Arch Hand Microsurg.
2023 Dec;28(4):211-225. 10.12790/ahm.23.0024.
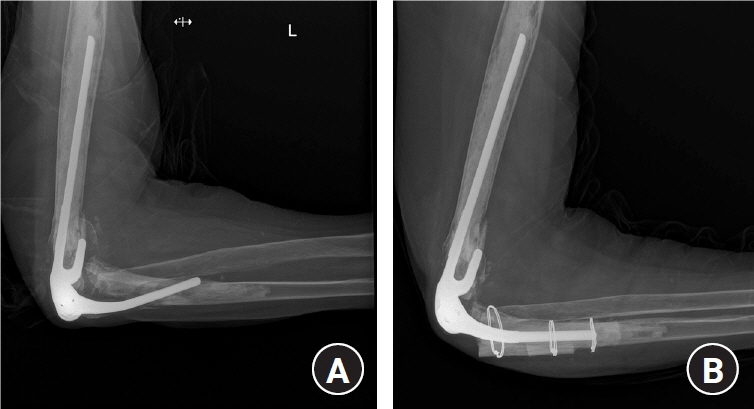
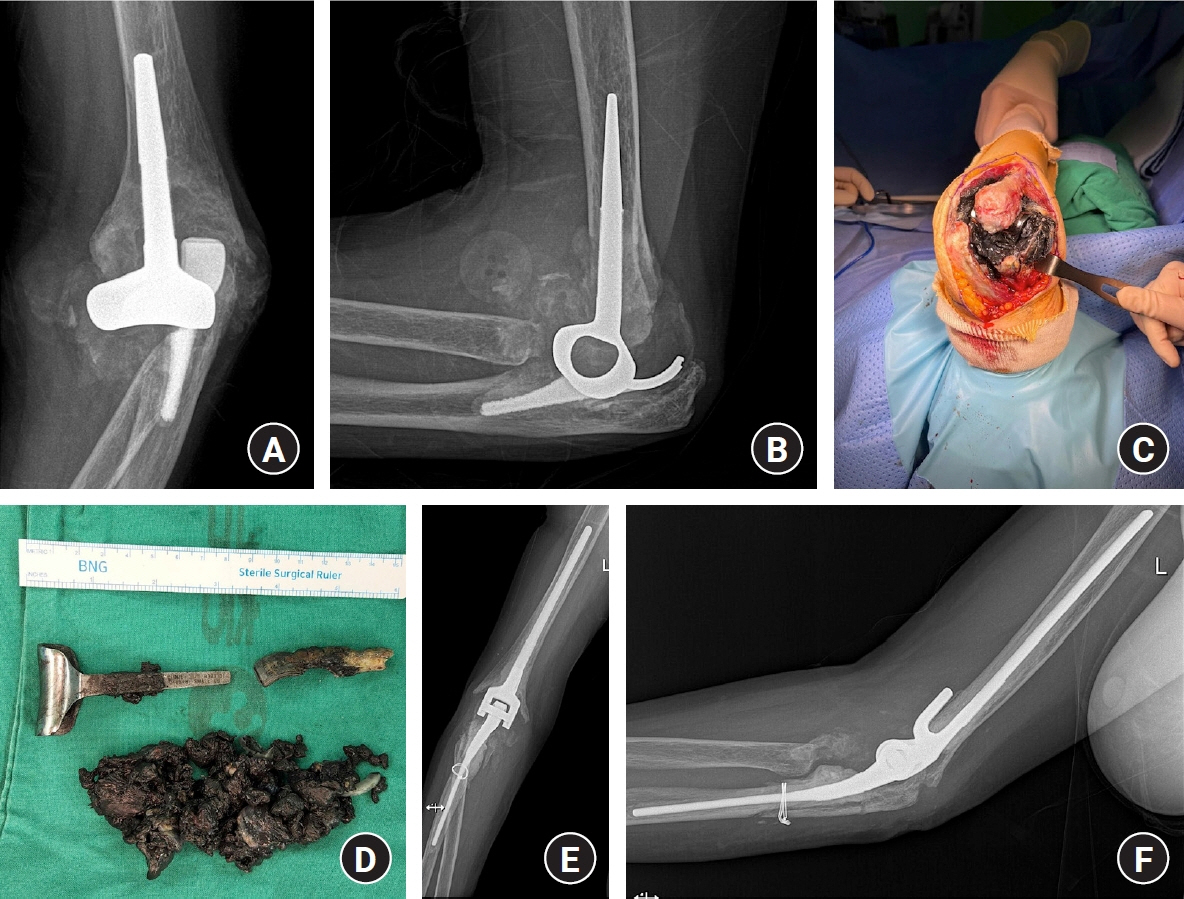
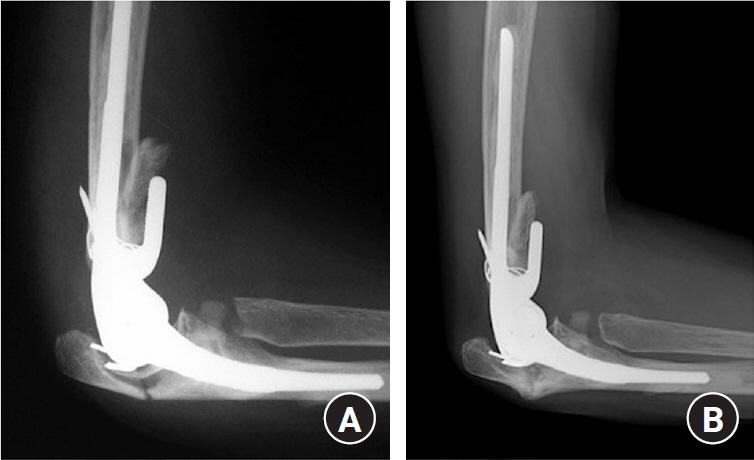
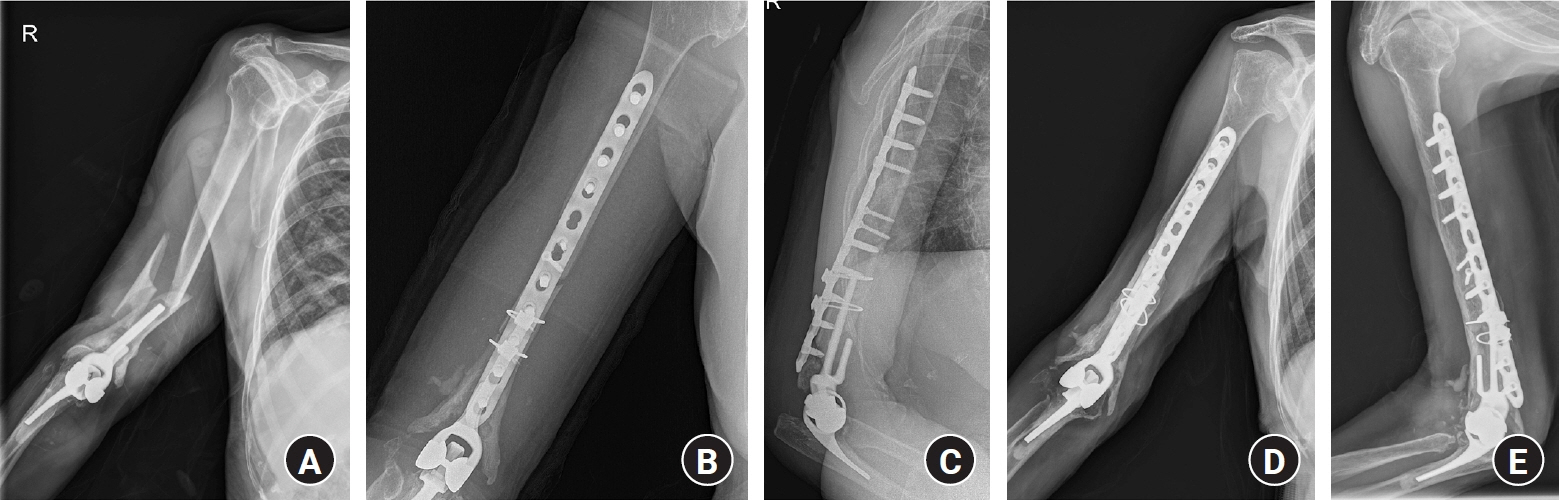
Complications of total elbow arthroplasty
- Affiliations
-
- 1Department of Orthopedic Surgery, Regional Rheumatoid and Degenerative Arthritis Center, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea
- KMID: 2548592
- DOI: http://doi.org/10.12790/ahm.23.0024
Abstract
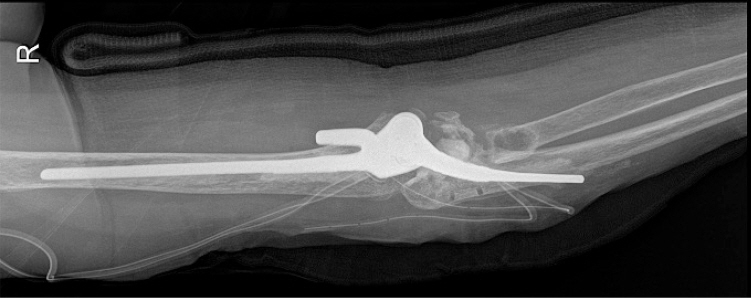
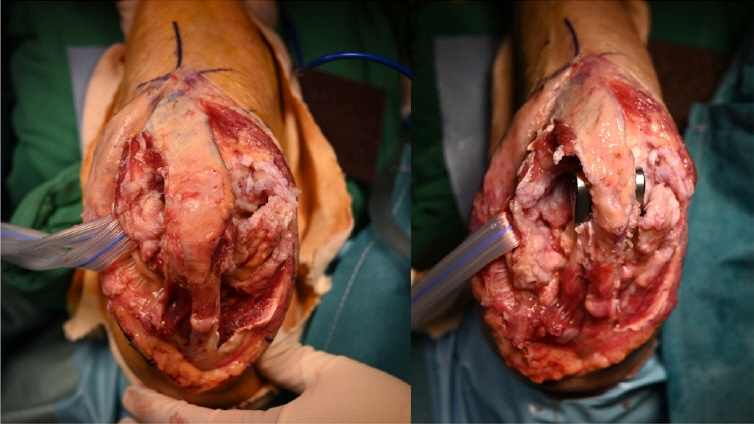
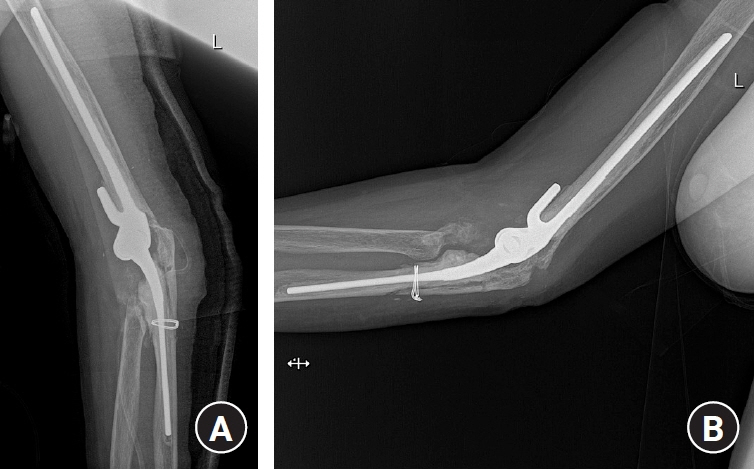
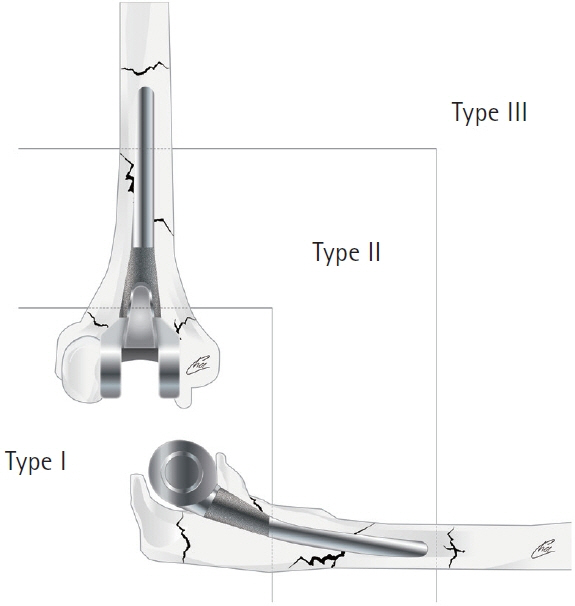
- The indications for total elbow arthroplasty have been expanded beyond severe arthritis to include acute comminuted fractures. Advances in implant manufacturing and surgical techniques in recent decades have led to increasingly better results. Semiconstrained implants are most commonly used, followed by conversion-type and unlinked implants. However, the results are still worse than those of arthroplasty in the knee or hip joint, and various complications such as aseptic loosening, infection, bushing wear, and periprosthetic fractures still occur. As aging adults are increasingly indicated for surgery, we inevitably face complications that are not easy to control. In this review, we discuss intraoperative and late complications, their prevention, and treatment options.
Keyword
Figure
Reference
-
References
1. Pritchard RW. Anatomic surface elbow arthroplasty: a preliminary report. Clin Orthop Relat Res. 1983; (179):223–30.
Article2. Kudo H, Iwano K. Total elbow arthroplasty with a non-constrained surface-replacement prosthesis in patients who have rheumatoid arthritis: a long-term follow-up study. J Bone Joint Surg Am. 1990; 72:355–62.
Article3. Madsen F, Gudmundson GH, Søjbjerg JO, Sneppen O. The Pritchard Mark II elbow prosthesis in rheumatoid arthritis. Acta Orthop Scand. 1989; 60:249–53.
Article4. O’Driscoll SW, An KN, Korinek S, Morrey BF. Kinematics of semi-constrained total elbow arthroplasty. J Bone Joint Surg Br. 1992; 74:297–9.5. Ring D, Koris M, Jupiter JB. Instability after total elbow arthroplasty. Orthop Clin North Am. 2001; 32:671–7.
Article6. O’Driscoll SW, King GJ. Treatment of instability after total elbow arthroplasty. Orthop Clin North Am. 2001; 32:679–95.
Article7. Kholinne E, Altamimi LA, Aldayel A, et al. Primary linked total elbow arthroplasty for acute distal humerus fracture management: a systematic review of clinical outcome. Clin Orthop Surg. 2020; 12:503–13.
Article8. Mäkelä KT, Matilainen M, Pulkkinen P, et al. Countrywise results of total hip replacement: an analysis of 438,733 hips based on the Nordic Arthroplasty Register Association database. Acta Orthop. 2014; 85:107–16.9. Little CP, Graham AJ, Carr AJ. Total elbow arthroplasty: a systematic review of the literature in the English language until the end of 2003. J Bone Joint Surg Br. 2005; 87:437–44.10. Labek G, Thaler M, Janda W, Agreiter M, Stöckl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011; 93:293–7.11. Perretta D, van Leeuwen WF, Dyer G, Ring D, Chen N. Risk factors for reoperation after total elbow arthroplasty. J Shoulder Elbow Surg. 2017; 26:824–9.
Article12. Wang JH, Ma HH, Chou TA, et al. Outcomes following total elbow arthroplasty for rheumatoid arthritis versus post-traumatic conditions: a systematic review and meta-analysis. Bone Joint J. 2019; 101-B:1489–97.13. van Riet RP, Morrey BF, O’Driscoll SW. The Pritchard ERS total elbow prosthesis: lessons to be learned from failure. J Shoulder Elbow Surg. 2009; 18:791–5.
Article14. Hastings H 2nd, Theng CS. Total elbow replacement for distal humerus fractures and traumatic deformity: results and complications of semiconstrained implants and design rationale for the Discovery Elbow System. Am J Orthop (Belle Mead NJ). 2003; 32(9 Suppl):20–8.15. Morrey BF. Elbow arthroplasty: historical perspective and emerging concepts. In : Morrey BF, Sanchez-Sotelo J, Morrey ME, editors. Morrey’s the elbow and its disorders. 15th ed. Philadelphia: Elsevier;2018. p. 807–17.16. Morrey BF, Chao EY. Passive motion of the elbow joint. J Bone Joint Surg Am. 1976; 58:501–8.
Article17. Aldridge JM 3rd, Lightdale NR, Mallon WJ, Coonrad RW. Total elbow arthroplasty with the Coonrad/Coonrad-Morrey prosthesis: a 10- to 31-year survival analysis. J Bone Joint Surg Br. 2006; 88:509–14.18. O’Driscoll SW, Morrey BF. Periprosthetic fractures about the elbow. Orthop Clin North Am. 1999; 30:319–25.
Article19. Sanchez-Sotelo J, O’Driscoll S, Morrey BF. Periprosthetic humeral fractures after total elbow arthroplasty: treatment with implant revision and strut allograft augmentation. J Bone Joint Surg Am. 2002; 84:1642–50.20. Ramirez MA, Cheung EV, Murthi AM. Revision total elbow arthroplasty. J Am Acad Orthop Surg. 2017; 25:e166–74.
Article21. Ito H, Matsumoto T, Yoshitomi H, Kakinoki R, Nakamura T. The outcome of peri-operative humeral condylar fractures after total elbow replacement in patients with rheumatoid arthritis. J Bone Joint Surg Br. 2007; 89:62–5.
Article22. Gschwend N, Simmen BR, Matejovsky Z. Late complications in elbow arthroplasty. J Shoulder Elbow Surg. 1996; 5(2 Pt 1):86–96.
Article23. Voloshin I, Schippert DW, Kakar S, Kaye EK, Morrey BF. Complications of total elbow replacement: a systematic review. J Shoulder Elbow Surg. 2011; 20:158–68.
Article24. Welsink CL, Lambers KT, van Deurzen DF, Eygendaal D, van den Bekerom MP. Total elbow arthroplasty: a systematic review. JBJS Rev. 2017; 5:e4.25. Parker P, Furness ND, Evans JP, Batten T, White WJ, Smith CD. A systematic review of the complications of contemporary total elbow arthroplasty. Shoulder Elbow. 2021; 13:544–51.
Article26. Brinkman JM, de Vos MJ, Eygendaal D. Failure mechanisms in uncemented Kudo type 5 elbow prosthesis in patients with rheumatoid arthritis: 7 of 49 ulnar components revised because of loosening after 2-10 years. Acta Orthop. 2007; 78:263–70.
Article27. Chou TA, Ma HH, Wang JH, et al. Total elbow arthroplasty in patients with rheumatoid arthritis. Bone Joint J. 2020; 102-B:967–80.
Article28. Prkic A, Welsink C, The B, van den Bekerom MP, Eygendaal D. Why does total elbow arthroplasty fail today?: a systematic review of recent literature. Arch Orthop Trauma Surg. 2017; 137:761–9.
Article29. Skyttä ET, Eskelinen A, Paavolainen P, Ikävalko M, Remes V. Total elbow arthroplasty in rheumatoid arthritis: a population-based study from the Finnish Arthroplasty Register. Acta Orthop. 2009; 80:472–7.30. Ibrahim EF, Rashid A, Thomas M. Linked semiconstrained and unlinked total elbow replacement in juvenile idiopathic arthritis: a case comparison series with mean 11.7-year follow-up. J Shoulder Elbow Surg. 2017; 26:305–13.
Article31. Wouthuyzen-Bakker M, Boerboom AL. Black pus from a worn-out elbow arthroplasty. J Bone Jt Infect. 2022; 7:33–4.
Article32. Lee H, Vaichinger AM, O’Driscoll SW. Component fracture after total elbow arthroplasty. J Shoulder Elbow Surg. 2019; 28:1449–56.
Article33. Goldberg SH, Urban RM, Jacobs JJ, King GJ, O’Driscoll SW, Cohen MS. Modes of wear after semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 2008; 90:609–19.
Article34. Kim JM, Mudgal CS, Konopka JF, Jupiter JB. Complications of total elbow arthroplasty. J Am Acad Orthop Surg. 2011; 19:328–39.
Article35. Lee SM, Park JC, Song SW, et al. Periprosthetic fractures after total elbow replacement. J Korean Soc Surg Hand. 2010; 15:107–11.36. Mavrogenis AF, Angelini A, Guerra E, Rotini R. Humeral fracture between a total elbow and total shoulder arthroplasty. Orthopedics. 2011; 34:01477447–20110228-21.
Article37. Rhee YG, Cho NS, Parke CS. Impaction grafting in revision total elbow arthroplasty due to aseptic loosening and bone loss. J Bone Joint Surg Am. 2013; 95:e741–7.
Article38. Dean GS, Holliger EH 4th, Urbaniak JR. Elbow allograft for reconstruction of the elbow with massive bone loss. Long term results. Clin Orthop Relat Res. 1997; (341):12–22.39. Figgie HE 3rd, Inglis AE, Ranawat CS, Rosenberg GM. Results of total elbow arthroplasty as a salvage procedure for failed elbow reconstructive operations. Clin Orthop Relat Res. 1987; (219):185–93.40. Kamineni S, Morrey BF. Proximal ulnar reconstruction with strut allograft in revision total elbow arthroplasty. J Bone Joint Surg Am. 2004; 86:1223–9.
Article41. Mansat P, Adams RA, Morrey BF. Allograft-prosthesis composite for revision of catastrophic failure of total elbow arthroplasty. J Bone Joint Surg Am. 2004; 86:724–35.
Article42. Laumonerie P, Granjou J, Tibbo ME, Massin V, Bonnevialle N, Mansat P. Midterm outcomes allograft prosthetic composite reconstruction for massive bone loss at the elbow. Orthop Traumatol Surg Res. 2023; 109:103517.
Article43. Athwal GS, Morrey BF. Revision total elbow arthroplasty for prosthetic fractures. J Bone Joint Surg Am. 2006; 88:2017–26.
Article44. Toulemonde J, Ancelin D, Azoulay V, Bonnevialle N, Rongières M, Mansat P. Complications and revisions after semi-constrained total elbow arthroplasty: a mono-centre analysis of one hundred cases. Int Orthop. 2016; 40:73–80.
Article45. Ljung P, Bornmyr S, Svensson H. Wound healing after total elbow replacement in rheumatoid arthritis: wound complications in 50 cases and laser-Doppler imaging of skin microcirculation. Acta Orthop Scand. 1995; 66:59–63.
Article46. Escalante A, Beardmore TD. Risk factors for early wound complications after orthopedic surgery for rheumatoid arthritis. J Rheumatol. 1995; 22:1844–51.47. Jeon IH, Morrey BF, Anakwenze OA, Tran NV. Incidence and implications of early postoperative wound complications after total elbow arthroplasty. J Shoulder Elbow Surg. 2011; 20:857–65.
Article48. Spangehl M. Preoperative prophylactic antibiotics in total hip and knee arthroplasty: what, when, and how. J Arthroplasty. 2022; 37:1432–4.49. Goyal N, Luchetti TJ, Wysocki RW, Cohen MS. Management of periprosthetic joint infection in total elbow arthroplasty. J Hand Surg Am. 2020; 45:957–70.
Article50. Yamaguchi K, Adams RA, Morrey BF. Infection after total elbow arthroplasty. J Bone Joint Surg Am. 1998; 80:481–91.
Article51. Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008; 23:984–91.
Article52. Block JE, Stubbs HA. Reducing the risk of deep wound infection in primary joint arthroplasty with antibiotic bone cement. Orthopedics. 2005; 28:1334–45.
Article53. Leong JW, Cook MJ, O’Neill TW, Board TN. Is the use of antibiotic-loaded bone cement associated with a lower risk of revision after primary total hip arthroplasty? Bone Joint J. 2020; 102-B:997–1002.54. Mercurio M, Castioni D, Cosentino O, et al. Revision surgery for periprosthetic elbow infection: eradication rate, complications, and functional outcomes: a systematic review. Arch Orthop Trauma Surg. 2023; 143:1117–31.
Article55. Spormann C, Achermann Y, Simmen BR, et al. Treatment strategies for periprosthetic infections after primary elbow arthroplasty. J Shoulder Elbow Surg. 2012; 21:992–1000.
Article56. Somerson JS, Morrey ME, Sanchez-Sotelo J, Morrey BF. Diagnosis and management of periprosthetic elbow infection. J Bone Joint Surg Am. 2015; 97:1962–71.
Article57. Peach CA, Nicoletti S, Lawrence TM, Stanley D. Two-stage revision for the treatment of the infected total elbow arthroplasty. Bone Joint J. 2013; 95-B:1681–6.
Article58. Wolfe SW, Figgie MP, Inglis AE, Bohn WW, Ranawat CS. Management of infection about total elbow prostheses. J Bone Joint Surg Am. 1990; 72:198–212.
Article59. Rhee YG, Cho NS, Park JG, Song JH. Resection arthroplasty for periprosthetic infection after total elbow arthroplasty. J Shoulder Elbow Surg. 2016; 25:105–11.
Article60. Dachs RP, Vrettos BC, Chivers DA, Du Plessis JP, Roche SJ. Outcomes after ulnar nerve in situ release during total elbow arthroplasty. J Hand Surg Am. 2015; 40:1832–7.
Article61. Gill DR, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis: a ten to fifteen-year follow-up study. J Bone Joint Surg Am. 1998; 80:1327–35.
Article62. Kelly EW, Coghlan J, Bell S. Five- to thirteen-year follow-up of the GSB III total elbow arthroplasty. J Shoulder Elbow Surg. 2004; 13:434–40.
Article63. Pierce TD, Herndon JH. The triceps preserving approach to total elbow arthroplasty. Clin Orthop Relat Res. 1998; (354):144–52.
Article64. Hildebrand KA, Patterson SD, Regan WD, MacDermid JC, King GJ. Functional outcome of semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 2000; 82:1379–86.
Article65. Studer A, Athwal GS, MacDermid JC, Faber KJ, King GJ. The lateral para-olecranon approach for total elbow arthroplasty. J Hand Surg Am. 2013; 38:2219–26.
Article66. Dachs RP, Fleming MA, Chivers DA, et al. Total elbow arthroplasty: outcomes after triceps-detaching and triceps-sparing approaches. J Shoulder Elbow Surg. 2015; 24:339–47.
Article67. Celli A, Arash A, Adams RA, Morrey BF. Triceps insufficiency following total elbow arthroplasty. J Bone Joint Surg Am. 2005; 87:1957–64.
Article68. Liu EY, Hildebrand A, Horner NS, Athwal GS, Khan M, Alolabi B. Heterotopic ossification after total elbow arthroplasty: a systematic review. J Shoulder Elbow Surg. 2019; 28:587–95.
Article69. Peden JP, Morrey BF. Total elbow replacement for the management of the ankylosed or fused elbow. J Bone Joint Surg Br. 2008; 90:1198–204.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Total Elbow Arthroplasty for the Fracture of Elbow Arthrodesis Site: A Case Report
- Outcomes and Complications of Total Elbow Arthroplasty
- Linked Semi-constrained or Unlinked TER: What We Should Know Before We Use?
- Unlinked and Convertible Total Elbow Arthroplasty
- Total Elbow Arthroplasty: Clinical Outcomes, Complications, and Revision Surgery