Korean Circ J.
2023 Nov;53(11):775-786. 10.4070/kcj.2023.0108.
Tricuspid Edge-to-Edge Repair Versus Tricuspid Valve Replacement for Severe Tricuspid Regurgitation
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Kangnam Sacred Heart Hospital, Hallym University Medical Center, Hallym University College of Medicine, Seoul, Korea
- 2Department of Thoracic and Cardiovascular Surgery, Bucheon Sejong Hospital, Bucheon, Korea
- 3Division of Cardiology, Department of Internal Medicine, Bucheon Sejong Hospital, Bucheon, Korea
- 4Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2548240
- DOI: http://doi.org/10.4070/kcj.2023.0108
Abstract
- Background and Objectives
Tricuspid valve (TV) repair techniques other than annuloplasty remain challenging and frequently end in tricuspid valve replacement (TVR) in complicated cases. However, the results of TVR are suboptimal compared with TV repair. This study aimed to evaluate the clinical effectiveness of TV edge-to-edge repair (E2E) compared to TVR for severe tricuspid regurgitation (TR).
Methods
We retrospectively reviewed 230 patients with severe TR who underwent E2E (n=139) or TVR (n=91) from 2001 to 2020. Clinical and echocardiographic results were analyzed using inverse probability of treatment weighting analysis and propensity score matching.
Results
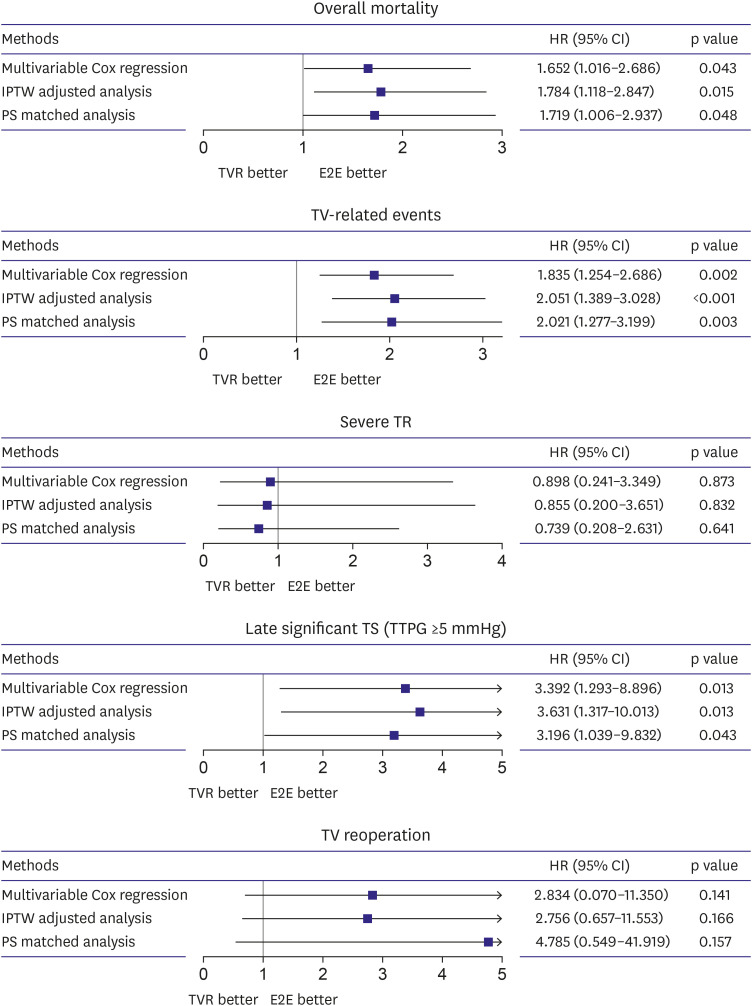
The two groups showed no significant differences in early mortality and morbidities. During the mean follow-up of 106.2±68.8 months, late severe TR and TV reoperation rates were not significantly different between groups. E2E group, however, showed better outcomes in overall survival (p=0.023), freedom from significant tricuspid stenosis (TS) (trans-tricuspid pressure gradient ≥5 mmHg, p=0.021), and freedom from TVrelated events (p<0.001). Matched analysis showed consistent results.
Conclusions
E2E for severe TR presented more favorable clinical outcomes than TVR. Our study supports that E2E might be a valuable option in severe TR surgery, avoiding TVR.
Keyword
Figure
Cited by 1 articles
-
Be Prepared: New Era of Heart-Team Approach for the Treatment of Tricuspid Regurgitation
Cheong Lim, Joon Chul Jung
Korean Circ J. 2023;53(11):787-789. doi: 10.4070/kcj.2023.0225.
Reference
-
1. Fukuda S, Song JM, Gillinov AM, et al. Tricuspid valve tethering predicts residual tricuspid regurgitation after tricuspid annuloplasty. Circulation. 2005; 111:975–979. PMID: 15710756.
Article2. Rodés-Cabau J, Taramasso M, O’Gara PT. Diagnosis and treatment of tricuspid valve disease: current and future perspectives. Lancet. 2016; 388:2431–2442. PMID: 27048553.
Article3. Wong WK, Chen SW, Chou AH, et al. Late outcomes of valve repair versus replacement in isolated and concomitant tricuspid valve surgery: a nationwide cohort study. J Am Heart Assoc. 2020; 9:e015637. PMID: 32301369.
Article4. Alkhouli M, Berzingi C, Kowatli A, Alqahtani F, Badhwar V. Comparative early outcomes of tricuspid valve repair versus replacement for secondary tricuspid regurgitation. Open Heart. 2018; 5:e000878. PMID: 30228911.
Article5. Choi JW, Jang MJ, Kim KH, Hwang HY. Repair versus replacement for the surgical correction of tricuspid regurgitation: a meta-analysis. Eur J Cardiothorac Surg. 2018; 53:748–755. PMID: 29228165.
Article6. Jang JY, Heo R, Lee S, et al. Comparison of results of tricuspid valve repair versus replacement for severe functional tricuspid regurgitation. Am J Cardiol. 2017; 119:905–910. PMID: 28214000.
Article7. Fucci C, Sandrelli L, Pardini A, Torracca L, Ferrari M, Alfieri O. Improved results with mitral valve repair using new surgical techniques. Eur J Cardiothorac Surg. 1995; 9:621–626. PMID: 8751250.8. De Bonis M, Lapenna E, La Canna G, et al. A novel technique for correction of severe tricuspid valve regurgitation due to complex lesions. Eur J Cardiothorac Surg. 2004; 25:760–765. PMID: 15082279.
Article9. Lai YQ, Meng X, Bai T, Zhang C, Luo Y, Zhang ZG. Edge-to-edge tricuspid valve repair: an adjuvant technique for residual tricuspid regurgitation. Ann Thorac Surg. 2006; 81:2179–2182. PMID: 16731150.
Article10. Lee H, Kim J, Oh SS, Yoo JS. Long-term clinical and hemodynamic outcomes of edge-to-edge repair for tricuspid regurgitation. Ann Thorac Surg. 2021; 112:803–808. PMID: 33157062.
Article11. Castedo E, Cañas A, Cabo RA, Burgos R, Ugarte J. Edge-to-edge tricuspid repair for redeveloped valve incompetence after DeVega’s annuloplasty. Ann Thorac Surg. 2003; 75:605–606. PMID: 12607693.
Article12. Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017; 30:303–371. PMID: 28314623.
Article13. Foale R, Nihoyannopoulos P, McKenna W, et al. Echocardiographic measurement of the normal adult right ventricle. Br Heart J. 1986; 56:33–44. PMID: 3730205.
Article14. Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice. J Am Soc Echocardiogr. 2009; 22:1–23. PMID: 19130998.
Article15. Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014; 33:1242–1258. PMID: 24122911.
Article16. Writing Committee Members. Otto CM, Nishimura RA, et al. 2020 ACC/AHA Guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021; 77:e25–197. PMID: 33342586.17. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022; 43:561–632. PMID: 34453165.18. Marquis-Gravel G, Bouchard D, Perrault LP, et al. Retrospective cohort analysis of 926 tricuspid valve surgeries: clinical and hemodynamic outcomes with propensity score analysis. Am Heart J. 2012; 163:851–858.e1. PMID: 22607864.
Article19. Lee H, Sung K, Kim WS, et al. Clinical and hemodynamic influences of prophylactic tricuspid annuloplasty in mechanical mitral valve replacement. J Thorac Cardiovasc Surg. 2016; 151:788–795. PMID: 26778212.
Article20. Chikwe J, Itagaki S, Anyanwu A, Adams DH. Impact of concomitant tricuspid annuloplasty on tricuspid regurgitation, right ventricular function, and pulmonary artery hypertension after repair of mitral valve prolapse. J Am Coll Cardiol. 2015; 65:1931–1938. PMID: 25936265.
Article21. Boyd JH, Edelman JJ, Scoville DH, Woo YJ. Tricuspid leaflet repair: innovative solutions. Ann Cardiothorac Surg. 2017; 6:248–254. PMID: 28706867.
Article22. Lapenna E, De Bonis M, Verzini A, et al. The clover technique for the treatment of complex tricuspid valve insufficiency: midterm clinical and echocardiographic results in 66 patients. Eur J Cardiothorac Surg. 2010; 37:1297–1303. PMID: 20117940.
Article23. Negm S, Arafat AA, Elatafy EE, Fawzy HF. Mechanical versus bioprosthetic valve replacement in the tricuspid valve position: a systematic review and meta-analysis. Heart Lung Circ. 2021; 30:362–371. PMID: 33229238.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Permanent Pacemaker Lead Induced Severe Tricuspid Regurgitation in Patient Undergoing Multiple Valve Surgery
- Tricuspid Valve Re-Repair in Ebstein Anomaly Using the Cone Technique
- Tricuspid Valve Repair for Tricuspid Valve Insufficiency Following a Cardiac Stab Injury
- Repair of Posttraumatic Tricuspid Regurgitation Using Artificial Chordae and an Annuloplasty Ring
- Chordae Tendineae Approximation Technique for Severe Tricuspid Regurgitation with Severe Leaflet Tethering Using a Totally Endoscopic Beating-Heart Strategy: A Case Report