Clin Orthop Surg.
2019 Dec;11(4):369-379. 10.4055/cios.2019.11.4.369.
Total Elbow Arthroplasty: Clinical Outcomes, Complications, and Revision Surgery
- Affiliations
-
- 1Department of Orthopedics, Biomechanics Laboratory, Mayo Clinic, Rochester, MN, USA.
- 2Department of Orthopedic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jeonchoi@gmail.com
- KMID: 2462529
- DOI: http://doi.org/10.4055/cios.2019.11.4.369
Abstract
- Total elbow arthroplasty is a common surgical procedure used in the management of advanced rheumatoid arthritis, posttraumatic arthritis, osteoarthritis, and unfixable fracture in elderly patients. Total elbow prostheses have evolved over the years and now include the linked, unlinked, and convertible types. However, long-term complications, including infection, aseptic loosening, instability, and periprosthetic fracture, remain a challenge. Here, we introduce each type of implant and evaluate clinical outcomes and complications by reviewing the previous literature.
Keyword
MeSH Terms
Figure
Reference
-
1. Dee R. Total replacement arthroplasty of the elbow for rheumatoid arthritis. J Bone Joint Surg Br. 1972; 54(1):88–95. PMID: 5011749.
Article2. Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986; 68(5):669–674. PMID: 3722222.
Article3. Giannicola G, Sacchetti FM, Antonietti G, Piccioli A, Postacchini R, Cinotti G. Radial head, radiocapitellar and total elbow arthroplasties: a review of recent literature. Injury. 2014; 45(2):428–436. PMID: 24112701.
Article4. Hackl M, Muller LP, Leschinger T, Wegmann K. Total elbow arthroplasty in traumatic and post-traumatic bone defects. Orthopade. 2017; 46(12):990–1000. PMID: 29098354.5. Lami D, Chivot M, Caubere A, Galland A, Argenson JN. First-line management of distal humerus fracture by total elbow arthroplasty in geriatric traumatology: results in a 21-patient series at a minimum 2 years' follow-up. Orthop Traumatol Surg Res. 2017; 103(6):891–897. PMID: 28733108.
Article6. Mansat P, Bonnevialle N, Rongieres M, Bonnevialle P. Bone, Joint Trauma Study Group (GETRAUM). The role of total elbow arthroplasty in traumatology. Orthop Traumatol Surg Res. 2014; 100(6 Suppl):S293–S298. PMID: 25164351.
Article7. Pogliacomi F, Schiavi P, Defilippo M, et al. Total elbow arthroplasty following complex fractures of the distal humerus: results in patients over 65 years of age. Acta Biomed. 2016; 87(2):148–155. PMID: 27648996.8. Pooley J, Salvador Carreno J. Total elbow joint replacement for fractures in the elderly: functional and radiological outcomes. Injury. 2015; 46 Suppl 5:S37–S42. PMID: 26362422.9. Rajaee SS, Lin CA, Moon CN. Primary total elbow arthroplasty for distal humeral fractures in elderly patients: a nationwide analysis. J Shoulder Elbow Surg. 2016; 25(11):1854–1860. PMID: 27528540.
Article10. Schoch BS, Werthel JD, Sanchez-Sotelo J, Morrey BF, Morrey M. Total elbow arthroplasty for primary osteoarthritis. J Shoulder Elbow Surg. 2017; 26(8):1355–1359. PMID: 28734537.
Article11. Brinkman JM, de Vos MJ, Eygendaal D. Failure mechanisms in uncemented Kudo type 5 elbow prosthesis in patients with rheumatoid arthritis: 7 of 49 ulnar components revised because of loosening after 2-10 years. Acta Orthop. 2007; 78(2):263–270. PMID: 17464617.
Article12. Kim HJ, Kim JY, Kee YM, Rhee YG. Total elbow arthroplasty under unfavourable soft tissue conditions. Int Orthop. 2018; 42(2):367–374. PMID: 29209741.
Article13. Kim JM, Mudgal CS, Konopka JF, Jupiter JB. Complications of total elbow arthroplasty. J Am Acad Orthop Surg. 2011; 19(6):328–339. PMID: 21628644.
Article14. Klug A, Gramlich Y, Buckup J, Schweigkofler U, Hoffmann R, Schmidt-Horlohe K. Trends in total elbow arthroplasty: a nationwide analysis in Germany from 2005 to 2014. Int Orthop. 2018; 42(4):883–889. PMID: 29423639.
Article15. Park SE, Kim JY, Cho SW, Rhee SK, Kwon SY. Complications and revision rate compared by type of total elbow arthroplasty. J Shoulder Elbow Surg. 2013; 22(8):1121–1127. PMID: 23664747.
Article16. Toulemonde J, Ancelin D, Azoulay V, Bonnevialle N, Rongieres M, Mansat P. Complications and revisions after semi-constrained total elbow arthroplasty: a mono-centre analysis of one hundred cases. Int Orthop. 2016; 40(1):73–80. PMID: 26435264.
Article17. Welsink CL, Lambers KT, van Deurzen DF, Eygendaal D, van den Bekerom MP. Total elbow arthroplasty: a systematic review. JBJS Rev. 2017; 5(7):e4.18. Kudo H, Iwano K. Total elbow arthroplasty with a non-constrained surface-replacement prosthesis in patients who have rheumatoid arthritis: a long-term follow-up study. J Bone Joint Surg Am. 1990; 72(3):355–362. PMID: 2312530.
Article19. Iwamoto T, Ikegami H, Suzuki T, et al. The history and future of unlinked total elbow arthroplasty. Keio J Med. 2018; 67(2):19–25. PMID: 28835585.
Article20. Kaufmann RA, D'Auria JL, Schneppendahl J. Total elbow arthroplasty: elbow biomechanics and failure. J Hand Surg Am. 2019; 44(8):687–692. PMID: 30770149.
Article21. Kodama A, Mizuseki T, Adachi N. Macroscopic investigation of failed Kudo type 5 total elbow arthroplasty. J Shoulder Elbow Surg. 2018; 27(8):1380–1385. PMID: 30016691.
Article22. Kodama A, Mizuseki T, Adachi N. Kudo type-5 total elbow arthroplasty for patients with rheumatoid arthritis: a minimum ten-year follow-up study. Bone Joint J. 2017; 99(6):818–823. PMID: 28566403.23. Ramirez MA, Cheung EV, Murthi AM. Revision total elbow arthroplasty. J Am Acad Orthop Surg. 2017; 25(8):e166–e174. PMID: 28737619.
Article24. Figgie MP, Wright TM, Drinkwater D. Bioengineering Working Group. What design and material factors impact the wear and corrosion performance in total elbow arthroplasties? Clin Orthop Relat Res. 2014; 472(12):3770–3776. PMID: 25024029.
Article25. Aldridge JM 3rd, Lightdale NR, Mallon WJ, Coonrad RW. Total elbow arthroplasty with the Coonrad/Coonrad-Morrey prosthesis: a 10- to 31-year survival analysis. J Bone Joint Surg Br. 2006; 88(4):509–514. PMID: 16567787.26. King EA, Favre P, Eldemerdash A, Bischoff JE, Palmer M, Lawton JN. Physiological loading of the Coonrad/Morrey, Nexel, and Discovery elbow systems: evaluation by finite element analysis. J Hand Surg Am. 2019; 44(1):61.e1–61.e9. PMID: 29908927.
Article27. Jeon IH, Morrey BF, Sanchez-Sotelo J. Ulnar component surface finish influenced the outcome of primary Coonrad-Morrey total elbow arthroplasty. J Shoulder Elbow Surg. 2012; 21(9):1229–1235. PMID: 22104128.
Article28. Shi LL, Zurakowski D, Jones DG, Koris MJ, Thornhill TS. Semiconstrained primary and revision total elbow arthroplasty with use of the Coonrad-Morrey prosthesis. J Bone Joint Surg Am. 2007; 89(7):1467–1475. PMID: 17606785.
Article29. Pham TT, Delclaux S, Huguet S, Wargny M, Bonnevialle N, Mansat P. Coonrad-Morrey total elbow arthroplasty for patients with rheumatoid arthritis: 54 prostheses reviewed at 7 years' average follow-up (maximum, 16 years). J Shoulder Elbow Surg. 2018; 27(3):398–403. PMID: 29306664.
Article30. Kiran M, Jariwala A, Wigderowitz C. Medium term outcomes of primary and revision Coonrad-Morrey total elbow replacement. Indian J Orthop. 2015; 49(2):233–238. PMID: 26015615.
Article31. Barthel PY, Mansat P, Sirveaux F, Dap F, Mole D, Dautel G. Is total elbow arthroplasty indicated in the treatment of traumatic sequelae? 19 Cases of Coonrad-Morrey(®) reviewed at a mean follow-up of 5.2 years. Orthop Traumatol Surg Res. 2014; 100(1):113–118. PMID: 24370486.32. Mansat P, Bonnevialle N, Rongieres M, Mansat M, Bonnevialle P. Experience with the Coonrad-Morrey total elbow arthroplasty: 78 consecutive total elbow arthroplasties reviewed with an average 5 years of follow-up. J Shoulder Elbow Surg. 2013; 22(11):1461–1468. PMID: 24138820.
Article33. Mansat P, Bonnevialle N, Rongieres M, Mansat M, Bonnevialle P. French Society for Shoulder and Elbow SOFEC. Results with a minimum of 10 years follow-up of the Coonrad/Morrey total elbow arthroplasty. Orthop Traumatol Surg Res. 2013; 99(6 Suppl):S337–S343. PMID: 23932914.
Article34. Schneeberger AG, Meyer DC, Yian EH. Coonrad-Morrey total elbow replacement for primary and revision surgery: a 2- to 7.5-year follow-up study. J Shoulder Elbow Surg. 2007; 16(3 Suppl):S47–S54. PMID: 16963289.
Article35. Gill DR, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis: a ten to fifteen-year follow-up study. J Bone Joint Surg Am. 1998; 80(9):1327–1335. PMID: 9759818.
Article36. Morrey BF, Bryan RS, Dobyns JH, Linscheid RL. Total elbow arthroplasty: a five-year experience at the Mayo Clinic. J Bone Joint Surg Am. 1981; 63(7):1050–1063. PMID: 7276042.
Article37. Sundfeldt M, Carlsson LV, Johansson CB, Thomsen P, Gretzer C. Aseptic loosening, not only a question of wear: a review of different theories. Acta Orthop. 2006; 77(2):177–197. PMID: 16752278.
Article38. Mukka S, Berg G, Hassany HR, Koye AK, Sjoden G, Sayed-Noor AS. Semiconstrained total elbow arthroplasty for rheumatoid arthritis patients: clinical and radiological results of 1-8 years follow-up. Arch Orthop Trauma Surg. 2015; 135(5):595–600. PMID: 25733382.39. Alizadehkhaiyat O, Al Mandhari A, Sinopidis C, Wood A, Frostick S. Total elbow arthroplasty: a prospective clinical outcome study of Discovery Elbow System with a 4-year mean follow-up. J Shoulder Elbow Surg. 2015; 24(1):52–59. PMID: 25441571.
Article40. Hastings H 2nd. Minimally constrained elbow implant arthroplasty: the discovery elbow system. Tech Hand Up Extrem Surg. 2004; 8(1):34–50. PMID: 16518239.
Article41. de Vos MJ, Wagener ML, Hannink G, van der Pluijm M, Verdonschot N, Eygendaal D. Short-term clinical results of revision elbow arthroplasty using the Latitude total elbow arthroplasty. Bone Joint J. 2016; 98(8):1086–1092. PMID: 27482022.
Article42. Wagener ML, de Vos MJ, Hannink G, van der Pluijm M, Verdonschot N, Eygendaal D. Mid-term clinical results of a modern convertible total elbow arthroplasty. Bone Joint J. 2015; 97(5):681–688. PMID: 25922464.
Article43. Prkic A, Welsink C, The B, van den, Eygendaal D. Why does total elbow arthroplasty fail today? A systematic review of recent literature. Arch Orthop Trauma Surg. 2017; 137(6):761–769. PMID: 28391430.
Article44. Krukhaug Y, Hallan G, Dybvik E, Lie SA, Furnes ON. A survivorship study of 838 total elbow replacements: a report from the Norwegian Arthroplasty Register 1994-2016. J Shoulder Elbow Surg. 2018; 27(2):260–269. PMID: 29332662.
Article45. Hildebrand KA, Patterson SD, Regan WD, MacDermid JC, King GJ. Functional outcome of semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 2000; 82(10):1379–1386. PMID: 11057465.
Article46. Rangarajan R, Papandrea RF, Cil A. Distal humeral hemiarthroplasty versus total elbow arthroplasty for acute distal humeral fractures. Orthopedics. 2017; 40(1):13–23. PMID: 28375524.
Article47. Lovy AJ, Keswani A, Koehler SM, Kim J, Hausman M. Short-term complications of distal humerus fractures in elderly patients: open reduction internal fixation versus total elbow arthroplasty. Geriatr Orthop Surg Rehabil. 2016; 7(1):39–44. PMID: 26929856.48. Lapner M, King GJ. Elbow arthroplasty for distal humeral fractures. Instr Course Lect. 2014; 63:15–26. PMID: 24720290.49. Zhang D, Chen N. Total elbow arthroplasty. J Hand Surg Am. 2019; 44(6):487–495. PMID: 30635202.
Article50. Schoch B, Wong J, Abboud J, Lazarus M, Getz C, Ramsey M. Results of total elbow arthroplasty in patients less than 50 years old. J Hand Surg Am. 2017; 42(10):797–802. PMID: 28823536.
Article51. McKee MD, Veillette CJ, Hall JA, et al. A multicenter, prospective, randomized, controlled trial of open reduction: internal fixation versus total elbow arthroplasty for displaced intra-articular distal humeral fractures in elderly patients. J Shoulder Elbow Surg. 2009; 18(1):3–12. PMID: 18823799.52. Barco R, Streubel PN, Morrey BF, Sanchez-Sotelo J. Total elbow arthroplasty for distal humeral fractures: a ten-year-minimum follow-up study. J Bone Joint Surg Am. 2017; 99(18):1524–1531. PMID: 28926381.53. Jenkins PJ, Watts AC, Norwood T, Duckworth AD, Rymaszewski LA, McEachan JE. Total elbow replacement: outcome of 1,146 arthroplasties from the Scottish Arthroplasty Project. Acta Orthop. 2013; 84(2):119–123. PMID: 23485072.
Article54. Fevang BT, Lie SA, Havelin LI, Skredderstuen A, Furnes O. Results after 562 total elbow replacements: a report from the Norwegian Arthroplasty Register. J Shoulder Elbow Surg. 2009; 18(3):449–456. PMID: 19393935.
Article55. Amirfeyz R, Blewitt N. Mid-term outcome of GSB-III total elbow arthroplasty in patients with rheumatoid arthritis and patients with post-traumatic arthritis. Arch Orthop Trauma Surg. 2009; 129(11):1505–1510. PMID: 19373479.
Article56. Giannicola G, Scacchi M, Polimanti D, Cinotti G. Discovery elbow system: 2- to 5-year results in distal humerus fractures and posttraumatic conditions: a prospective study on 24 patients. J Hand Surg Am. 2014; 39(9):1746–1756. PMID: 25063393.
Article57. Lenich A, Imhoff AB, Siebenlist S. Post-traumatic osteoarthritis of the elbow joint: endoprosthetic options in young patients. Orthopade. 2016; 45(10):844–852. PMID: 27647165.58. Celli A, Morrey BF. Total elbow arthroplasty in patients forty years of age or less. J Bone Joint Surg Am. 2009; 91(6):1414–1418. PMID: 19487519.
Article59. Park JG, Cho NS, Song JH, Lee DS, Rhee YG. Clinical outcomes of semiconstrained total elbow arthroplasty in patients who were forty years of age or younger. J Bone Joint Surg Am. 2015; 97(21):1781–1791. PMID: 26537166.
Article60. Kwak JM, Kholinne E, Sun Y, Lim S, Koh KH, Jeon IH. Clinical outcome of osteocapsular arthroplasty for primary osteoarthritis of the elbow: comparison of arthroscopic and open procedure. Arthroscopy. 2019; 35(4):1083–1089. PMID: 30871900.
Article61. Kwak JM, Kholinne E, Sun Y, Kim MS, Koh KH, Jeon IH. Clinical results of revision total elbow arthroplasty: comparison of infected and non-infected total elbow arthroplasty. Int Orthop. 2019; 43(6):1421–1427. PMID: 30617613.62. Farnsworth CW, Schott EM, Benvie AM, et al. Obesity/type 2 diabetes increases inflammation, periosteal reactive bone formation, and osteolysis during Staphylococcus aureus implant-associated bone infection. J Orthop Res. 2018; 36(6):1614–1623. PMID: 29227579.63. Perretta D, van Leeuwen WF, Dyer G, Ring D, Chen N. Risk factors for reoperation after total elbow arthroplasty. J Shoulder Elbow Surg. 2017; 26(5):824–829. PMID: 28159475.
Article64. Griffin JW, Werner BC, Gwathmey FW, Chhabra AB. Obesity is associated with increased postoperative complications after total elbow arthroplasty. J Shoulder Elbow Surg. 2015; 24(10):1594–1601. PMID: 26385389.
Article65. Geurts EJ, Viveen J, van Riet RP, Kodde IF, Eygendaal D. Outcomes after revision total elbow arthroplasty: a systematic review. J Shoulder Elbow Surg. 2019; 28(2):381–386. PMID: 30658776.
Article66. Parvizi J, Shohat N, Gehrke T. Prevention of periprosthetic joint infection: new guidelines. Bone Joint J. 2017; 99(4 Supple B):3–10.67. Ting NT, Della Valle CJ. Diagnosis of periprosthetic joint infection-an algorithm-based approach. J Arthroplasty. 2017; 32(7):2047–2050. PMID: 28343826.
Article68. Somerson JS, Morrey ME, Sanchez-Sotelo J, Morrey BF. Diagnosis and management of periprosthetic elbow infection. J Bone Joint Surg Am. 2015; 97(23):1962–1971. PMID: 26631998.
Article69. Drago L, De Vecchi E, Bortolin M, Zagra L, Romano CL, Cappelletti L. Epidemiology and antibiotic resistance of late prosthetic knee and hip infections. J Arthroplasty. 2017; 32(8):2496–2500. PMID: 28390886.
Article70. Henderson RA, Austin MS. Management of periprosthetic joint infection: the more we learn, the less we know. J Arthroplasty. 2017; 32(7):2056–2059. PMID: 28318868.
Article71. Pruzansky JS, Bronson MJ, Grelsamer RP, Strauss E, Moucha CS. Prevalence of modifiable surgical site infection risk factors in hip and knee joint arthroplasty patients at an urban academic hospital. J Arthroplasty. 2014; 29(2):272–276. PMID: 23890832.
Article72. Streubel PN, Simone JP, Morrey BF, Sanchez-Sotelo J, Morrey ME. Infection in total elbow arthroplasty with stable components: outcomes of a staged surgical protocol with retention of the components. Bone Joint J. 2016; 98(7):976–983. PMID: 27365477.73. Kok TW, Agrawal N, Sathappan SS, Chen WK. Risk factors for early implant-related surgical site infection. J Orthop Surg (Hong Kong). 2016; 24(1):72–76. PMID: 27122517.
Article74. Spormann C, Achermann Y, Simmen BR, et al. Treatment strategies for periprosthetic infections after primary elbow arthroplasty. J Shoulder Elbow Surg. 2012; 21(8):992–1000. PMID: 22221886.
Article75. Pope D, Scaife SL, Tzeng TH, Vasdev S, Saleh KJ. Impact of diabetes on early postoperative outcomes after total elbow arthroplasty. J Shoulder Elbow Surg. 2015; 24(3):348–352. PMID: 25499723.
Article76. Toor AS, Jiang JJ, Shi LL, Koh JL. Comparison of perioperative complications after total elbow arthroplasty in patients with and without diabetes. J Shoulder Elbow Surg. 2014; 23(11):1599–1606. PMID: 25213826.
Article77. Mraovic B, Suh D, Jacovides C, Parvizi J. Perioperative hyperglycemia and postoperative infection after lower limb arthroplasty. J Diabetes Sci Technol. 2011; 5(2):412–418. PMID: 21527113.
Article78. Yoon HK, Cho SH, Lee DY, et al. A review of the literature on culture-negative periprosthetic joint infection: epidemiology, diagnosis and treatment. Knee Surg Relat Res. 2017; 29(3):155–164. PMID: 28854760.
Article79. Peach CA, Nicoletti S, Lawrence TM, Stanley D. Two-stage revision for the treatment of the infected total elbow arthroplasty. Bone Joint J. 2013; 95(12):1681–1686. PMID: 24293600.
Article80. Rudge WB, Eseonu K, Brown M, et al. The management of infected elbow arthroplasty by two-stage revision. J Shoulder Elbow Surg. 2018; 27(5):879–886. PMID: 29503100.
Article81. Wagner ER, Ransom JE, Kremers HM, Morrey M, Sanchez-Sotelo J. Comparison of the hospital costs for two-stage reimplantation for deep infection, single-stage revision and primary total elbow arthroplasty. Shoulder Elbow. 2017; 9(4):279–284. PMID: 28932285.
Article82. Zmistowski B, Pourjafari A, Padegimas EM, et al. Treatment of periprosthetic joint infection of the elbow: 15-year experience at a single institution. J Shoulder Elbow Surg. 2018; 27(9):1636–1641. PMID: 30045830.
Article83. Osmon DR, Berbari EF, Berendt AR, et al. Diagnosis and management of prosthetic joint infection: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2013; 56(1):e1–e25. PMID: 23223583.84. Choi HR, Kwon YM, Freiberg AA, Nelson SB, Malchau H. Periprosthetic joint infection with negative culture results: clinical characteristics and treatment outcome. J Arthroplasty. 2013; 28(6):899–903. PMID: 23523496.
Article85. Parvizi J, Adeli B, Zmistowski B, Restrepo C, Greenwald AS. Management of periprosthetic joint infection: the current knowledge: AAOS exhibit selection. J Bone Joint Surg Am. 2012; 94(14):e104. PMID: 22810411.86. Morrey BF, Bryan RS. Infection after total elbow arthroplasty. J Bone Joint Surg Am. 1983; 65(3):330–338. PMID: 6826595.
Article87. Zhou H, Orvets ND, Merlin G, et al. Total elbow arthroplasty in the United States: evaluation of cost, patient demographics, and complication rates. Orthop Rev (Pavia). 2016; 8(1):6113. PMID: 27114806.
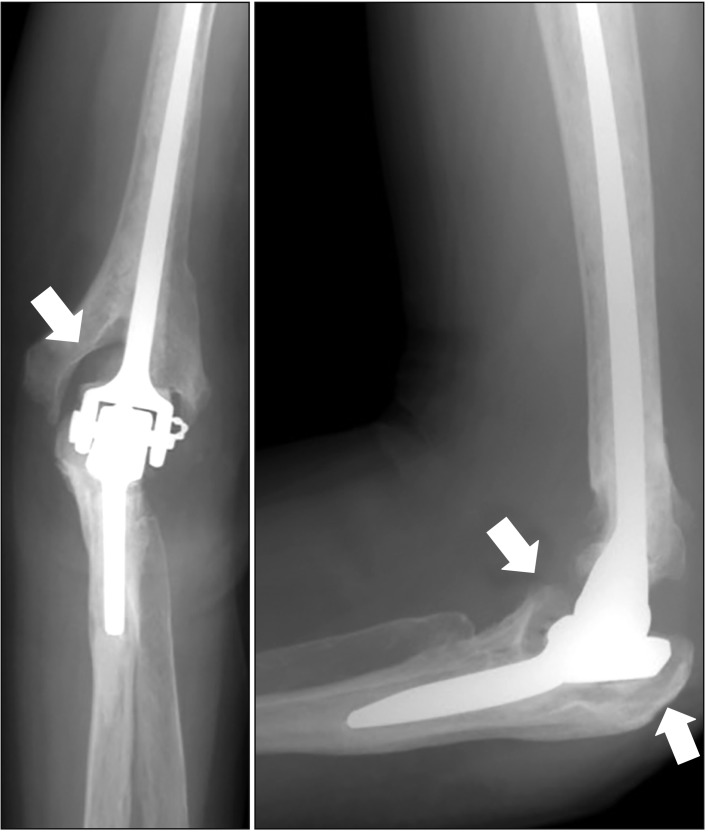
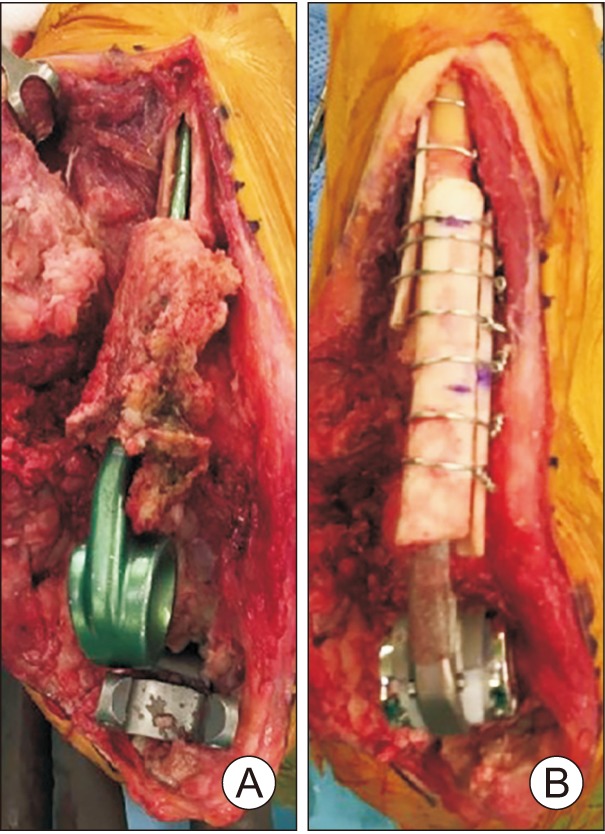
Article88. Rhee YG, Cho NS, Parke CS. Impaction grafting in revision total elbow arthroplasty due to aseptic loosening and bone loss. J Bone Joint Surg Am. 2013; 95(11):e741–e747. PMID: 23780544.
Article89. Goldberg SH, Urban RM, Jacobs JJ, King GJ, O'Driscoll SW, Cohen MS. Modes of wear after semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 2008; 90(3):609–619. PMID: 18310712.
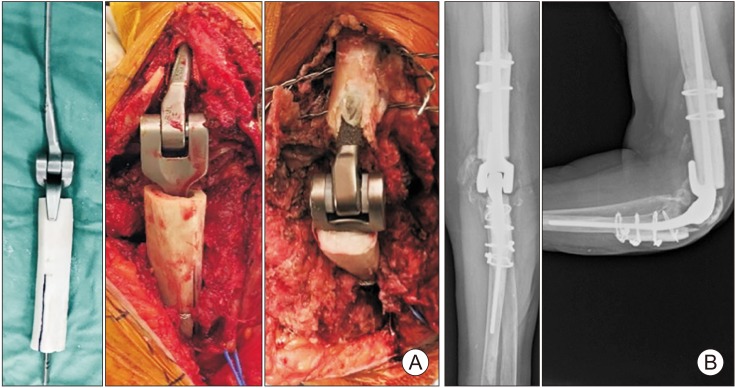
Article90. Morrey ME, Sanchez-Sotelo J, Abdel MP, Morrey BF. Allograft-prosthetic composite reconstruction for massive bone loss including catastrophic failure in total elbow arthroplasty. J Bone Joint Surg Am. 2013; 95(12):1117–1124. PMID: 23783209.
Article91. King GJ, Adams RA, Morrey BF. Total elbow arthroplasty: revision with use of a non-custom semiconstrained prosthesis. J Bone Joint Surg Am. 1997; 79(3):394–400. PMID: 9070529.92. Sanchez-Sotelo J, O’Driscoll S, Morrey BF. Periprosthetic humeral fractures after total elbow arthroplasty: treatment with implant revision and strut allograft augmentation. J Bone Joint Surg Am. 2002; 84(9):1642–1650. PMID: 12208923.93. Celli A, Arash A, Adams RA, Morrey BF. Triceps insufficiency following total elbow arthroplasty. J Bone Joint Surg Am. 2005; 87(9):1957–1964. PMID: 16140809.
Article94. Voloshin I, Schippert DW, Kakar S, Kaye EK, Morrey BF. Complications of total elbow replacement: a systematic review. J Shoulder Elbow Surg. 2011; 20(1):158–168. PMID: 21134667.
Article95. Dachs RP, Fleming MA, Chivers DA, et al. Total elbow arthroplasty: outcomes after triceps-detaching and triceps-sparing approaches. J Shoulder Elbow Surg. 2015; 24(3):339–347. PMID: 25591460.
Article96. Solarz MK, Patel MK, Struk AM, et al. A clinical comparison of triceps-sparing and triceps-detaching approaches for revision total elbow arthroplasty. J Hand Surg Am. 2019; 6. 18. [Epub]. DOI: 10.1016/j.jhsa.2019.05.002.
Article97. Lee H, Vaichinger AM, O'Driscoll SW. Component fracture after total elbow arthroplasty. J Shoulder Elbow Surg. 2019; 28(8):1449–1456. PMID: 31076278.
Article98. Dachs RP, Vrettos BC, Chivers DA, Du Plessis JP, Roche SJ. Outcomes after ulnar nerve in situ release during total elbow arthroplasty. J Hand Surg Am. 2015; 40(9):1832–1837. PMID: 26254945.
Article99. Morrey BF, Bryan RS. Revision total elbow arthroplasty. J Bone Joint Surg Am. 1987; 69(4):523–532. PMID: 3571311.
Article100. Cheung EV, O'Driscoll SW. Total elbow prosthesis loosening caused by ulnar component pistoning. J Bone Joint Surg Am. 2007; 89(6):1269–1274. PMID: 17545430.
Article101. Renfree KJ, Dell PC, Kozin SH, Wright TW. Total elbow arthroplasty with massive composite allografts. J Shoulder Elbow Surg. 2004; 13(3):313–321. PMID: 15111902.
Article102. O'Driscoll SW, King GJ. Treatment of instability after total elbow arthroplasty. Orthop Clin North Am. 2001; 32(4):679–695. PMID: 11689380.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unlinked and Convertible Total Elbow Arthroplasty
- Outcomes and Complications of Total Elbow Arthroplasty
- Reverse Total Shoulder Arthroplasty: Complications
- Total Elbow Arthroplasty for the Fracture of Elbow Arthrodesis Site: A Case Report
- Revision Total Elbow Replacement Arthroplasty with an Allograft-Prosthesis Composite: Case Series and Technical Points