Ann Hepatobiliary Pancreat Surg.
2023 Nov;27(4):394-402. 10.14701/ahbps.23-044.
Is aggressive intravenous fluid prescription the answer to reduce mortality in severe pancreatitis? The FLIP study: Fluid resuscitation in pancreatitis
- Affiliations
-
- 1Health Education England North East, Newcastle upon Tyne, UK
- 2Northern Surgical Trainees Research Association (NOSTRA), Newcastle upon Tyne, UK
- 3Department of HPB and Transplant Surgery, Freeman Hospital, Newcastle upon Tyne, UK
- KMID: 2548506
- DOI: http://doi.org/10.14701/ahbps.23-044
Abstract
- Backgrounds/Aims
Acute pancreatitis is an emergency presentation, which can range from mild to life threatening. Intravenous fluids are the cornerstone of management. Although the WATERFALL trial described the optimal fluid rate in mild/moderate pancreatitis, this trial excluded patients with moderate-severe/severe pancreatitis. The aim of this study was to establish clinical practice regarding intravenous fluid administration in acute pancreatitis and assess its effect on mortality.
Methods
Prospective multi-centre audit of patients with acute pancreatitis was conducted. Data were collected regarding intravenous fluid administration within 72 hours of admission. The primary outcome was 30-day mortality. Multivariable logistic regression was used to identify predictors of 30-day mortality.
Results
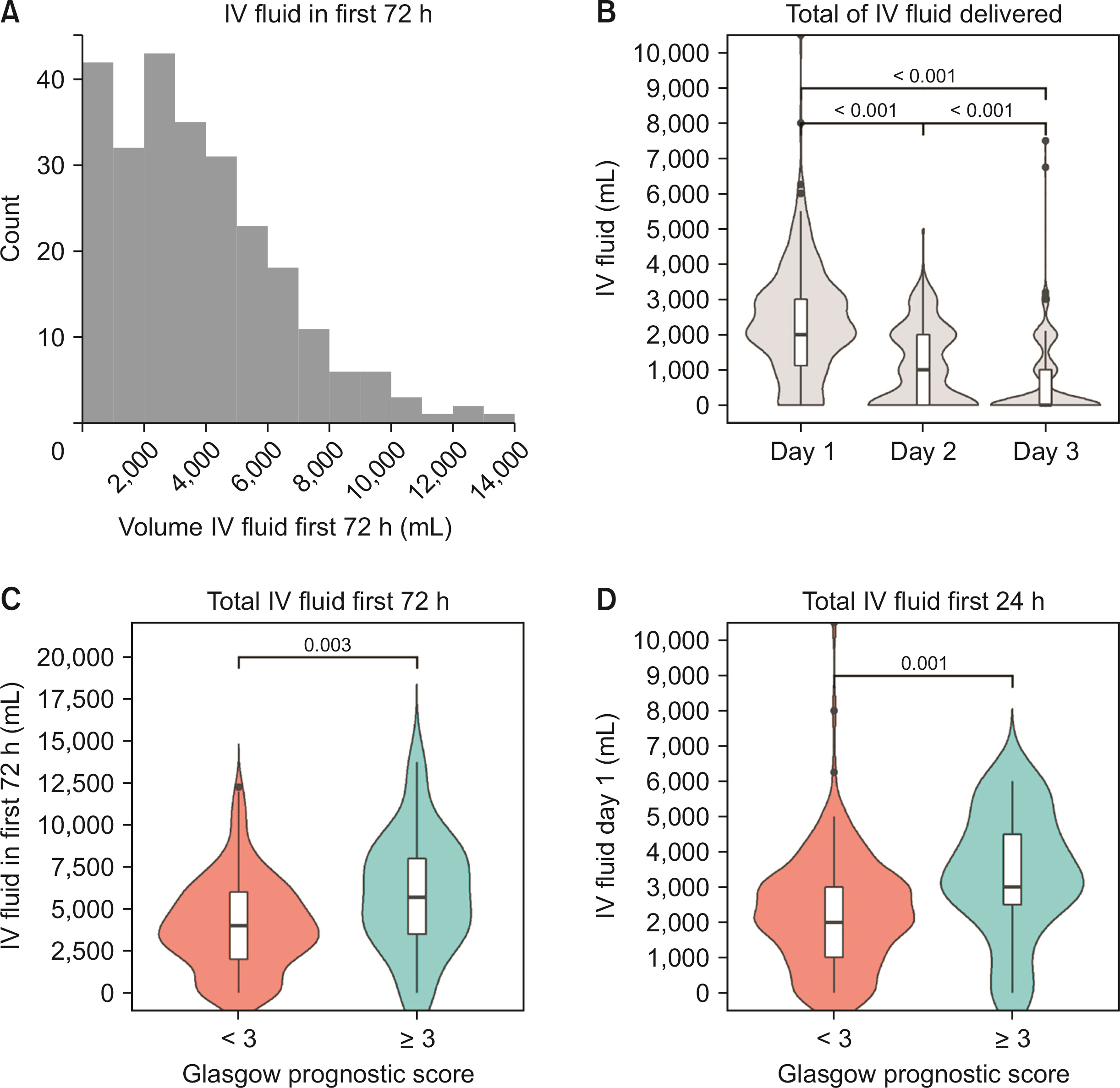
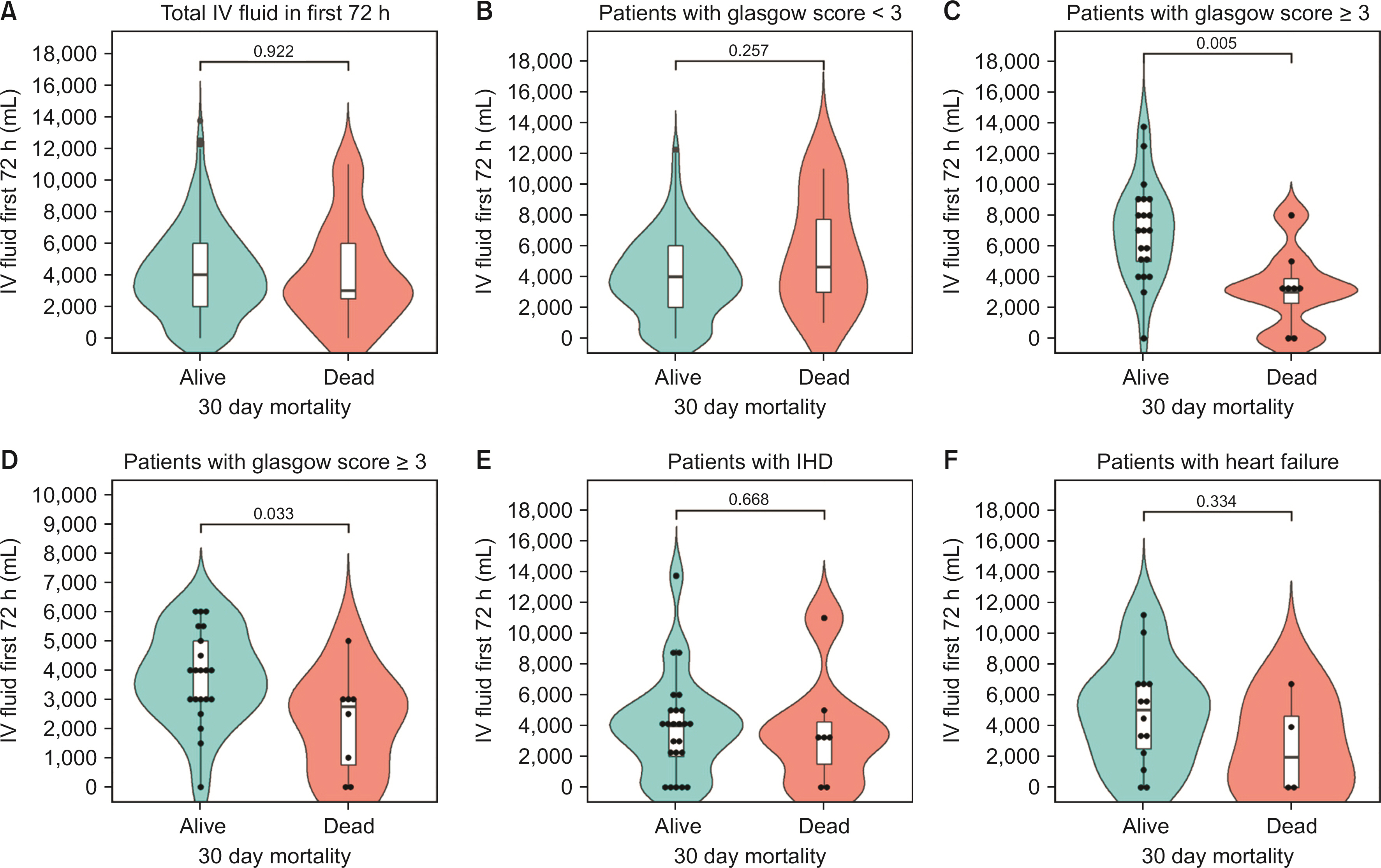
Those with severe pancreatitis received more fluid; median 5.7 L versus 4 L in 72 hours (p = 0.003). Participants with severe pancreatitis who died within 30 days received a median of 2,750 mL in the first 24 hours, compared to 4,000 mL in those who survived. The following factors were significant predictors of 30-day mortality: age, Glasgow score, C-reactive protein, ischaemic heart disease, and pancreatitis aetiology. Overall, volume of intravenous fluid was not associated with mortality. However, the effect of intravenous fluid volume on mortality differed significantly depending on pancreatitis severity. In severe pancreatitis, increased volume of intravenous fluid was associated with significant reductions in mortality (odds ratio = 0.655; 0.459–0.936; p = 0.020).
Conclusions
In severe pancreatitis, more aggressive fluid prescription was associated with decreased mortality; however, this was not the case in milder disease. Further prospective trials guiding fluid resuscitation in severe pancreatitis are needed, as the impact of fluid on this population appears to differ from that in those with milder disease.
Keyword
Figure
Reference
-
1. National Institute for Health and Care Excellence (NICE) guideline: Pancreatitis. NG104 (September 2018) [Internet]. NICE;2018. Available from: https://www.nice.org.uk/guidance/ng104/evidence/full-guideline-pdf-6535536157. cited 2023 Apr 20.2. Koutroumpakis E, Slivka A, Furlan A, Dasyam AK, Dudekula A, Greer JB, et al. 2017; Management and outcomes of acute pancreatitis patients over the last decade: a US tertiary-center experience. Pancreatology. 17:32–40. DOI: 10.1016/j.pan.2016.10.011. PMID: 28341116.3. Schepers NJ, Bakker OJ, Besselink MG, Ahmed Ali U, Bollen TL, Gooszen HG, et al. 2019; Impact of characteristics of organ failure and infected necrosis on mortality in necrotising pancreatitis. Gut. 68:1044–1051. DOI: 10.1136/gutjnl-2017-314657. PMID: 29950344.4. van Dijk SM, Hallensleben NDL, van Santvoort HC, Fockens P, van Goor H, Bruno MJ, et al. 2017; Acute pancreatitis: recent advances through randomised trials. Gut. 66:2024–2032. DOI: 10.1136/gutjnl-2016-313595. PMID: 28838972.5. Blamey SL, Imrie CW, O'Neill J, Gilmour WH, Carter DC. 1984; Prognostic factors in acute pancreatitis. Gut. 25:1340–1346. DOI: 10.1136/gut.25.12.1340. PMID: 6510766. PMCID: PMC1420197.6. Nathens AB, Curtis JR, Beale RJ, Cook DJ, Moreno RP, Romand JA, et al. 2004; Management of the critically ill patient with severe acute pancreatitis. Crit Care Med. 32:2524–2536. DOI: 10.1097/01.CCM.0000148222.09869.92. PMID: 15599161.7. Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis-2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013; 62:102–111. DOI: 10.1136/gutjnl-2012-302779. PMID: 23100216.
Article8. Haydock MD, Mittal A, Wilms HR, Philips A, Petrov MS, Windsor JA. 2013; Fluid therapy in acute pancreatitis: anybody's guess. Ann Surg. 257:182–188. DOI: 10.1097/SLA.0b013e31827773ff. PMID: 23207241.9. Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN. American Gastroenterological Association Institute Clinical Guidelines Committee. 2018; American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology. 154:1096–1101. DOI: 10.1053/j.gastro.2018.01.032. PMID: 29409760.
Article10. Working Party of the British Society of Gastroenterology; Association of Surgeons of Great Britain and Ireland; Pancreatic Society of Great Britain and Ireland; Association of Upper GI Surgeons of Great Britain and Ireland. 2005; UK guidelines for the management of acute pancreatitis. Gut. 54 Suppl 3:iii1–iii9. DOI: 10.1136/gut.2004.057059. PMID: 15888770. PMCID: PMC1867803.11. National Institute for Health and Care Excellence (NICE) clinical guideline [CG174]. Intravenous fluid therapy in adults in hospital (December 2013) [Internet]. NICE;2013. cited 2023 Apr 20. Available from: https://www.nice.org.uk/guidance/cg174/chapter/1-Recommendations.12. Mao EQ, Tang YQ, Fei J, Qin S, Wu J, Li L, et al. 2009; Fluid therapy for severe acute pancreatitis in acute response stage. Chin Med J (Engl). 122:169–173. PMID: 19187641.13. Mao EQ, Fei J, Peng YB, Huang J, Tang YQ, Zhang SD. 2010; Rapid hemodilution is associated with increased sepsis and mortality among patients with severe acute pancreatitis. Chin Med J (Engl). 123:1639–1644. DOI: 10.3410/f.8685963.9200066. PMID: 20819621.14. Messallam AA, Body CB, Berger S, Sakaria SS, Chawla S. 2021; Impact of early aggressive fluid resuscitation in acute pancreatitis. Pancreatology. 21:69–73. DOI: 10.1016/j.pan.2020.11.006. PMID: 33257225.
Article15. Gad MM, Simons-Linares CR. 2020; Is aggressive intravenous fluid resuscitation beneficial in acute pancreatitis? A meta-analysis of randomized control trials and cohort studies. World J Gastroenterol. 26:1098–1106. DOI: 10.3748/wjg.v26.i10.1098. PMID: 32206000. PMCID: PMC7081000.
Article16. de-Madaria E, Buxbaum JL, Maisonneuve P, García García de Paredes A, Zapater P, Guilabert L, et al. 2022; Aggressive or moderate fluid resuscitation in acute pancreatitis. N Engl J Med. 387:989–1000. DOI: 10.1056/NEJMoa2202884. PMID: 36103415.
Article17. Di MY, Liu H, Yang ZY, Bonis PA, Tang JL, Lau J. 2016; Prediction models of mortality in acute pancreatitis in adults: a systematic review. Ann Intern Med. 165:482–490. DOI: 10.7326/M16-0650. PMID: 27454310.
Article18. Working Group IAP/APA Acute Pancreatitis Guidelines. 2013; IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 13:e1–15. DOI: 10.1016/j.pan.2013.07.063. PMID: 24054878.19. Tan YHA, Rafi S, Tyebally Fang M, Hwang S, Lim EW, Ngu J, et al. 2017; Validation of the modified Ranson versus Glasgow score for pancreatitis in a Singaporean population. ANZ J Surg. 87:700–703. DOI: 10.1111/ans.13139. PMID: 25924928.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Severity and Fluid Administration in Acute Pancreatitis
- Medical Management of Acute Pancreatitis and Complications
- Medical Management of Acute Pancreatitis: Intravenous Fluid, Nutrition and Antimicrobial Therapy
- Recent Advances in Management of Acute Pancreatitis
- Pancreaticopleural Fistula: CT Demonstration