Arch Hand Microsurg.
2023 Dec;28(4):296-301. 10.12790/ahm.23.0029.
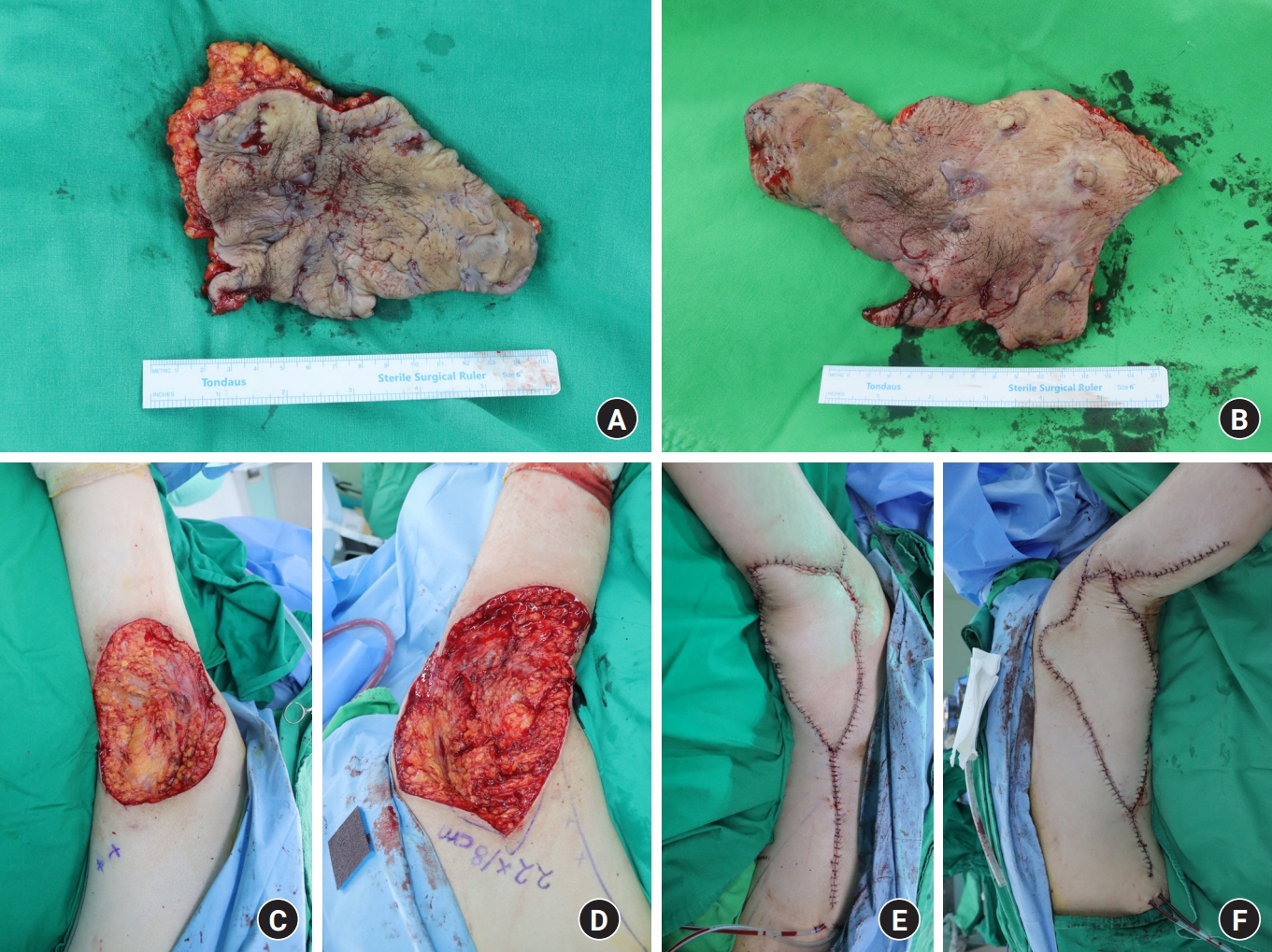
The treatment of axillary hidradenitis suppurativa with a thoracodorsal artery perforator V-Y advancement flap: a case report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Jeonbuk National University Hospital, Jeonju, Korea
- KMID: 2548602
- DOI: http://doi.org/10.12790/ahm.23.0029
Abstract
- Hidradenitis suppurativa, a recurrent and chronic inflammatory skin disease, presents with extensive scars and multiple abscesses. Moreover, axillary hidradenitis suppurativa could be impacted by scar contracture, which can limit arm mobility. The most reliable treatment for advanced hidradenitis suppurativa is meticulous and radical excision. Several methods exist for the reconstruction of axillary wounds after reconstruction. Skin grafts are an option, but their drawbacks include secondary contracture and poor aesthetic results. Local flaps could be useful, but also have a limited arc of rotation for larger defects. Thoracodorsal artery perforator (TDAP) flaps have been proven to be very effective as part of the armamentarium for axillary wounds. Herein, we describe the use of a TDAP flap in a V-Y advancement fashion with minimal pedicle dissection. We only dissected the perforator pedicle about 1 to 2 cm from its muscle entry point. With this maneuver, the flap could be easily moved to cover the defect without vascular compromise. We found that the TDAP flap performed in a V-Y fashion, with a propeller design, was very useful for an axillary defect over an island. This procedure was simple, easy, and time-saving.
Figure
Reference
-
References
1. Saunte DM, Jemec GB. Hidradenitis suppurativa: advances in diagnosis and treatment. JAMA. 2017; 318:2019–32.2. Flood KS, Porter ML, Kimball AB. Biologic treatment for hidradenitis suppurativa. Am J Clin Dermatol. 2019; 20:625–38.
Article3. Slade DE, Powell BW, Mortimer PS. Hidradenitis suppurativa: pathogenesis and management. Br J Plast Surg. 2003; 56:451–61.
Article4. Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: Part I: Diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019; 81:76–90.
Article5. Busnardo FF, Coltro PS, Olivan MV, Busnardo AP, Ferreira MC. The thoracodorsal artery perforator flap in the treatment of axillary hidradenitis suppurativa: effect on preservation of arm abduction. Plast Reconstr Surg. 2011; 128:949–53.6. Taylor EM, Hamaguchi R, Kramer KM, Kimball AB, Orgill DP. Plastic surgical management of hidradenitis suppurativa. Plast Reconstr Surg. 2021; 147:479–91.
Article7. Hamdi M, Van Landuyt K, Hijjawi JB, Roche N, Blondeel P, Monstrey S. Surgical technique in pedicled thoracodorsal artery perforator flaps: a clinical experience with 99 patients. Plast Reconstr Surg. 2008; 121:1632–41.
Article8. Angrigiani C, Grilli D, Siebert J. Latissimus dorsi musculocutaneous flap without muscl. Plast Reconstr Surg. 1995; 96:1608–14.9. Wormald JC, Balzano A, Clibbon JJ, Figus A. Surgical treatment of severe hidradenitis suppurativa of the axilla: thoracodorsal artery perforator (TDAP) flap versus split skin graft. J Plast Reconstr Aesthet Surg. 2014; 67:1118–24.
Article10. Baudet J, Guimberteau JC, Nascimento E. Successful clinical transfer of two free thoraco-dorsal axillary flaps. Plast Reconstr Surg. 1976; 58:680–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of the Soft Tissue Defect Using Thoracodorsal Artery Perforator Skin Flap
- A Case of Hidradenitis Suppurativa
- Axillary Reconstruction Using a Pedicled Thoracodorsal Artery Perforator Flap Including Latissimus Dorsi Muscle Strip
- Surgical treatment of postauricular hidradenitis suppurativa with delayed diagnosis: a case report and literature review
- Skin Infection Caused by Serratia marcescens in an Immunocompetent Patient with Hidradenitis Suppurativa