Korean Circ J.
2023 Dec;53(12):813-825. 10.4070/kcj.2023.0050.
Seven-day and In-hospital Mortality According to Left and Right Ventricular Dysfunction in Patients With Septic Shock
- Affiliations
-
- 1Department of Critical Care Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 2Division of Infectious Disease, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 3Division of Pulmonology, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 4Division of Cardiology, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- KMID: 2548788
- DOI: http://doi.org/10.4070/kcj.2023.0050
Abstract
- Background and Objectives
The prognostic implications of septic cardiomyopathy have not been clearly demonstrated. We evaluated serial changes in left ventricular (LV) and right ventricular (RV) function in patients with septic shock and their prognostic value on 7-day and in-hospital mortality.
Methods
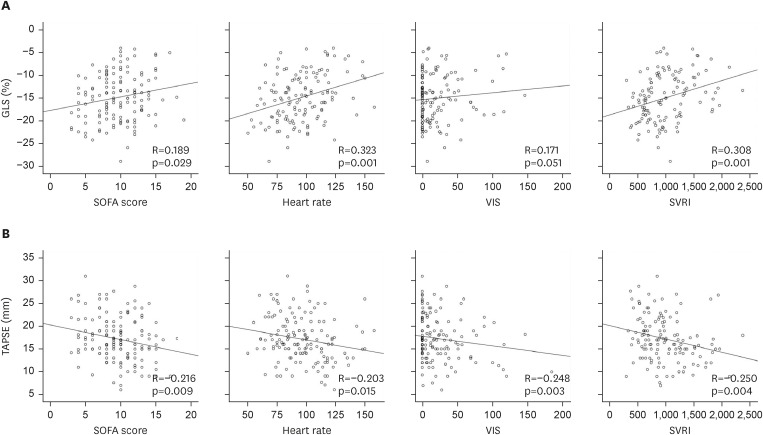
Transthoracic echocardiography was performed within 48 hours of the diagnosis of septic shock and 7 days after the initial evaluation. In addition to traditional echocardiographic parameters, LV and RV function was evaluated using global longitudinal strain (GLS), and tricuspid annular plane systolic excursion (TAPSE).
Results
A total of 162 patients (men, 83, 51.5%; 70.7±13.4 years; Acute Physiology and Chronic Health Evaluation [APACHE] II, 30.6±9.2) were enrolled. Initial GLS and TAPSE were −14.9±5.2% and 16.9±5.5 mm, and improved in the follow-up evaluation (GLS, −17.6±4.9%; TAPSE, 19.2±5.4 mm). Seven-day and in-hospital mortality were 24 (14.9%) and 64 (39.8%). Seven-day mortality was significantly associated with initial GLS >−16% (odds ratio [OR], 14.066, 95% confidence interval [CI], 1.178–167.969, p=0.037) and APACHE II score (OR, 1.196, 95% CI, 1.047–1.365, p=0.008). The in-hospital mortality of 7-day survivors was associated with follow-up TAPSE <16 mm (OR, 10.109, 95% CI, 1.640–62.322, p=0.013) and Sequential Organ Failure Assessment score (OR, 1.340, 95% CI, 1.078–1.667, p=0.008). GLS was not associated with in-hospital mortality of 7-day survivors.
Conclusions
Fluctuation of both ventricular function was common in septic shock. Sevenday mortality of patients with septic shock was related to GLS, whereas in-hospital mortality of 7-day survivors was related to TAPSE, not to GLS.
Keyword
Figure
Reference
-
1. Pulido JN, Afessa B, Masaki M, et al. Clinical spectrum, frequency, and significance of myocardial dysfunction in severe sepsis and septic shock. Mayo Clin Proc. 2012; 87:620–628. PMID: 22683055.2. Charpentier J, Luyt CE, Fulla Y, et al. Brain natriuretic peptide: a marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004; 32:660–665. PMID: 15090944.3. Ehrman RR, Sullivan AN, Favot MJ, et al. Pathophysiology, echocardiographic evaluation, biomarker findings, and prognostic implications of septic cardiomyopathy: a review of the literature. Crit Care. 2018; 22:112. PMID: 29724231.4. Martin L, Derwall M, Al Zoubi S, et al. The septic heart: current understanding of molecular mechanisms and clinical implications. Chest. 2019; 155:427–437. PMID: 30171861.5. Lee MT, Jung SY, Baek MS, Shin J, Kim WY. Early vitamin C, hydrocortisone, and thiamine treatment for septic cardiomyopathy: a propensity score analysis. J Pers Med. 2021; 11:610. PMID: 34203183.6. Bréchot N, Hajage D, Kimmoun A, et al. Venoarterial extracorporeal membrane oxygenation to rescue sepsis-induced cardiogenic shock: a retrospective, multicentre, international cohort study. Lancet. 2020; 396:545–552. PMID: 32828186.7. Hollenberg SM, Singer M. Pathophysiology of sepsis-induced cardiomyopathy. Nat Rev Cardiol. 2021; 18:424–434. PMID: 33473203.8. De Backer D, Cecconi M, Lipman J, et al. Challenges in the management of septic shock: a narrative review. Intensive Care Med. 2019; 45:420–433. PMID: 30741328.9. Kakihana Y, Ito T, Nakahara M, Yamaguchi K, Yasuda T. Sepsis-induced myocardial dysfunction: pathophysiology and management. J Intensive Care. 2016; 4:22. PMID: 27011791.10. Malbrain ML, Van Regenmortel N, Saugel B, et al. Principles of fluid management and stewardship in septic shock: it is time to consider the four D’s and the four phases of fluid therapy. Ann Intensive Care. 2018; 8:66. PMID: 29789983.11. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016; 315:801–810. PMID: 26903338.12. Ruopp MD, Perkins NJ, Whitcomb BW, Schisterman EF. Youden Index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J. 2008; 50:419–430. PMID: 18435502.13. Smith LM, Yoza BK, Hoth JJ, McCall CE, Vachharajani V. SIRT1 mediates septic cardiomyopathy in a murine model of polymicrobial sepsis. Shock. 2020; 54:96–101. PMID: 31393272.14. Boyd JH, Mathur S, Wang Y, Bateman RM, Walley KR. Toll-like receptor stimulation in cardiomyoctes decreases contractility and initiates an NF-κB dependent inflammatory response. Cardiovasc Res. 2006; 72:384–393. PMID: 17054926.15. Haileselassie B, Mukherjee R, Joshi AU, et al. Drp1/Fis1 interaction mediates mitochondrial dysfunction in septic cardiomyopathy. J Mol Cell Cardiol. 2019; 130:160–169. PMID: 30981733.16. Zanotti-Cavazzoni SL, Hollenberg SM. Cardiac dysfunction in severe sepsis and septic shock. Curr Opin Crit Care. 2009; 15:392–397. PMID: 19633546.17. Ince C, Mayeux PR, Nguyen T, et al. The endothelium in sepsis. Shock. 2016; 45:259–270. PMID: 26871664.18. Bazalgette F, Roger C, Louart B, et al. Prognostic value and time course evolution left ventricular global longitudinal strain in septic shock: an exploratory prospective study. J Clin Monit Comput. 2021; 35:1501–1510. PMID: 33216237.19. Ng PY, Sin WC, Ng AK, Chan WM. Speckle tracking echocardiography in patients with septic shock: a case control study (SPECKSS). Crit Care. 2016; 20:145. PMID: 27177587.20. Zhang HM, Wang XT, Zhang LN, et al. Left ventricular longitudinal systolic function in septic shock patients with normal ejection fraction: a case-control study. Chin Med J (Engl). 2017; 130:1169–1174. PMID: 28485316.21. Chang WT, Lee WH, Lee WT, et al. Left ventricular global longitudinal strain is independently associated with mortality in septic shock patients. Intensive Care Med. 2015; 41:1791–1799. PMID: 26183489.22. Sanfilippo F, Corredor C, Fletcher N, et al. Left ventricular systolic function evaluated by strain echocardiography and relationship with mortality in patients with severe sepsis or septic shock: a systematic review and meta-analysis. Crit Care. 2018; 22:183. PMID: 30075792.23. Hai PD, Binh NT, Hien NV, et al. Prognostic role of left ventricular systolic function measured by speckle tracking echocardiography in septic shock. BioMed Res Int. 2020; 2020:7927353. PMID: 33150180.24. Sanz J, Sánchez-Quintana D, Bossone E, Bogaard HJ, Naeije R. Anatomy, function, and dysfunction of the right ventricle: JACC state-of-the-art review. J Am Coll Cardiol. 2019; 73:1463–1482. PMID: 30922478.25. Lanspa MJ, Cirulis MM, Wiley BM, et al. Right ventricular dysfunction in early sepsis and septic shock. Chest. 2021; 159:1055–1063. PMID: 33068615.26. Singh RK, Kumar S, Nadig S, et al. Right heart in septic shock: prospective observational study. J Intensive Care. 2016; 4:38. PMID: 27280022.27. Vallabhajosyula S, Shankar A, Vojjini R, et al. Impact of right ventricular dysfunction on short-term and long-term mortality in sepsis: a meta-analysis of 1,373 patients. Chest. 2021; 159:2254–2263. PMID: 33359215.28. Carluccio E, Biagioli P, Alunni G, et al. Prognostic value of right ventricular dysfunction in heart failure with reduced ejection fraction: superiority of longitudinal strain over tricuspid annular plane systolic excursion. Circ Cardiovasc Imaging. 2018; 11:e006894. PMID: 29321212.29. van Diepen S, Katz JN, Albert NM, et al. Contemporary management of cardiogenic shock: a scientific statement from the American Heart Association. Circulation. 2017; 136:e232–e268. PMID: 28923988.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between Left Ventricular Systolic Dysfunction and Mortality in Patients with Septic Shock
- The Clinical Value of TnI and BNP for the Evaluation of Sepsis-related Cardiac Dysfunction in the Emergency Department
- Mortality among adult patients with sepsis and septic shock in Korea: a systematic review and meta-analysis
- Association between high-sensitivity troponin test and tissue Doppler assessment of left ventricular diastolic dysfunction in critically ill septic patients
- Validation of Immature Granulocyte as a Predictor for the 28-Day Mortality in Patients with Severe Sepsis and Septic Shock