Ann Rehabil Med.
2023 Oct;47(5):393-402. 10.5535/arm.23058.
Effect of Adding Physiotherapy Program to the Conservative Medical Therapy on Quality of Life and Pain in Chronic Rhinosinusitis Patients
- Affiliations
-
- 1Department of Basic Science for Physical Therapy, Faculty of Physical Therapy, Cairo University, Giza, Egypt
- 2Department of Physical Therapy and Health Rehabilitation, College of Applied Medical Science, Jouf University, Sakaka, Kingdom of Saudi Arabia
- 3Department of Physical Therapy for Surgery, Faculty of Physical Therapy, Cairo University, Giza, Egypt
- 4Department of Biomechanics, Faculty of Physical Therapy, Cairo University, Giza, Egypt
- KMID: 2548399
- DOI: http://doi.org/10.5535/arm.23058
Abstract
Objective
To assess the effectiveness of combining physiotherapy techniques with conservative medical treatment in chronic rhinosinusitis (CRS) patients.
Methods
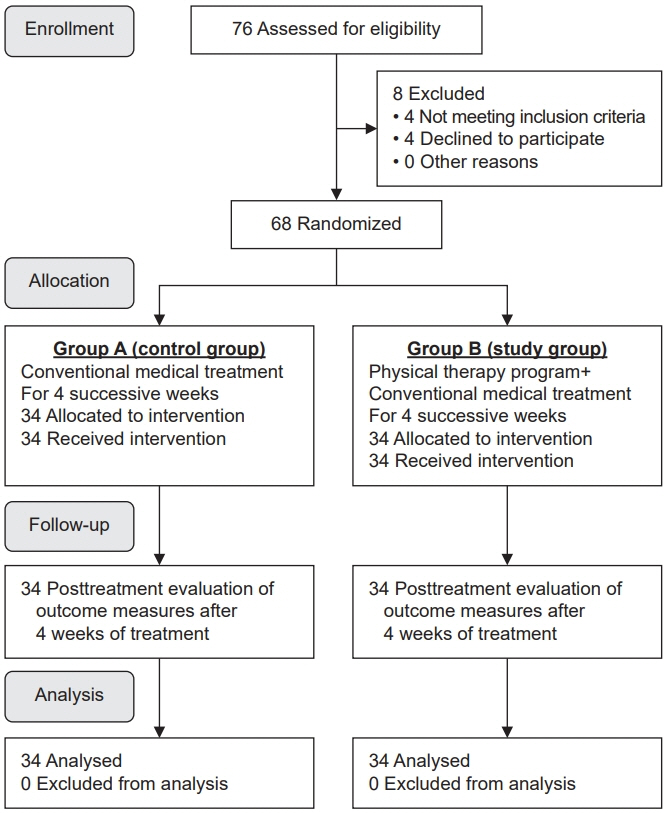
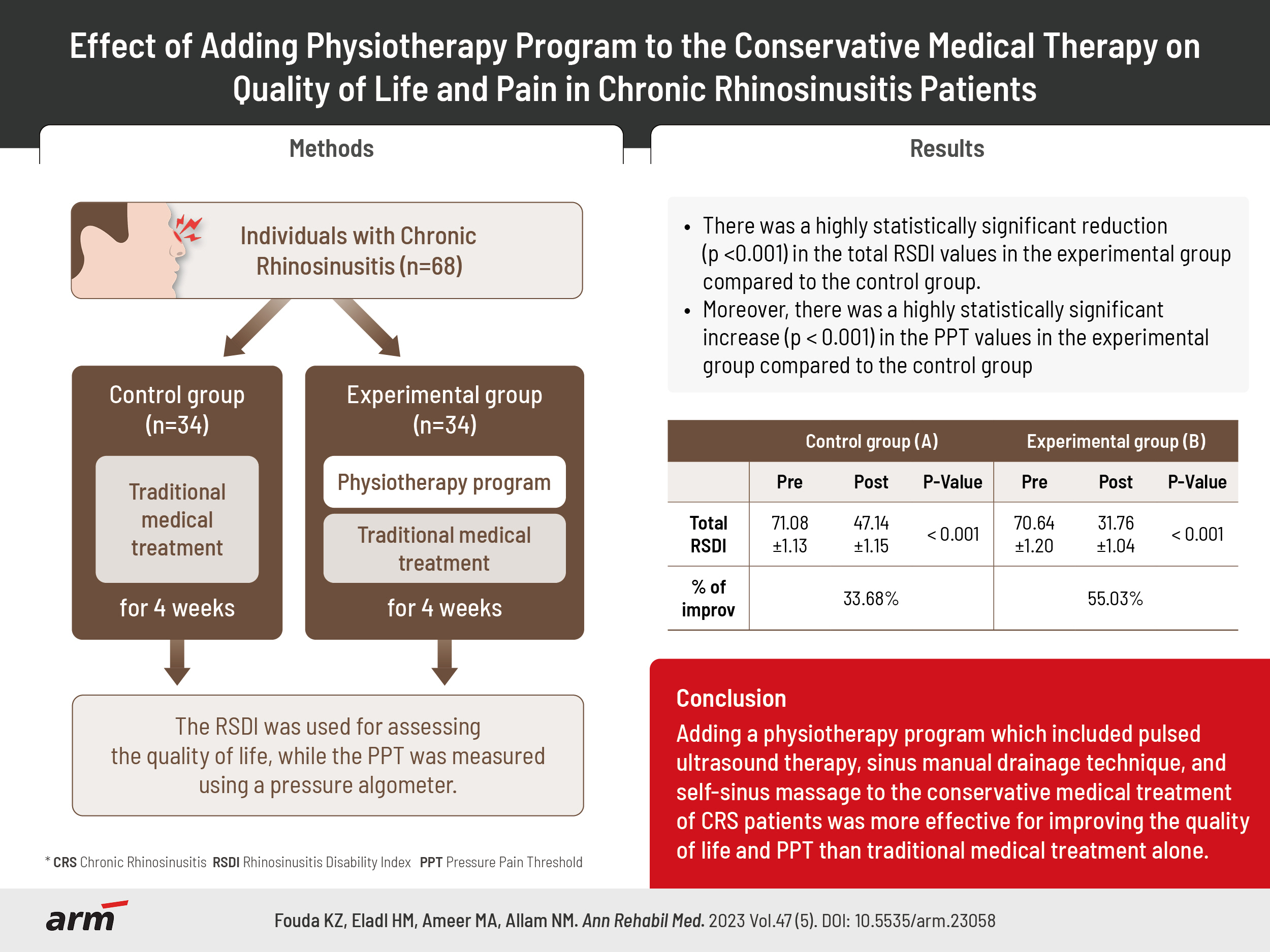
Sixty-eight volunteers with CRS were randomly assigned. Group A received only traditional medical treatment, whereas group B received a physiotherapy program that included pulsed ultrasound therapy, sinus manual drainage techniques, and self-sinus massage technique in addition to traditional medical treatment. Interventions were applied 3 sessions a week for 4 weeks. The rhinosinusitis disability index (RSDI) served as the main outcome indicator for assessing the quality of life, and the secondary outcome measure was the pressure pain threshold (PPT) using a pressure algometer.
Results
Wilcoxon signed rank test revealed a significant reduction (p<0.001) in total RSDI values from 71.08±1.13 pretest to 47.14±1.15 posttest for group A, while it decreased from 70.64±1.20 pretreatment to 31.76±1.04 posttreatment for group B; furthermore, Mann–Whitney U-test revealed a significant difference (p<0.001) in total RSDI values between both groups when comparing the change of the pre-post data values, it was 23.94±0.95 for group A and 38.88±0.67 for group B. The independent t-test revealed a highly statistically significant increase (p<0.001) in the PPT values in the experimental group compared to the control group.
Conclusion
The physiotherapy program which included pulsed ultrasound therapy, sinus manual drainage technique, and self-sinus massage technique in conjunction with conventional medical treatment was more beneficial for enhancing the quality of life and PPT than traditional medical treatment alone in CRS patients.
Figure
Reference
-
1. Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Brook I, Ashok Kumar K, Kramper M, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015; 152(2 Suppl):S1–39.
Article2. Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology. 2020; 58(Suppl S29):1–464.3. Levy JM, Marino MJ, McCoul ED. Paranasal sinus balloon catheter dilation for treatment of chronic rhinosinusitis: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2016; 154:33–40.
Article4. Rudmik L, Smith TL, Schlosser RJ, Hwang PH, Mace JC, Soler ZM. Productivity costs in patients with refractory chronic rhinosinusitis. Laryngoscope. 2014; 124:2007–12.
Article5. Orlandi RR, Kingdom TT, Hwang PH. International Consensus Statement on Allergy and Rhinology: Rhinosinusitis executive summary. Int Forum Allergy Rhinol. 2016; 6 Suppl 1:S3–21.
Article6. Bova R. Treatment decisions in adult rhinosinusitis. MedicineToday. 2011; 12:16–26.7. Peters AT, Spector S, Hsu J, Hamilos DL, Baroody FM, Chandra RK, et al. Diagnosis and management of rhinosinusitis: a practice parameter update. Ann Allergy Asthma Immunol. 2014; 113:347–85.
Article8. Ansari NN, Naghdi S, Fathali M, Bartley J, Rastak MS. A randomized clinical trial comparing pulsed ultrasound and erythromycin phonophoresis in the treatment of patients with chronic rhinosinusitis. Physiother Theory Pract. 2015; 31:166–72.
Article9. Ansari NN, Fathali M, Naghdi S, Hasson S, Jalaie S, Rastak MS. A randomized, double-blind clinical trial comparing the effects of continuous and pulsed ultrasound in patients with chronic rhinosinusitis. Physiother Theory Pract. 2012; 28:85–94.
Article10. Feizabadi N, Sarrafzadeh J, Fathali M, Vasaghi-Gharamaleki B, Dadgoo M, Kardan-Yamchi J, et al. The pulsed ultrasound strategy effectively decreases the S. aureus population of chronic rhinosinusitis patients. BMC Res Notes. 2019; 12:576.
Article11. De Castro RB, Cruz-Daylo MAB, Jardin MLA. Low frequency ultrasound in Chronic Rhinosinusitis with Nasal Polyposis and recovery after endoscopic sinus surgery: a randomized controlled trial. Philipp J Otolaryngol Head Neck Surg. 2017; 32:6–13.
Article12. Bartley J, Ansari NN, Naghdi S. Therapeutic ultrasound as a treatment modality for chronic rhinosinusitis. Curr Infect Dis Rep. 2014; 16:398.
Article13. Rocha WA, Rodrigues KM, Pereira RR, Nogueira BV, Gonçalves WL. [Acute effects of therapeutic 1-MHz ultrasound on nasal unblocking of subjects with chronic rhinosinusitis]. Braz J Otorhinolaryngol. 2011; 77:7–12. Portuguese.14. da Silva GS, Dos Santos Isoppo K. Therapeutic ultrasound as a treatment for chronic rhinosinusitis: a systematic review. Clin Respir J. 2021; 15:1275–85.
Article15. Méndez-Sánchez R, González-Iglesias J, Puente-González AS, Sánchez-Sánchez JL, Puentedura EJ, Fernández-de-Las-Peñas C. Effects of manual therapy on craniofacial pain in patients with chronic rhinosinusitis: a case series. J Manipulative Physiol Ther. 2012; 35:64–72.
Article16. Baisakhiya N. Efficacy of osteopathic manipulative treatment in the patient of chronic rhinosinusitis: a case report. Clin Rhinol An Int J. 2018; 11:58–60.
Article17. Lee-Wong M, Karagic M, Doshi A, Gomez S, Resnick D. An osteopathic approach to chronic sinusitis. J Aller Ther. 2011; 2:109.
Article18. Naghdi S, Ansari NN, Fathali M, Bartley J, Varedi M, Honarpishe R. A pilot study into the effect of low-level laser therapy in patients with chronic rhinosinusitis. Physiother Theory Pract. 2013; 29:596–603.
Article19. Kalekar S, Gurudut P. Effect of therapeutic ultrasound versus shortwave diathermy combined with suboccipital release and manual drainage techniques for chronic sinusitis: a randomized clinical trial. Indian J Phys Ther Res. 2019; 1:29–36.20. Ahmadi F, Rostami F, Mahdavi R. The effect of therapeutic massage on the athletes with chronic sinusitis. J Paramed Sci Rehabil. 2017; 6:83–90.21. Bahraini S. The effect of facial and head massage on the pain severity of sinus headache. J Paramed Sci Rehabil. 2014; 3:68–73.22. Aldrees T, Almubarak Z, Hassouneh B, Albosaily A, Aloulah M, Almasoud M, et al. Translation, validation, and cultural adaptation of the Rhinosinusitis Disability Index and the Chronic Sinusitis Survey into Arabic. Ann Saudi Med. 2018; 38:159–66.
Article23. Lehrer-Coriat E, Mariño-Sánchez F, Alobid I, Mullol J. Quality of life measures in patients on rhinosinusitis trials. Clin Invest. 2013; 3:251–63.
Article24. Al Sayah F, Ishaque S, Lau D, Johnson JA. Health related quality of life measures in Arabic speaking populations: a systematic review on cross-cultural adaptation and measurement properties. Qual Life Res. 2013; 22:213–29.
Article25. Park G, Kim CW, Park SB, Kim MJ, Jang SH. Reliability and usefulness of the pressure pain threshold measurement in patients with myofascial pain. Ann Rehabil Med. 2011; 35:412–7.
Article26. Knapstad MK, Nordahl SHG, Naterstad IF, Ask T, Skouen JS, Goplen FK. Measuring pressure pain threshold in the cervical region of dizzy patients- the reliability of a pressure algometer. Physiother Res Int. 2018; 23:e1736.
Article27. Kamińska A, Dalewski B, Sobolewska E. The usefulness of the pressure algometer in the diagnosis and treatment of orofacial pain patients: a systematic review. Occup Ther Int. 2020; 2020:5168457.
Article28. Bartley J, Young D. Ultrasound as a treatment for chronic rhinosinusitis. Med Hypotheses. 2009; 73:15–7.
Article29. Rediske AM, Roeder BL, Nelson JL, Robison RL, Schaalje GB, Robison RA, et al. Pulsed ultrasound enhances the killing of Escherichia coli biofilms by aminoglycoside antibiotics in vivo. Antimicrob Agents Chemother. 2000; 44:771–2.
Article30. Carmen JC, Roeder BL, Nelson JL, Ogilvie RL, Robison RA, Schaalje GB, et al. Treatment of biofilm infections on implants with low-frequency ultrasound and antibiotics. Am J Infect Control. 2005; 33:78–82.
Article31. Ensing GT, Roeder BL, Nelson JL, van Horn JR, van der Mei HC, Busscher HJ, et al. Effect of pulsed ultrasound in combination with gentamicin on bacterial viability in biofilms on bone cements in vivo. J Appl Microbiol. 2005; 99:443–8.
Article32. Ansari NN, Naghdi S, Farhadi M, Jalaie S. A preliminary study into the effect of low-intensity pulsed ultrasound on chronic maxillary and frontal sinusitis. Physiother Theory Pract. 2007; 23:211–8.
Article33. Polat BE, Hart D, Langer R, Blankschtein D. Ultrasound-mediated transdermal drug delivery: mechanisms, scope, and emerging trends. J Control Release. 2011; 152:330–48.
Article34. Young D, Morton R, Bartley J. Therapeutic ultrasound as treatment for chronic rhinosinusitis: preliminary observations. J Laryngol Otol. 2010; 124:495–9.
Article35. Gandhi M, Gurudut P. Comparative effectiveness of jade stone mobilisation, non-abrasive cupping, and manual drainage technique in subjects with chronic sinusitis: a randomized clinical trial. Internet J Allied Health Sci Pract. 2022; 20:21.
Article36. Schenkel EJ, Messina Jr. JC, Bodine A, Mcginley JS, Wirth RJ, Mahmoud RA. Disease burden of chronic rhinosinusitis (CRS) is as severe as other serious chronic diseases. J Allergy Clin Immunol. 2018; 141(2 Suppl):AB165.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of Opioid Analgesics for the Management of Chronic Noncancer Pain
- Inverse Electrode Placement May Help to Improve Electrotherapeutic Effects in the Field of Chronic Pain Management
- Effects of Pain, Sleep Disturbance, and Fatigue on the Quality of Life in Patients with Pancreatic Cancer Undergoing Chemotherapy
- Medical treatment according to phenotypes of chronic rhinosinusitis
- The Predictive Factors of Olfactory Changes after Endoscopic Sinus Surgery