Arch Hand Microsurg.
2020 Jun;25(2):101-107. 10.12790/ahm.20.0021.
Revision Total Elbow Replacement Arthroplasty with an Allograft-Prosthesis Composite: Case Series and Technical Points
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- KMID: 2502705
- DOI: http://doi.org/10.12790/ahm.20.0021
Abstract
- Purpose
The purpose of this study was to report the results of revision total elbow replacement arthroplasty (TERA) with an allograft-prosthesis composite (APC).
Methods
We retrospectively reviewed 6 patients with an average age of 75 years who had undergone revision TERA with an APC for periprosthetic fracture or loosening of the component. The mean follow-up period was 13 months. We assessed serial radiographs for bone union and evaluated the outcomes in terms of pain visual analogue scale (VAS), the Mayo Elbow Performance Score (MEPS), range of motion, and complications.
Results
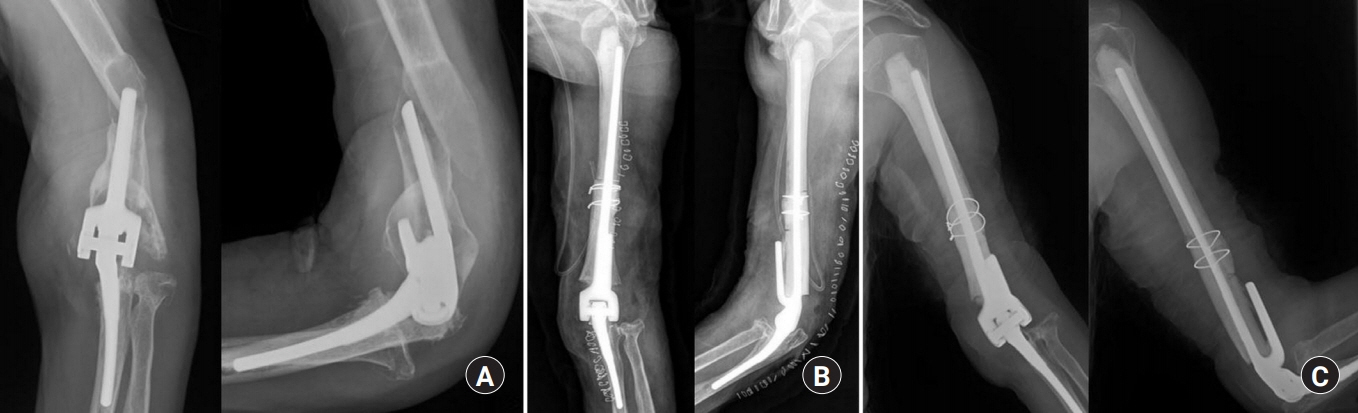
The APC was used for the humerus in 5 patients and for the ulna in 1 patient. The clinical bone union was achieved at average 9 months after surgery. The mean pain VAS score improved from 6.8 to 1.7, the mean elbow joint range of motion increased from 95° to 129° and the MEPS score improved from 40 to 79 at the last follow-up. There were no major complications such as infection, nonunion, malunion, limitation of motion or refracture. One patient experienced transient radial nerve palsy and another patient a prominent edge of the humeral allobone that needed a trimming surgery later.
Conclusion
Revision TERA with an APC provides good functional outcomes and can be recommended as one of the options for failed total elbow arthroplasty.
Keyword
Figure
Reference
-
1. Lee DH. Impaction allograft bone-grafting for revision total elbow arthroplasty: a case report. J Bone Joint Surg Am. 1999; 81:1008–12.
Article2. Renfree KJ, Dell PC, Kozin SH, Wright TW. Total elbow arthroplasty with massive composite allografts. J Shoulder Elbow Surg. 2004; 13:313–21.
Article3. Morrey ME, Sanchez-Sotelo J, Abdel MP, Morrey BF. Allograft-prosthetic composite reconstruction for massive bone loss including catastrophic failure in total elbow arthroplasty. J Bone Joint Surg Am. 2013; 95:1117–24.
Article4. Ramirez MA, Cheung EV, Murthi AM. Revision total elbow arthroplasty. J Am Acad Orthop Surg. 2017; 25:e166–74.
Article5. Geurts EJ, Viveen J, van Riet RP, Kodde IF, Eygendaal D. Outcomes after revision total elbow arthroplasty: a systematic review. J Shoulder Elbow Surg. 2019; 28:381–6.
Article6. Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010; 19:1115–20.
Article7. Amirfeyz R, Stanley D. Allograft-prosthesis composite reconstruction for the management of failed elbow replacement with massive structural bone loss: a medium-term follow-up. J Bone Joint Surg Br. 2011; 93:1382–8.8. Little CP, Graham AJ, Karatzas G, Woods DA, Carr AJ. Outcomes of total elbow arthroplasty for rheumatoid arthritis: comparative study of three implants. J Bone Joint Surg Am. 2005; 87:2439–48.
Article9. Bicknell RT, Hughes JS. A new technique for management of ulnar bone loss in revision total elbow arthroplasty using a tuberized tricortical iliac crest autograft: a case report. J Shoulder Elbow Surg. 2008; 17:e15–8.
Article10. Rhee YG, Cho NS, Parke CS. Impaction grafting in revision total elbow arthroplasty due to aseptic loosening and bone loss. J Bone Joint Surg Am. 2013; 95:e741–7.
Article11. Urbaniak JR, Black KE Jr. Cadaveric elbow allografts: a six-year experience. Clin Orthop Relat Res. 1985; (197):131–40.12. Urbaniak JR, Aitken M. Clinical use of bone allografts in the elbow. Orthop Clin North Am. 1987; 18:311–21.
Article13. Head WC, Wagner RA, Emerson RH Jr, Malinin TI. Revision total hip arthroplasty in the deficient femur with a proximal load-bearing prosthesis. Clin Orthop Relat Res. 1994; (298):119–26.
Article14. Morshed S. Current options for determining fracture union. Adv Med. 2014; 2014:708574.
Article15. Mansat P, Adams RA, Morrey BF. Allograft-prosthesis composite for revision of catastrophic failure of total elbow arthroplasty. J Bone Joint Surg Am. 2004; 86:724–35.
Article16. King JJ, Nystrom LM, Reimer NB, Gibbs CP Jr, Scarborough MT, Wright TW. Allograft-prosthetic composite reverse total shoulder arthroplasty for reconstruction of proximal humerus tumor resections. J Shoulder Elbow Surg. 2016; 25:45–54.
Article17. Gautam D, Malhotra R. Megaprosthesis versus allograft prosthesis composite for massive skeletal defects. J Clin Orthop Trauma. 2018; 9:63–80.
Article18. Zhao Y, Hu X, Li Z, et al. Use of polyvinylpyrrolidone-iodine solution for sterilisation and preservation improves mechanical properties and osteogenesis of allografts. Sci Rep. 2016; 6:38669.
Article19. Soyer J, Rouil M, Castel O. The effect of 10% povidone: iodine solution on contaminated bone allografts. J Hosp Infect. 2002; 50:183–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Revision Total Elbow Arthroplasty Using Strut Allograft: Two Cases Report
- Revision Arthroplasty for the Aseptic Loosening after Semiconstrained Total Elbow Replacement: Midterm Results
- Total Elbow Arthroplasty for the Fracture of Elbow Arthrodesis Site: A Case Report
- Total Elbow Replacement
- Reverse Total Shoulder Arthroplasty: Complications