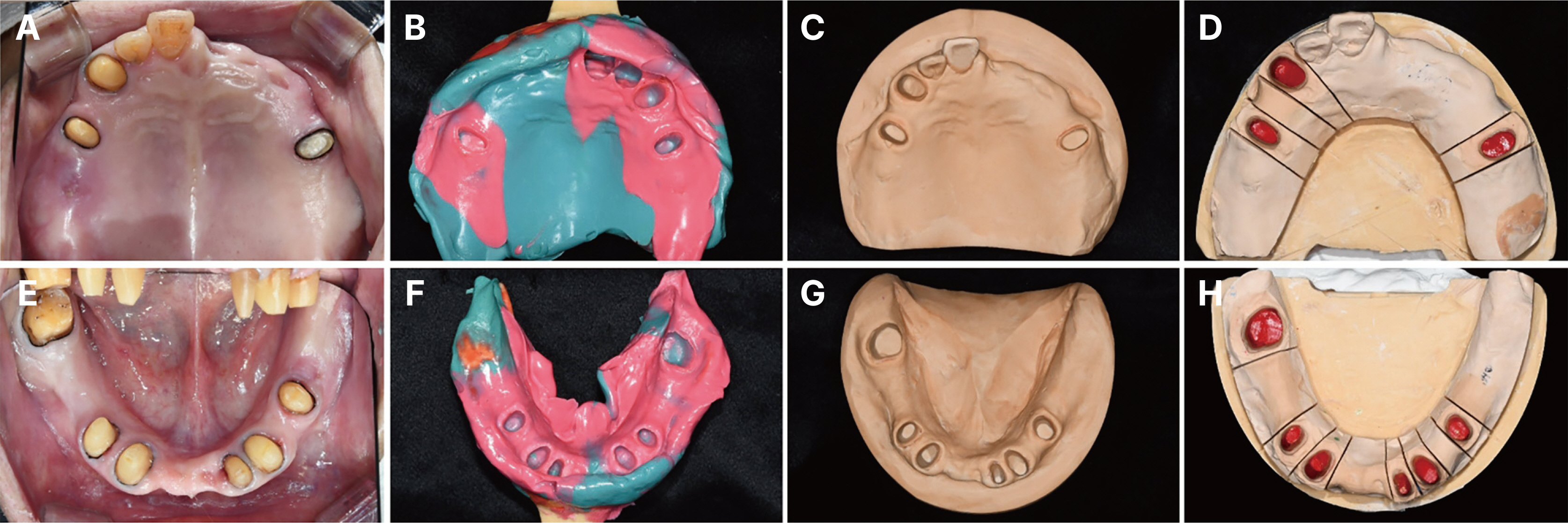
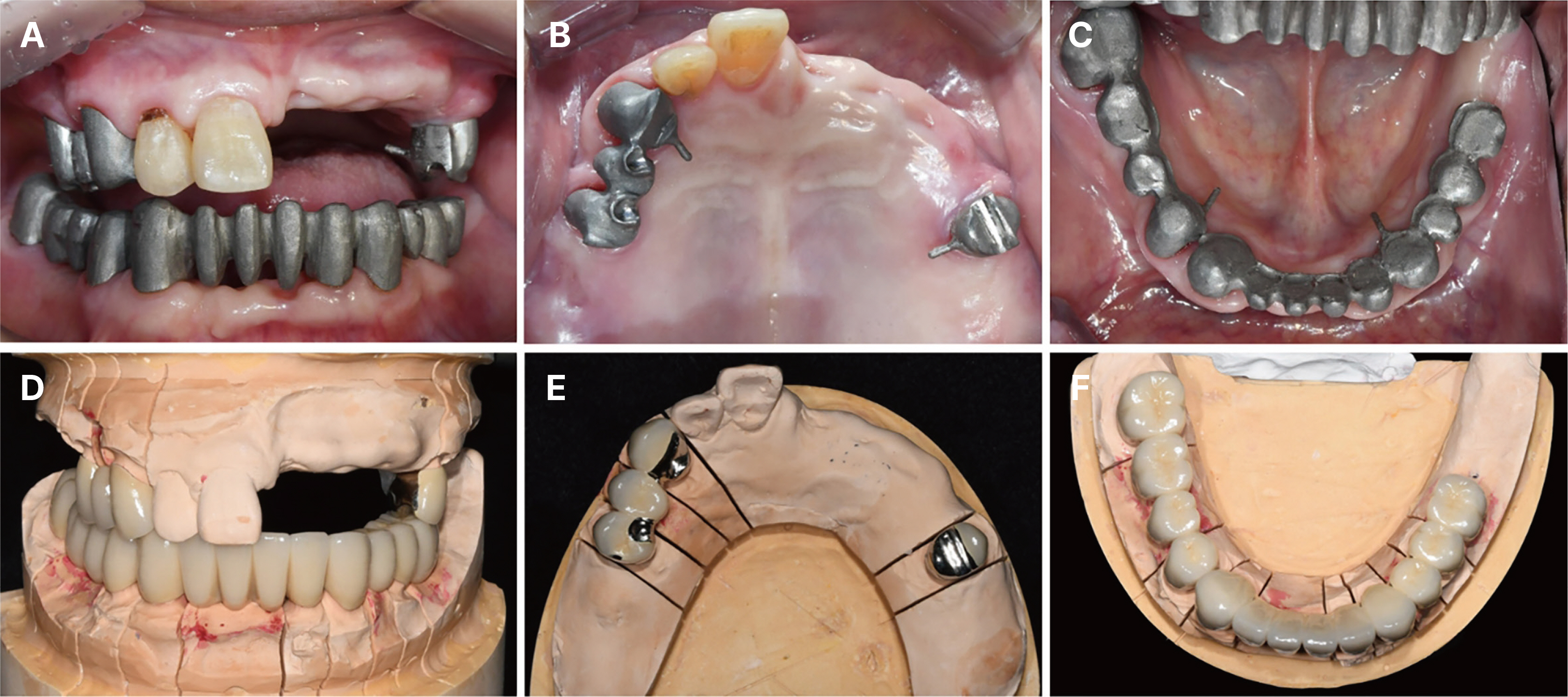
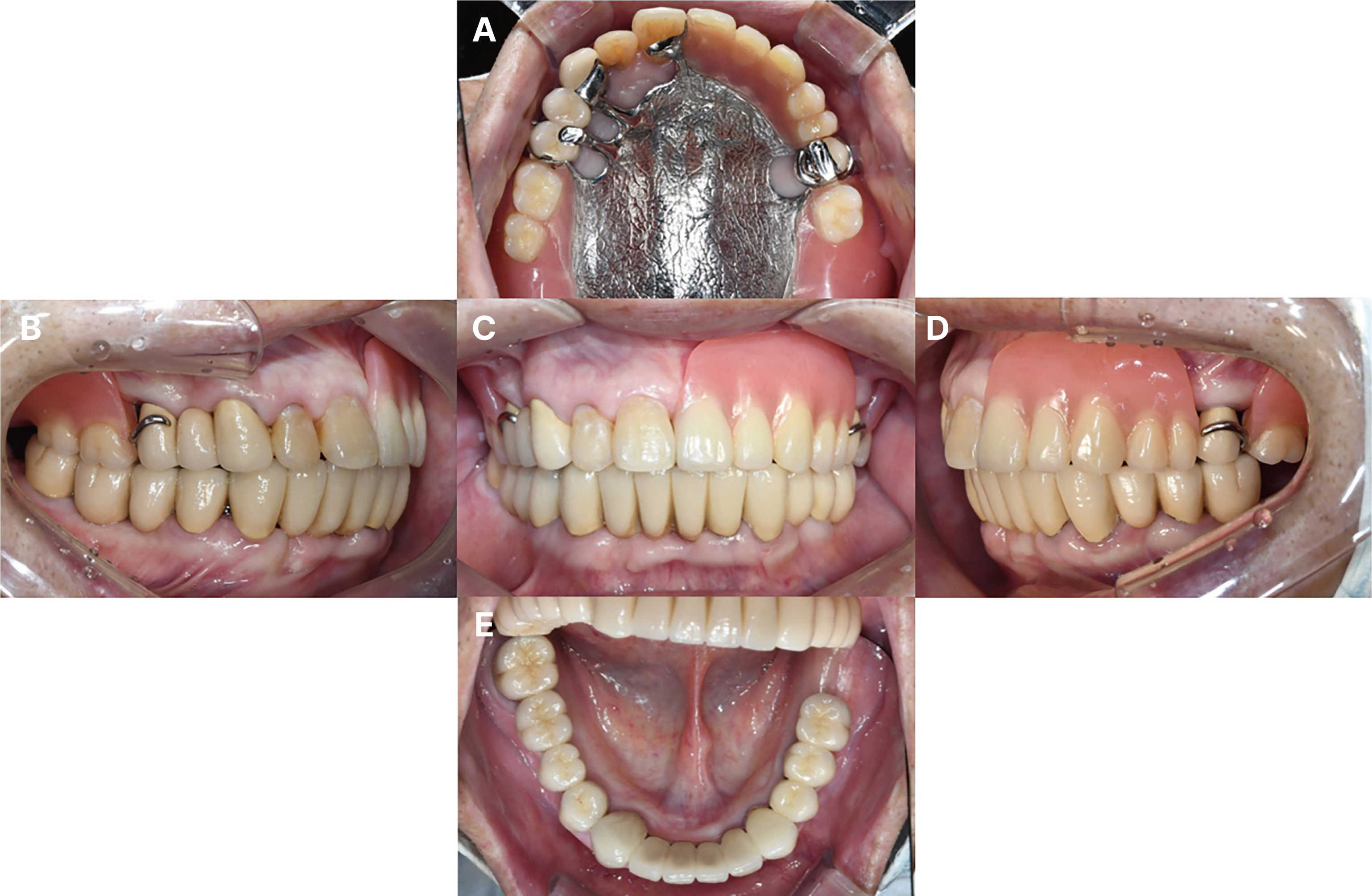
- The loss of posterior occlusal support due to tooth loss is likely to lead to compensatory protrusion and labial tilt of the anterior teeth, which may be accompanied by a deep bite and a decrease in vertical dimension. The patient may suffer from a decrease in masticatory efficiency, inaccurate pronunciation, facial appearance changes, and temporomandibular joint disorder, so stable occlusal formation with support of posterior occlusion and restoration of vertical dimension is necessary. We report the case of a patient with reduction of vertical dimension, and inaccurate pronunciation due to multiple tooth loss who underwent full mouth rehabilitation with increased vertical dimension accompanied by phonetic analysis and achieved satisfactory functional and aesthetic results.
Figure
Reference
-
References
1. Dawson PE. 2007. Functional occlusion: from TMJ to smile design. 1st ed. Mosby;St. Louis: p. 430–52. DOI: 10.4103/0972-4052.32520.2. Ramfjord SP, Blankenship JR. 1981; Increased occlusal vertical dimension in adult monkeys. J Prosthet Dent. 45:74–83. DOI: 10.1016/0022-3913(81)90015-9. PMID: 7007628.3. Sato S, Hotta TH, Pedrazzi V. 2000; Removable occlusal overlay splint in the management of tooth wear: a clinical report. J Prosthet Dent. 83:392–5. DOI: 10.1016/S0022-3913(00)70032-1. PMID: 10756287.4. Shifman A, Laufer BZ, Chweidan H. 1998; Posterior bite collapse-revisited. J Oral Rehabil. 25:376–85. DOI: 10.1046/j.1365-2842.1998.00243.x. PMID: 9639163.5. Hemmings KW, Darbar UR, Vaughan S. 2000; Tooth wear treated with direct composite restorations at an increased vertical dimension: results at 30 months. J Prosthet Dent. 83:287–93. DOI: 10.1016/S0022-3913(00)70130-2. PMID: 10709036.6. Thompson JR. 1946; The rest position of the mandible and its significance to dental science. J Am Dent Assoc. 33:151–80. DOI: 10.14219/jada.archive.1946.0034. PMID: 21010948.7. Choi YS, Lee SM. 2016; Prosthetic restoration of the patient with inaccurate pronunciation after prosthesis fabrication through systematic diagnosis and treatment procedure: A case report. J Korean Acad Prosthodont. 54:413–22. DOI: 10.4047/jkap.2016.54.4.413.8. Vaz Freitas S, Melo Pestana P, Almeida V, Ferreira A. 2015; Integrating voice evaluation: correlation between acoustic and audio-perceptual measures. J Voice. 29:390.e1–7. DOI: 10.1016/j.jvoice.2014.08.007. PMID: 25619471.9. Palmer JM. 1974; Analysis of speech in prosthodontic practice. J Prosthet Dent. 31:605–14. DOI: 10.1016/0022-3913(74)90115-2. PMID: 4524858.10. Porwal A, Sasaki K. 2013; Current status of the neutral zone: a literature review. J Prosthet Dent. 109:129–34. DOI: 10.1016/S0022-3913(13)60030-X. PMID: 23395339.11. Al-Magaleh WR, Swelem AA, Shohdi SS, Mawsouf NM. 2012; Setting up of teeth in the neutral zone and its effect on speech. Saudi Dent J. 24:43–8. DOI: 10.1016/j.sdentj.2011.11.004. PMID: 23960527. PMCID: PMC3723271.12. Willis FM. 1935; Features of the face involved in full denture prosthesis. Dent Cosmos. 77:851–4.13. Silverman MM. 2001; The speaking method in measuring vertical dimension. 1952. J Prosthet Dent. 85:427–31. DOI: 10.1067/mpr.2001.116139. PMID: 11357066.14. Park JH, Jeong CM, Jeon YC, Lim JS. 2005; A study on the occlusal plane and the vertical dimension in Korean adults with natural dentition. J Korean Acad Prosthodont. 43:41–51.15. Pang KL, Low NY, Chin KY. 2020; A review on the role of denosumab in fracture prevention. Drug Des Devel Ther. 14:4029–51. DOI: 10.2147/DDDT.S270829. PMID: 33061307. PMCID: PMC7534845.16. Kün-Darbois JD, Fauvel F. 2021; Medication-related osteonecrosis and osteoradionecrosis of the jaws: Update and current management. J Morphologie. 105:170–87. DOI: 10.1016/j.morpho.2020.11.008. PMID: 33281055.17. Brudvik JS. 1999. Advanced removable partial denture. 1st ed. Quintessence Publishing Co.;Batavia: p. 7–36.18. Kratochvil FJ. 1963; Influence of occlusal rest position and clasp design on movement of abutment teeth. J Prosthet Dent. 13:114–24. DOI: 10.1016/0022-3913(63)90204-X.19. McCracken WL. 1961; Differential diagnosis: fixed or removable partial dentures. J Am Dent Assoc. 63:767–75. DOI: 10.14219/jada.archive.1961.0294.20. Schwindling FS, Dittmann B, Rammelsberg P. 2014; Double-crown-retained removable dental prostheses: A retrospective study of survival and complications. J Prosthetic Dent. 112:488–93. DOI: 10.1016/j.prosdent.2014.02.017. PMID: 24831747.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Full mouth rehabilitation of patient with decreased occlusal vertical dimension due to severely worn dentition and posterior bite collapse
- A case of full mouth rehabilitation in patient with loss of vertical dimension and deep bite due to tooth wear
- Full mouth rehabilitation of the patient with severe tooth loss and tooth wear with vertical dimension gaining: A case report
- Full mouth rehabilitation of the patient with severely worn dentition: a case report
- Full mouth rehabilitation of a patient with excessive worn dentition by increasing vertical dimension of occlusion: a case report