Restor Dent Endod.
2022 Nov;47(4):e38. 10.5395/rde.2022.47.e38.
Calcium-doped zinc oxide nanocrystals as an innovative intracanal medicament: a pilot study
- Affiliations
-
- 1Department of Endodontics, School of Dentistry, Federal University of Uberlândia, Uberlândia, MG, Brazil
- 2School of Dentistry, Federal University of Uberlândia, Uberlândia, MG, Brazil
- 3Department of Oral Diagnosis, School of Dentistry, Federal University of Uberlândia, Uberlândia, MG, Brazil
- 4Functional and New Nanostructured Materials Laboratory, Physics Institute, Federal University of Alagoas, Maceió, AL, Brazil
- KMID: 2548142
- DOI: http://doi.org/10.5395/rde.2022.47.e38
Abstract
Objectives
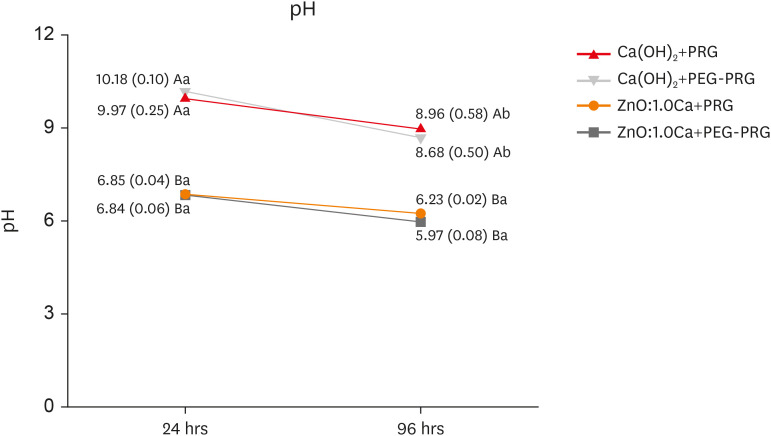
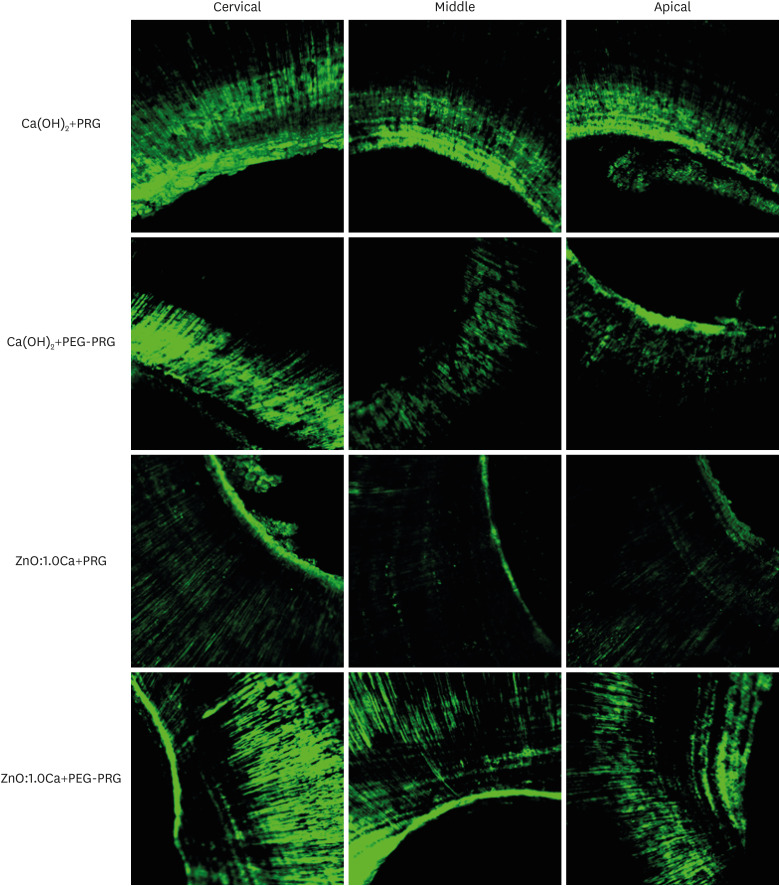
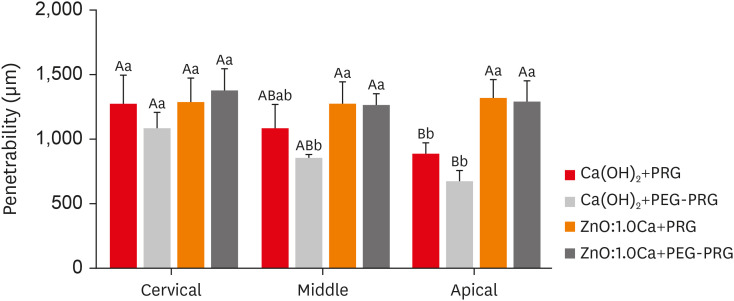
This study investigated the cytotoxicity, radiopacity, pH, and dentinal tubule penetration of a paste of 1.0% calcium-doped zinc oxide nanocrystals (ZnO:1.0Ca) combined with propylene glycol (PRG) or polyethylene glycol and propylene glycol (PEG-PRG).
Materials and Methods
The pastes were prepared by mixing calcium hydroxide [Ca(OH) 2 ] or ZnO:1.0Ca with PRG or a PEG-PRG mixture. The pH was evaluated after 24 and 96 hours of storage in deionized water. Digital radiographs were acquired for radiopacity analysis and bubble counting of each material. The materials were labeled with 0.1% fluorescein and applied to root canals, and images of their dentinal tubule penetration were obtained using confocal laser scanning microscopy. RAW264.7 macrophages were placed in different dilutions of culture media previously exposed to the materials for 24 and 96 hours and tested for cell viability using the MTT assay. Analysis of variance and the Tukey test (α = 0.05) were performed.
Results
ZnO:1.0Ca materials showed lower viability at 1:1 and 1:2 dilutions than Ca(OH)2 materials (p < 0.0001). Ca(OH)2 had higher pH values than ZnO:1.0Ca at 24 and 96 hours, regardless of the vehicle (p < 0.05). ZnO:1.0Ca pastes showed higher radiopacity than Ca(OH)2 pastes (p < 0.01). No between-material differences were found in bubble counting (p = 0.0902). The ZnO:1.0Ca pastes had a greater penetration depth than Ca(OH)2 in the apical third (p < 0.0001).
Conclusions
ZnO:1.0Ca medicaments presented higher penetrability, cell viability, and radiopacity than Ca(OH)2 . Higher values of cell viability and pH were present in Ca(OH)2 than in ZnO:1.0Ca.
Figure
Reference
-
1. Bourguignon C, Cohenca N, Lauridsen E, Flores MT, O’Connell AC, Day PF, Tsilingaridis G, Abbott PV, Fouad AF, Hicks L, Andreasen JO, Cehreli ZC, Harlamb S, Kahler B, Oginni A, Semper M, Levin L. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dent Traumatol. 2020; 36:314–330. PMID: 32475015.
Article2. Lauridsen E, Hermann NV, Gerds TA, Ahrensburg SS, Kreiborg S, Andreasen JO. Combination injuries 1. The risk of pulp necrosis in permanent teeth with concussion injuries and concomitant crown fractures. Dent Traumatol. 2012; 28:364–370. PMID: 22221538.
Article3. Krastl G, Weiger R, Filippi A, Van Waes H, Ebeleseder K, Ree M, Connert T, Widbiller M, Tjäderhane L, Dummer PM, Galler K. Endodontic management of traumatized permanent teeth: a comprehensive review. Int Endod J. 2021; 54:1221–1245. PMID: 33683731.
Article4. Athanassiadis B, Walsh LJ. Aspects of solvent chemistry for calcium hydroxide medicaments. Materials (Basel). 2017; 10:1219. PMID: 29065542.
Article5. Deniz Sungur D, Aksel H, Purali N. Effect of a low surface tension vehicle on the dentinal tubule penetration of calcium hydroxide and triple antibiotic paste. J Endod. 2017; 43:452–455. PMID: 28131413.
Article6. Faria G, Rodrigues EM, Coaguila-Llerena H, Gomes-Cornélio AL, Neto Angéloco RR, Swerts Pereira MS, Tanomaru Filho M. Influence of the vehicle and antibiotic formulation on cytotoxicity of triple antibiotic paste. J Endod. 2018; 44:1812–1816. PMID: 30477667.
Article7. de Jesus Soares A, Yuri Nagata J, Casarin RC, Flávio Affonso de Almeida J, Gomes BP, Augusto Zaia A, Randi Ferraz CC, José de Souza-Filho F. Apexification with a new intra-canal medicament: a multidisciplinary case report. Iran Endod J. 2012; 7:165–170. PMID: 23056138.8. Herrera DR, Herrera CM, Lima AR, Nagata JY, Pereira AC, Silva EJ, Soares AJ, Gomes BP. Repair of apical root resorption associated with periodontitis using a new intracanal medicament protocol. J Oral Sci. 2014; 56:311–314. PMID: 25500930.
Article9. Lima TF, Ascendino JF, Cavalcante IO, D Assunção FL, Salazar-Silva JR, Silva EJ, Lemos SG, Soares AJ. Influence of chlorhexidine and zinc oxide in calcium hydroxide pastes on pH changes in external root surface. Braz Oral Res. 2019; 33:e005. PMID: 30758405.
Article10. Guerreiro-Tanomaru JM, Pereira KF, Nascimento CA, Bernardi MI, Tanomaru-Filho M. Use of nanoparticulate zinc oxide as intracanal medication in endodontics: pH and antimicrobial activity. Acta Odontol Latinoam. 2013; 26:144–148. PMID: 25335366.11. Silva AC, Zóia MA, Correia LI, Azevedo FV, Paula AT, Maia LP, Carvalho LS, Carvalho LN, Costa MP, Giaretta LC, Rodrigues RS, Ávila VM, Goulart LR, Dantas NO. Biocompatibility of doped semiconductors nanocrystals and nanocomposites. Askin Celik T, editor. Cytotoxicity. London: IntechOpen;2018. p. 149–161.12. de Souza GL, Moura CC, Silva AC, Marinho JZ, Silva TR, Dantas NO, Bonvicini JF, Turrioni AP. Effects of zinc oxide and calcium-doped zinc oxide nanocrystals on cytotoxicity and reactive oxygen species production in different cell culture models. Restor Dent Endod. 2020; 45:e54. PMID: 33294419.
Article13. Oliveira LV, de Souza GL, da Silva GR, Magalhães TE, Freitas GA, Turrioni AP, de Rezende Barbosa GL, Moura CC. Biological parameters, discolouration and radiopacity of calcium silicate-based materials in a simulated model of partial pulpotomy. Int Endod J. 2021; 54:2133–2144. Epub ahead of print. PMID: 34418112.
Article14. Pintor AV, Queiroz LD, Barcelos R, Primo LS, Maia LC, Alves GG. MTT versus other cell viability assays to evaluate the biocompatibility of root canal filling materials: a systematic review. Int Endod J. 2020; 53:1348–1373. PMID: 32602945.
Article15. Lin LM, Rosenberg PA. Repair and regeneration in endodontics. Int Endod J. 2011; 44:889–906. PMID: 21718337.
Article16. Guerreiro-Tanomaru JM, Chula DG, de Pontes Lima RK, Berbert FL, Tanomaru-Filho M. Release and diffusion of hydroxyl ion from calcium hydroxide-based medicaments. Dent Traumatol. 2012; 28:320–323. PMID: 22273011.
Article17. Samiei M, Torab A, Hosseini O, Abbasi T, Abdollahi AA, Divband B. antibacterial effect of two nano zinc oxide gel preparations compared to calcium hydroxide and chlorhexidine mixture. Iran Endod J. 2018; 13:305–311. PMID: 30083198.18. de Almeida Barbosa M, de Oliveira KV, Dos Santos VR, da Silva WJ, Tomazinho FS, Baratto-Filho F, Gabardo MC. Effect of vehicle and agitation methods on the penetration of calcium hydroxide paste in the dentinal tubules. J Endod. 2020; 46:980–986. PMID: 32439224.
Article19. Oliveira LV, da Silva GR, Souza GL, Magalhães TE, Barbosa GL, Turrioni AP, Moura CC. A laboratory evaluation of cell viability, radiopacity and tooth discoloration induced by regenerative endodontic materials. Int Endod J. 2020; 53:1140–1152. PMID: 32299123.
Article20. Souza GL, Almeida Silva AC, Dantas NO, Silveira Turrioni AP, Moura CC. Cytotoxicity and effects of a new calcium hydroxide nanoparticle material on production of reactive oxygen species by LPS-stimulated dental pulp cells. Iran Endod J. 2020; 15:227–235.21. Jeevanandam J, Chan YS, Danquah MK, Law MC. Cytotoxicity analysis of morphologically different sol-gel-synthesized MgO nanoparticles and their in vitro insulin resistance reversal ability in adipose cells. Appl Biochem Biotechnol. 2020; 190:1385–1410. PMID: 31776944.
Article22. Pan C, Hu Y, Gong Z, Yang Y, Liu S, Quan L, Yang Z, Wei Y, Ye W. Improved blood compatibility and endothelialization of titanium oxide nanotube arrays on titanium surface by zinc doping. ACS Biomater Sci Eng. 2020; 6:2072–2083. PMID: 33455341.
Article23. Vasile BŞ, Vasile OR, GhiŢulică DC, Ilie FC, Nicoară IF, Truşcă R, Oprea OC, Surdu VA, Neacşu IA. Eu3+-doped ZnO nanostructures: advanced characterizations, photoluminescence and cytotoxic effect. Rom J Morphol Embryol. 2017; 58:941–952. PMID: 29250673.24. Mishra PK, Mishra H, Ekielski A, Talegaonkar S, Vaidya B. Zinc oxide nanoparticles: a promising nanomaterial for biomedical applications. Drug Discov Today. 2017; 22:1825–1834. PMID: 28847758.
Article25. Grabrucker AM, Garner CC, Boeckers TM, Bondioli L, Ruozi B, Forni F, Vandelli MA, Tosi G. Development of novel Zn2+ loaded nanoparticles designed for cell-type targeted drug release in CNS neurons: in vitro evidences. PLoS One. 2011; 6:e17851. PMID: 21448455.
Article26. Yamamoto O. Influence of particle size on the antibacterial activity of zinc oxide. Int J Inorg Mater. 2001; 3:643–646.
Article27. Jones N, Ray B, Ranjit KT, Manna AC. Antibacterial activity of ZnO nanoparticle suspensions on a broad spectrum of microorganisms. FEMS Microbiol Lett. 2008; 279:71–76. PMID: 18081843.
Article28. Kishen A, Shi Z, Shrestha A, Neoh KG. An investigation on the antibacterial and antibiofilm efficacy of cationic nanoparticulates for root canal disinfection. J Endod. 2008; 34:1515–1520. PMID: 19026885.
Article29. International Organization for Standardization. ISO 6876: dental root canal sealing materials. Geneva: International Organization for Standardization;2012. p. 3–4.30. Villa N, Santos VV, Costa UM, Mendes AT, Duarte PH, Rosa RA, Pereira JR, Só MV. A new calcium silicate-based root canal dressing: physical and chemical properties, cytotoxicity and dentinal tubule penetration. Braz Dent J. 2020; 31:598–604. PMID: 33237230.
Article31. Shetty S, Manjunath MK, Tejaswi S. An in-vitro evaluation of the pH change through root dentin using different calcium hydroxide preparations as an intracanal medicament. J Clin Diagn Res. 2014; 8:ZC13–ZC16.32. Zancan RF, Vivan RR, Milanda Lopes MR, Weckwerth PH, de Andrade FB, Ponce JB, Duarte MA. Antimicrobial activity and physicochemical properties of calcium hydroxide pastes used as intracanal medication. J Endod. 2016; 42:1822–1828. PMID: 27776884.
Article33. Louwakul P, Saelo A, Khemaleelakul S. Efficacy of calcium oxide and calcium hydroxide nanoparticles on the elimination of Enterococcus faecalis in human root dentin. Clin Oral Investig. 2017; 21:865–871.
Article34. Fava LR, Saunders WP. Calcium hydroxide pastes: classification and clinical indications. Int Endod J. 1999; 32:257–282. PMID: 10551118.
Article35. Mohammadi Z, Dummer PM. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J. 2011; 44:697–730. PMID: 21535021.
Article36. Zand V, Mokhtari H, Hasani A, Jabbari G. Comparison of the penetration depth of conventional and nano-particle calcium hydroxide into dentinal tubules. Iran Endod J. 2017; 12:366–370. PMID: 28808467.37. Komabayashi T, D’souza RN, Dechow PC, Safavi KE, Spångberg LS. Particle size and shape of calcium hydroxide. J Endod. 2009; 35:284–287. PMID: 19166791.
Article38. Paredes RM, Etzler JC, Watts LT, Zheng W, Lechleiter JD. Chemical calcium indicators. Methods. 2008; 46:143–151. PMID: 18929663.
Article39. Xuereb M, Sorrentino F, Damidot D, Camilleri J. Development of novel tricalcium silicate-based endodontic cements with sintered radiopacifier phase. Clin Oral Investig. 2016; 20:967–982.
Article40. Ordinola-Zapata R, Bramante CM, García-Godoy F, Moldauer BI, Gagliardi Minotti P, Tercília Grizzo L, Duarte MA. The effect of radiopacifiers agents on pH, calcium release, radiopacity, and antimicrobial properties of different calcium hydroxide dressings. Microsc Res Tech. 2015; 78:620–625. PMID: 25990864.41. Pelepenko LE, Saavedra F, Bombarda GF, Gomes BP, DE-Jesus-Soares A, Zaia AA, Duarte MA, Tanomaru-Filho M, Marciano MA. Dental discoloration caused by Grey-MTAFlow cement: analysis of its physicochemical, biological and antimicrobial properties. J Appl Oral Sci. 2020; 28:e20200269. PMID: 32785521.
Article42. Galvão T, Camargo B, Armada L, Alves F. Efficacy of three methods for inserting calcium hydroxide-based paste in root canals. J Clin Exp Dent. 2017; 9:e762–e766. PMID: 28638552.
Article43. Zare S, Shen I, Zhu Q, Ahn C, Primus C, Komabayashi T. Micro-computed tomographic evaluation of single-cone obturation with three sealers. Restor Dent Endod. 2021; 46:e25. PMID: 34123761.
Article44. Bhandi S, Mashyakhy M, Abumelha AS, Alkahtany MF, Jamal M, Chohan H, Raj AT, Testarelli L, Reda R, Patil S. Complete obturation-cold lateral condensation vs. thermoplastic techniques: a systematic review of micro-CT studies. Materials (Basel). 2021; 14:4013. PMID: 34300930.
Article45. Donnermeyer D, Wyrsch H, Bürklein S, Schäfer E. Removal of calcium hydroxide from artificial grooves in straight root canals: sonic activation using EDDY versus passive ultrasonic irrigation and XP endo Finisher. J Endod. 2019; 45:322–326. PMID: 30803540.
Article46. De Faria-Júnior NB, Keine KC, Só MV, Weckwerth PH, Guerreiro-Tanomaru JM, Kuga MC. Residues of calcium hydroxide-based intracanal medication associated with different vehicles: a scanning electron microscopy evaluation. Microsc Res Tech. 2012; 75:898–902. PMID: 22279037.
Article47. Balvedi RP, Versiani MA, Manna FF, Biffi JC. A comparison of two techniques for the removal of calcium hydroxide from root canals. Int Endod J. 2010; 43:763–768. PMID: 20546045.
Article48. da Silva JM, Andrade Junior CV, Zaia AA, Pessoa OF. Microscopic cleanliness evaluation of the apical root canal after using calcium hydroxide mixed with chlorhexidine, propylene glycol, or antibiotic paste. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 111:260–264. PMID: 21168349.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial effect of calcium hydroxide as an intracanal medicament in root canal treatment: a literature review - Part I. In vitro studies
- Antimicrobial effect of calcium hydroxide as an intracanal medicament in root canal treatment: a literature review - Part II. in vivo studies
- Incidence of interappointment emergencies in multiple-visit root canal treatments performed with or without intracanal medicament by undergraduate students
- Effects of zinc oxide and calcium–doped zinc oxide nanocrystals on cytotoxicity and reactive oxygen species production in different cell culture models
- Effect of Intracanal Medicaments on Push-out Bond Strength of Calcium Silicate-based Materials