Ann Hepatobiliary Pancreat Surg.
2023 Nov;27(4):380-387. 10.14701/ahbps.23-045.
Clinicopathological characteristics of extrahepatic biliary neuroendocrine neoplasms in the gallbladder, extrahepatic biliary tract, and ampulla of Vater: A single-center cross-sectional study
- Affiliations
-
- 1Department of Surgery, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- 2Department of Radiology, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- 3Department of Internal Medicine, Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- KMID: 2548504
- DOI: http://doi.org/10.14701/ahbps.23-045
Abstract
- Backgrounds/Aims
In 2019, the grading and staging system for neuroendocrine neoplasms (NENs) was significantly changed. In this study, we report the clinicopathological characteristics and surgical outcomes of patients with extrahepatic biliary NENs who underwent curative resection with or without adjuvant treatment.
Methods
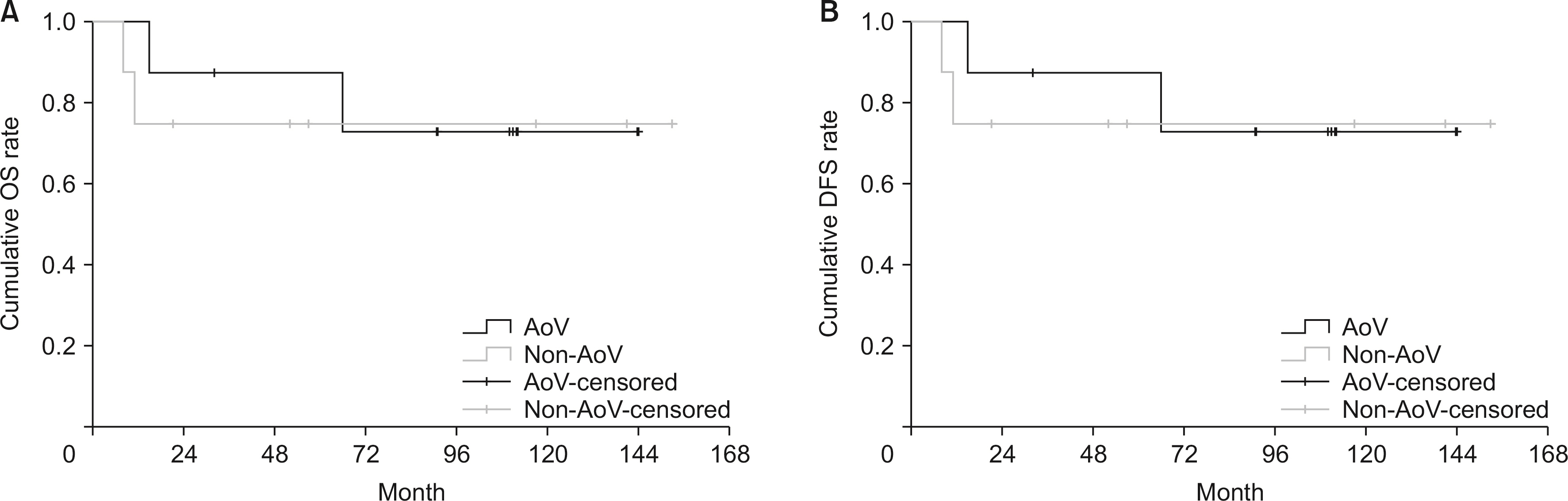
We retrospectively reviewed a database of 16 patients who developed NENs, neuroendocrine carcinoma (NEC), and mixed endocrine non-endocrine neoplasms (MiNENs) after curative resection. Among them, eight patients had ampulla of Vater (AoV) tumors, and eight patients had non-AoV tumors.
Results
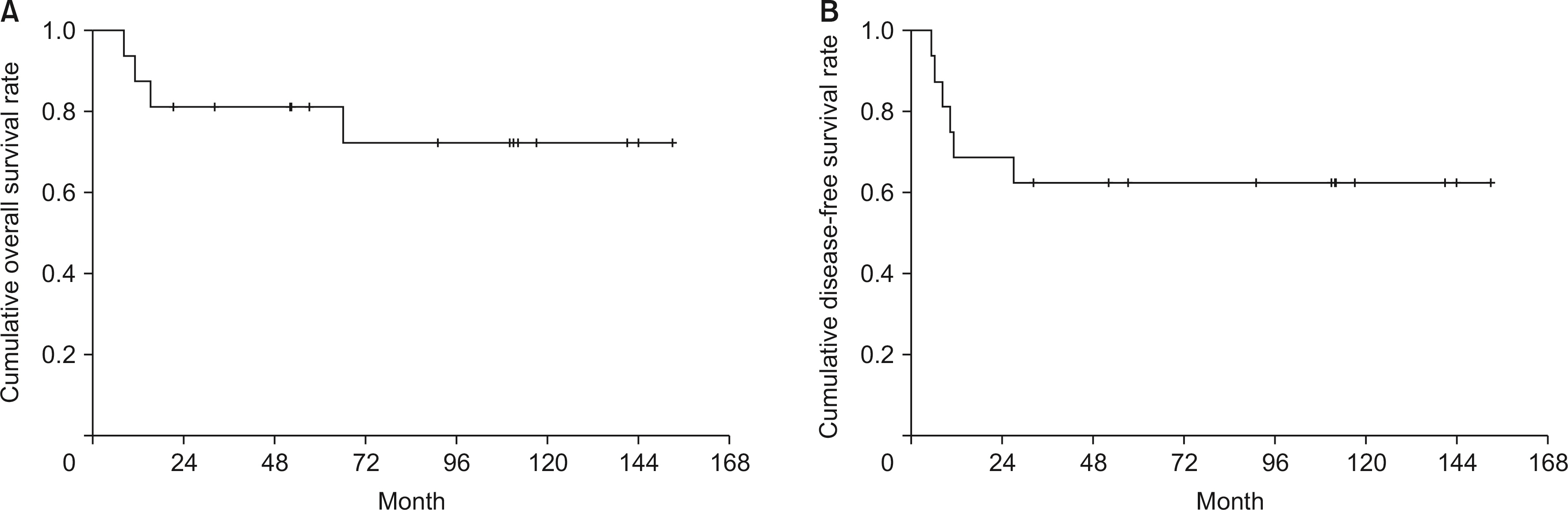
G1 and G2 were more frequently observed in the AoV group than in the non-AoV group (12.5% and 62.5%, respectively). In contrast, NEC and MiNEN were more common in the non-AoV group (50.0%). High Ki-67 index (> 20%) and perineural invasion (PNI) were more frequently observed in the non-AoV group. Advanced age (> 65 years), mitotic count > 20 per 2 mm2 , and Ki-67 index > 20% were strongly correlated with patient survival (p = 0.018, 0.009, and 0.044, respectively). Advanced age (> 65 years) and mitotic count > 20 per 2 mm2 were significantly correlated with disease recurrence (p = 0.033 and 0.010, respectively).
Conclusions
AoV and non-AoV tumors had significant differences in the histologic grade, Ki67, and PNI. Patients with non-AoV tumors had an increased risk for survival and recurrence than those in the AoV group. For extrahepatic biliary NENs, early detection of tumors, adequate surgery, and aggressive adjuvant treatment for high-risk patients are important to achieve long-term survival and prevent disease recurrence.
Keyword
Figure
Reference
-
1. Gustafsson BI, Kidd M, Modlin IM. 2008; Neuroendocrine tumors of the diffuse endocrine system. Curr Opin Oncol. 20:1–12. DOI: 10.1097/CCO.0b013e3282f1c595. PMID: 18043250.2. Modlin IM, Sandor A. 1997; An analysis of 8305 cases of carcinoids tumors. Cancer. 79:813–829. DOI: 10.1002/(SICI)1097-0142(19970215)79:4<813::AID-CNCR19>3.0.CO;2-2.3. Kim J, Lee WJ, Lee SH, Lee KB, Ryu JK, Kim YT, et al. 2011; Clinical features of 20 patients with curatively resected biliary neuroendocrine tumours. Dig Liver Dis. 43:965–970. DOI: 10.1016/j.dld.2011.07.010. PMID: 21856258.
Article4. Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, et al. 2020; The 2019 WHO Classification of tumours of the digestive system. Histopathology. 76:182–188. DOI: 10.1111/his.13975. PMID: 31433515. PMCID: PMC7003895.
Article5. de Mestier L, Cros J, Neuzillet C, Hentic O, Egal A, Muller N, et al. 2017; Digestive system mixed neuroendocrine-non-neuroendocrine neoplasms. Neuroendocrinology. 105:412–425. DOI: 10.1159/000475527. PMID: 28803232.
Article6. Eltawil KM, Gustafsson BI, Kidd M, Modlin IM. 2010; Neuroendocrine tumors of the gallbladder: an evaluation and reassessment of management strategy. J Clin Gastroenterol. 44:687–695. DOI: 10.1097/MCG.0b013e3181d7a6d4. PMID: 20375728.7. Nishime C, Ohnishi Y, Suemizu H, Tamaoki N, Kusumi T, Sato F, et al. 2008; In vivo chemotherapeutic profile of human gallbladder small cell carcinoma. Biomed Res. 29:251–256. DOI: 10.2220/biomedres.29.251. PMID: 18997440.
Article8. Jun SR, Lee JM, Han JK, Choi BI. 2006; High-grade neuroendocrine carcinomas of the gallbladder and bile duct: report of four cases with pathological correlation. J Comput Assist Tomogr. 30:604–609. DOI: 10.1097/00004728-200607000-00009. PMID: 16845291.9. Lane JE, Walker AN, Ayers GW, Foster JL, Williams JT. 2002; Small-cell undifferentiated carcinoma of neuroendocrine type originating in the gallbladder. Curr Surg. 59:495–497. DOI: 10.1016/S0149-7944(02)00638-4. PMID: 15727797.
Article10. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. Neuroendocrine tumors. [Online, 16 December, 2017]. National Comprehensive Cancer Network.11. Klimstra D, Klöppel G, La Rosa S, Rindi G. 2019; Classification of neuroendocrine neoplasms of the digestive system. In: WHO Classification of Tumours Editorial Board, ed. Digestive system tumours WHO classification of tumours. 5th ed. IARC,. 16–19.12. Kim JM, Sohn JH, Kim MJ, Kim KM, Kim WH, et al. Gastrointestinal Pathology Study Group of Korean Society of Pathologists. Current trends of the incidence and pathological diagnosis of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in Korea 2000-2009: multicenter study. Cancer Res Treat. 2012; 44:157–165. DOI: 10.4143/crt.2012.44.3.157. PMID: 23091441. PMCID: PMC3467418.
Article13. Kitano M, Yoshida T, Itonaga M, Tamura T, Hatamaru K, Yamashita Y. 2019; Impact of endoscopic ultrasonography on diagnosis of pancreatic cancer. J Gastroenterol. 54:19–32. DOI: 10.1007/s00535-018-1519-2. PMID: 30406288. PMCID: PMC6314985.
Article14. Burns WR, Edil BH. 2012; Neuroendocrine pancreatic tumors: guidelines for management and update. Curr Treat Options Oncol. 13:24–34. DOI: 10.1007/s11864-011-0172-2. PMID: 22198808.
Article15. Zheng Z, Chen C, Li B, Liu H, Zhou L, Zhang H, et al. 2019; Biliary neuroendocrine neoplasms: clinical profiles, management, and analysis of prognostic factors. Front Oncol. 9:38. DOI: 10.3389/fonc.2019.00038. PMID: 30805307. PMCID: PMC6370735.
Article16. Parekh JR, Wang SC, Bergsland EK, Venook AP, Warren RS, Kim GE, et al. 2012; Lymph node sampling rates and predictors of nodal metastasis in pancreatic neuroendocrine tumor resections: the UCSF experience with 149 patients. Pancreas. 41:840–844. DOI: 10.1097/MPA.0b013e31823cdaa0. PMID: 22781907.
Article17. Lee L, Ito T, Jensen RT. 2019; Prognostic and predictive factors on overall survival and surgical outcomes in pancreatic neuroendocrine neoplasm: recent advances and controversies. Expert Rev Anticancer Ther. 19:1028–1050. DOI: 10.1080/14737140.2019.1693893. PMID: 31738624. PMCID: PMC6923565.18. Jayant M, Punia R, Kaushik R, Sharma R, Sachdev A, Nadkarni NK, et al. 2012; Neuroendocrine tumors of the ampulla of Vater: presentation, pathology and prognosis: presentation. JOP. 13:263–267.19. Modlin IM, Gustafsson BI, Moss SF, Pavel M, Tsolakis AV, Kidd M. 2010; Chromogranin A-biological function and clinical utility in neuro endocrine tumor disease. Ann Surg Oncol. 17:2427–2443. DOI: 10.1245/s10434-010-1006-3. PMID: 20217257.
Article20. Modlin IM, Kidd M, Drozdov I, Siddique ZL, Gustafsson BI. 2008; Pharmacotherapy of neuroendocrine cancers. Expert Opin Pharmacother. 9:2617–2626. DOI: 10.1517/14656566.9.15.2617. PMID: 18803449.
Article21. Iwasa S, Morizane C, Okusaka T, Ueno H, Ikeda M, Kondo S, et al. 2010; Cisplatin and etoposide as first-line chemotherapy for poorly differentiated neuroendocrine carcinoma of the hepatobiliary tract and pancreas. Jpn J Clin Oncol. 40:313–318. DOI: 10.1093/jjco/hyp173. PMID: 20047862.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum: Clinicopathological characteristics of extrahepatic biliary neuroendocrine neoplasms in the gallbladder, extrahepatic biliary tract, and ampulla of Vater: A single-center cross-sectional study
- A Case of Early Carcinoma of the Ampulla of Vater Combined with Adenoma of Colon
- Clinical Characteristics of Biliary Tract Cancer Associated with Choledochal Cyst
- Synchronous Biliary Tract Cancers in a Patient with von Recklinghausen Disease
- A Case of Congenital Agenesis of the Gallbladder without Biliary Atresia associated with Duodenal Web