Korean Circ J.
2023 Nov;53(11):744-755. 10.4070/kcj.2023.0022.
Early Aortic Valve Replacement in Symptomatic Normal-Flow, LowGradient Severe Aortic Stenosis: A Propensity Score–Matched Retrospective Cohort Study
- Affiliations
-
- 1Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Cardiothoracic Surgery, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2548236
- DOI: http://doi.org/10.4070/kcj.2023.0022
Abstract
- Background and Objectives
Aortic valve replacement (AVR) is considered a class I indication for symptomatic severe aortic stenosis (AS). However, there is little evidence regarding the potential benefits of early AVR in symptomatic patients diagnosed with normal-flow, low-gradient (NFLG) severe AS.
Methods
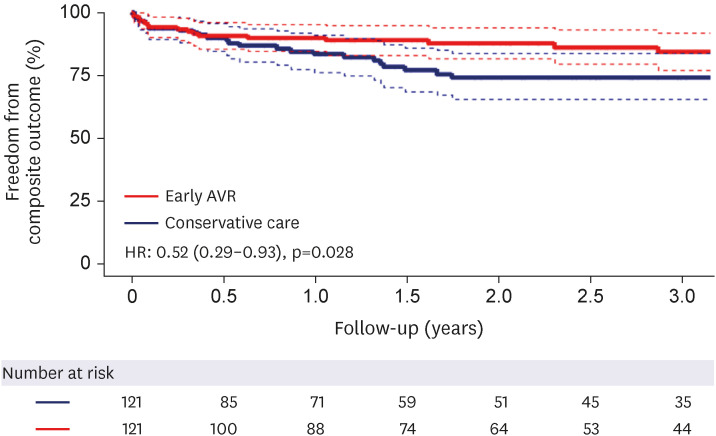
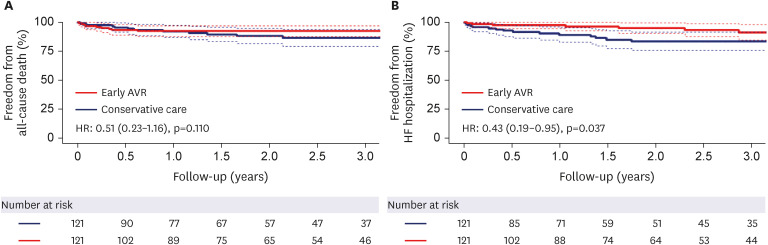
Two-hundred eighty-one patients diagnosed with symptomatic NFLG severe AS (stroke volume index ≥35 mL/m 2 , mean transaortic pressure gradient <40 mmHg, peak transaortic velocity <4 m/s, and aortic valve area <1.0 cm 2 ) between January 2010 and December 2020 were included in this retrospective study. After performing 1:1 propensity score matching, 121 patients aged 75.1±9.8 years (including 63 women) who underwent early AVR within 3 months after index echocardiography, were compared with 121 patients who received conservative care. The primary outcome was a composite of all-cause death and heart failure (HF) hospitalization.
Results
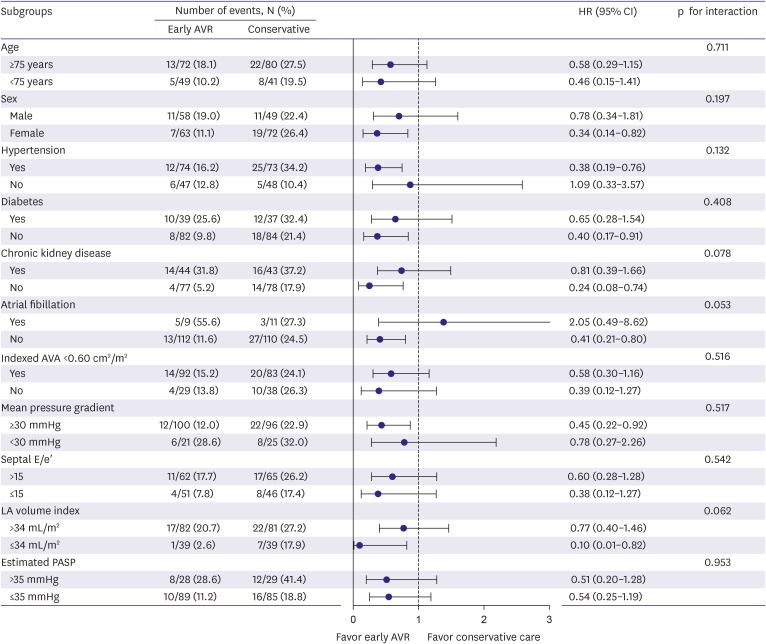
During a median follow-up of 21.9 months, 48 primary outcomes (18 in the early AVR group and 30 in the conservative care group) occurred. The early AVR group demonstrated a significantly lower incidence of primary outcomes (hazard ratio [HR], 0.52; 95% confidence interval [CI], 0.29–0.93; p=0.028); specifically, there was no significant difference in all-cause death (HR, 0.51; 95% CI, 0.23–1.16; p=0.110), although the early AVR group showed a significantly lower incidence of hospitalization for HF (HR, 0.43; 95% CI, 0.19–0.95, p=0.037). Subgroup analyses supported the main findings.
Conclusions
An early AVR strategy may be beneficial in reducing the risk of a composite outcome of death or hospitalization for HF in symptomatic patients with NFLG severe AS. Future randomized studies are required to validate and confirm our findings.
Keyword
Figure
Cited by 1 articles
-
Reconsidering the Timing of Aortic Valve Replacement in Symptomatic Normal-Flow Low-Gradient Severe Aortic Stenosis
Hsin-Fu Lee
Korean Circ J. 2023;53(11):756-757. doi: 10.4070/kcj.2023.0183.
Reference
-
1. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2021; 143:e35–e71. PMID: 33332149.2. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022; 43:561–632. PMID: 34453165.3. Minners J, Allgeier M, Gohlke-Baerwolf C, Kienzle RP, Neumann FJ, Jander N. Inconsistencies of echocardiographic criteria for the grading of aortic valve stenosis. Eur Heart J. 2008; 29:1043–1048. PMID: 18156619.
Article4. Berthelot-Richer M, Pibarot P, Capoulade R, et al. Discordant grading of aortic stenosis severity: echocardiographic predictors of survival benefit associated with aortic valve replacement. JACC Cardiovasc Imaging. 2016; 9:797–805. PMID: 27209111.5. Clavel MA, Burwash IG, Pibarot P. Cardiac imaging for assessing low-gradient severe aortic stenosis. JACC Cardiovasc Imaging. 2017; 10:185–202. PMID: 28183438.
Article6. Strange G, Stewart S, Celermajer D, et al. Poor long-term survival in patients with moderate aortic stenosis. J Am Coll Cardiol. 2019; 74:1851–1863. PMID: 31491546.
Article7. Li SX, Patel NK, Flannery LD, et al. Trends in utilization of aortic valve replacement for severe aortic stenosis. J Am Coll Cardiol. 2022; 79:864–877. PMID: 35241220.
Article8. Clavel MA, Guzzetti E, Annabi MS, Salaun E, Ong G, Pibarot P. Normal-flow low-gradient severe aortic stenosis: myth or reality? Struct Heart. 2018; 2:180–187.
Article9. Kang DH, Jang JY, Park SJ, et al. Watchful observation versus early aortic valve replacement for symptomatic patients with normal flow, low-gradient severe aortic stenosis. Heart. 2015; 101:1375–1381. PMID: 26105038.
Article10. Saeed S, Vamvakidou A, Seifert R, Khattar R, Li W, Senior R. The impact of aortic valve replacement on survival in patients with normal flow low gradient severe aortic stenosis: a propensity-matched comparison. Eur Heart J Cardiovasc Imaging. 2019; 20:1094–1101. PMID: 31327014.
Article11. Zusman O, Pressman GS, Banai S, Finkelstein A, Topilsky Y. Intervention versus observation in symptomatic patients with normal flow low gradient severe aortic stenosis. JACC Cardiovasc Imaging. 2018; 11:1225–1232. PMID: 29055632.
Article12. Taniguchi T, Morimoto T, Shiomi H, et al. High- versus low-gradient severe aortic stenosis: demographics, clinical outcomes, and effects of the initial aortic valve replacement strategy on long-term prognosis. Circ Cardiovasc Interv. 2017; 10:e004796. PMID: 28500139.13. Nashef SA, Roques F, Sharples LD, et al. EuroSCORE II. Eur J Cardiothorac Surg. 2012; 41:734–744. PMID: 22378855.
Article14. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14. PMID: 25559473.
Article15. Baumgartner H, Hung J, Bermejo J, et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2017; 30:372–392. PMID: 28385280.
Article16. Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography developed in collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2017; 30:303–371. PMID: 28314623.
Article17. Harris H, Horst SJ. A brief guide to decisions at each step of the propensity score matching process. Pract Assess Res Eval. 2016; 21:4.18. Zhao QY, Luo JC, Su Y, Zhang YJ, Tu GW, Luo Z. Propensity score matching with R: conventional methods and new features. Ann Transl Med. 2021; 9:812. PMID: 34268425.
Article19. VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017; 167:268–274. PMID: 28693043.
Article20. Mantovani F, Fanti D, Tafciu E, et al. When aortic stenosis is not alone: epidemiology, pathophysiology, diagnosis and management in mixed and combined valvular disease. Front Cardiovasc Med. 2021; 8:744497. PMID: 34722676.
Article21. Tribouilloy C, Rusinaru D, Maréchaux S, et al. Low-gradient, low-flow severe aortic stenosis with preserved left ventricular ejection fraction: characteristics, outcome, and implications for surgery. J Am Coll Cardiol. 2015; 65:55–66. PMID: 25572511.
Article22. Wilson JB, Jackson LR 2nd, Ugowe FE, et al. Racial and ethnic differences in treatment and outcomes of severe aortic stenosis: a review. JACC Cardiovasc Interv. 2020; 13:149–156. PMID: 31973792.
Article23. Ryu DR, Park SJ, Han H, et al. Progression rate of aortic valve stenosis in Korean patients. J Cardiovasc Ultrasound. 2010; 18:127–133. PMID: 21253361.
Article24. Dayan V, Vignolo G, Magne J, Clavel MA, Mohty D, Pibarot P. Outcome and impact of aortic valve replacement in patients with preserved LVEF and low-gradient aortic stenosis. J Am Coll Cardiol. 2015; 66:2594–2603. PMID: 26670058.
Article25. Chadha G, Bohbot Y, Lachambre P, et al. Progression of normal flow low gradient “severe” aortic stenosis with preserved left ventricular ejection fraction. Am J Cardiol. 2020; 128:151–158. PMID: 32650909.
Article26. Eleid MF, Sorajja P, Michelena HI, Malouf JF, Scott CG, Pellikka PA. Flow-gradient patterns in severe aortic stenosis with preserved ejection fraction: clinical characteristics and predictors of survival. Circulation. 2013; 128:1781–1789. PMID: 24048203.
Article27. Banovic M, Putnik S, Penicka M, et al. Aortic valve replacement versus conservative treatment in asymptomatic severe aortic stenosis: the AVATAR trial. Circulation. 2022; 145:648–658. PMID: 34779220.28. Solomon SD, McMurray JJ, Claggett B, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med. 2022; 387:1089–1098. PMID: 36027570.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unicommisural Unicuspid Aortic Valve with Very Severe Aortic Stenosis in a 17-Year-Old Female
- Expanding transcatheter aortic valve replacement into uncharted indications
- Aortic Stenosis and Transcatheter Aortic Valve Implantation: Current Status and Future Directions in Korea
- Right Coronary Artery Ostial Stenosis after Re-do Aortic Valve Replacement
- Bentall Operation in a Patient with a Unicommissural Unicuspid Aortic Valve