Restor Dent Endod.
2022 Nov;47(4):e36. 10.5395/rde.2022.47.e36.
Correlation between different methodologies used to evaluate the marginal adaptation of proximal dentin gingival margins elevated using a glass hybrid
- Affiliations
-
- 1Department of Operative Dentistry Faculty of Dentistry, Mansoura University, Mansoura, Egypt
- 2Department of Bioscience Research, College of Dentistry, University of Tennessee Health Science Center, Memphis, TN, USA
- 3Adjunct Faculty, The Forsyth Institute, Cambridge, MA, USA
- KMID: 2548140
- DOI: http://doi.org/10.5395/rde.2022.47.e36
Abstract
Objectives
This study aimed to evaluate the effect of aging on the marginal quality of glass hybrid (GH) material used to elevate dentin gingival margins, and to analyze the consistency of the results obtained by 3 in vitro methods.
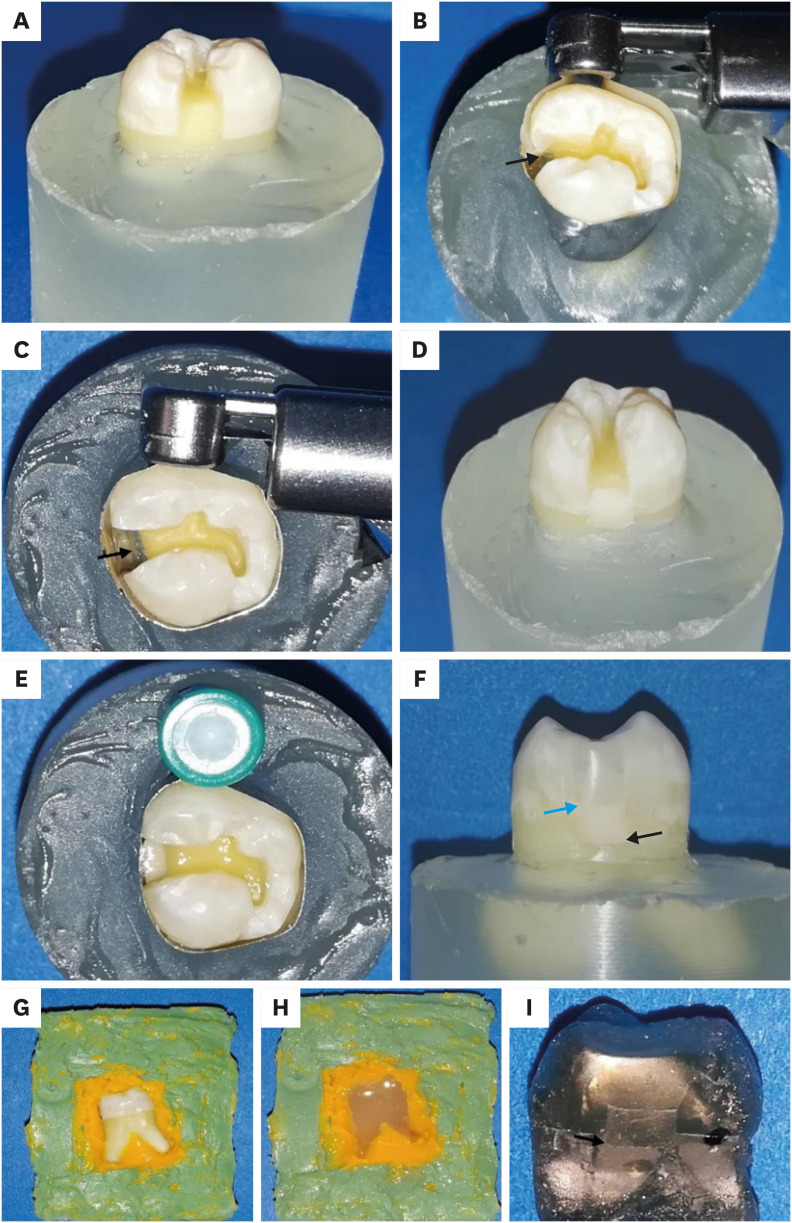
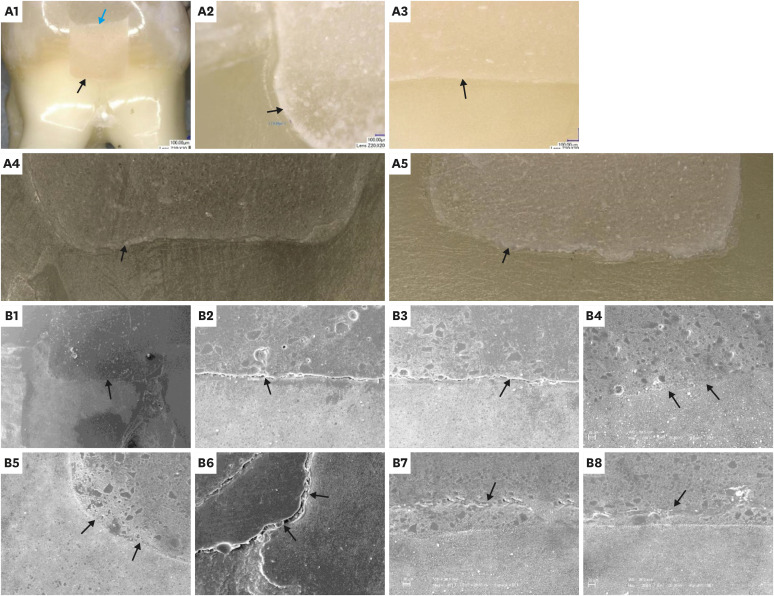
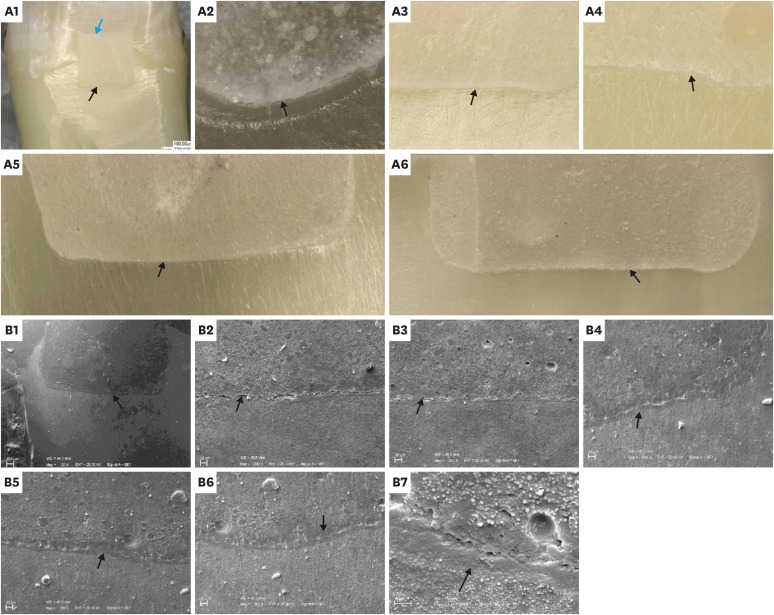
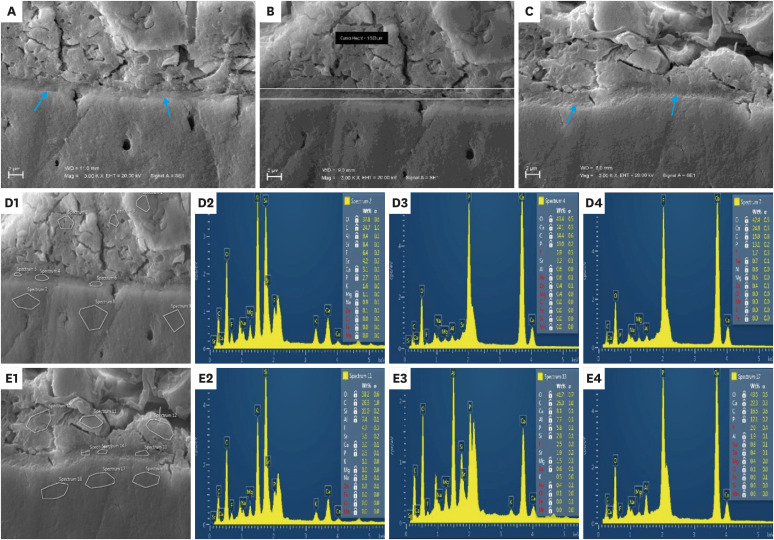
Materials and Methods
Ten teeth received compound class II cavities with subgingival margins. The dentin gingival margins were elevated with GH, followed by resin composite. The GH/gingival dentin interfaces were examined through digital microscopy, scanning electron microscopy (SEM) using resin replicas, and according to the World Dental Federation (FDI) criteria. After initial evaluations, all teeth were subjected to 10,000 thermal cycles, followed by repeating the same marginal evaluations and energy dispersive spectroscopy (EDS) analysis for the interfacial zone of 2 specimens. Marginal quality was expressed as the percentage of continuous margin at ×200 for microscopic techniques and as the frequency of each score for FDI ranking. Data were analyzed using the paired sample t-test, Wilcoxon signed-rank test, and Pearson and Spearmen correlation coefficients.
Results
None of the testing techniques proved the significance of the aging factor. Moderate and strong significant correlations were found between the testing techniques. The EDS results suggested the presence of an ion-exchange layer along the GH/gingival dentin interface of aged specimens.
Conclusions
The marginal quality of the GH/dentin gingival interface defied aging by thermocycling. The replica SEM and FDI ranking results had stronger correlations with each other than either showed with the digital microscopy results.
Keyword
Figure
Reference
-
1. Zhou X, Huang X, Li M, Peng X, Wang S, Zhou X, Cheng L. Development and status of resin composite as dental restorative materials. J Appl Polym Sci. 2019; 136:48180.
Article2. Kielbassa AM, Philipp F. Restoring proximal cavities of molars using the proximal box elevation technique: Systematic review and report of a case. Quintessence Int. 2015; 46:751–764. PMID: 26159213.3. Veneziani M. Adhesive restorations in the posterior area with subgingival cervical margins: new classification and differentiated treatment approach. Eur J Esthet Dent. 2010; 5:50–76. PMID: 20305873.4. Al-Harbi F, Kaisarly D, Michna A, ArRejaie A, Bader D, El Gezawi M. Cervical interfacial bonding effectiveness of Class II bulk versus incremental fill resin composite restorations. Oper Dent. 2015; 40:622–635. PMID: 26151459.
Article5. Manuja N, Nagpal R, Pandit IK. Dental adhesion: mechanism, techniques and durability. J Clin Pediatr Dent. 2012; 36:223–234. PMID: 22838222.6. Juloski J, Köken S, Ferrari M. Cervical margin relocation in indirect adhesive restorations: a literature review. J Prosthodont Res. 2018; 62:273–280. PMID: 29153552.
Article7. Lindberg A, van Dijken JW, Lindberg M. 3-year evaluation of a new open sandwich technique in Class II cavities. Am J Dent. 2003; 16:33–36. PMID: 12744410.8. Dietschi D, Spreafico R. Current clinical concepts for adhesive cementation of tooth-colored posterior restorations. Pract Periodontics Aesthet Dent. 1998; 10:47–54. PMID: 9582662.9. Ilgenstein I, Zitzmann NU, Bühler J, Wegehaupt FJ, Attin T, Weiger R, Krastl G. Influence of proximal box elevation on the marginal quality and fracture behavior of root-filled molars restored with CAD/CAM ceramic or composite onlays. Clin Oral Investig. 2015; 19:1021–1028.
Article10. Vertolli TJ, Martinsen BD, Hanson CM, Howard RS, Kooistra S, Ye L. Effect of deep margin elevation on CAD/CAM-fabricated ceramic inlays. Oper Dent. 2020; 45:608–617. PMID: 32243253.
Article11. Grubbs TD, Vargas M, Kolker J, Teixeira EC. Efficacy of direct restorative materials in proximal box elevation on the margin quality and fracture resistance of molars restored with CAD/CAM onlays. Oper Dent. 2020; 45:52–61. PMID: 31084532.
Article12. Miletić I, Baraba A, Basso M, Pulcini MG, Marković D, Perić T, Ozkaya CA, Turkun LS. Clinical performance of a glass-hybrid system compared with a resin composite in the posterior region: Results of a 2-year multicenter study. J Adhes Dent. 2020; 22:235–247. PMID: 32435764.13. Moshaverinia M, Navas A, Jahedmanesh N, Shah KC, Moshaverinia A, Ansari S. Comparative evaluation of the physical properties of a reinforced glass ionomer dental restorative material. J Prosthet Dent. 2019; 122:154–159. PMID: 31326149.
Article14. Mahmoud SH, Al-Wakeel ES. Marginal adaptation of ormocer-, silorane-, and methacrylate-based composite restorative systems bonded to dentin cavities after water storage. Quintessence Int. 2011; 42:e131–e139. PMID: 22026005.15. Al-Harbi F, Kaisarly D, Bader D, El Gezawi M. Marginal integrity of bulk versus incremental fill Class II composite restorations. Oper Dent. 2016; 41:146–156. PMID: 26266653.
Article16. Aggarwal V, Bhasin SS. Application of calcium silicate materials after acid etching may preserve resin-dentin bonds. Oper Dent. 2018; 43:E243–E252. PMID: 29953337.
Article17. Heintze SD. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007; 9(Supplement 1):77–106. PMID: 18341236.18. Heintze SD. Clinical relevance of tests on bond strength, microleakage and marginal adaptation. Dent Mater. 2013; 29:59–84. PMID: 22920539.
Article19. Han SH, Park SH. Incremental and bulk-fill techniques with bulk-fill resin composite in different cavity configurations. Oper Dent. 2018; 43:631–641. PMID: 29630486.
Article20. Irie M, Suzuki K, Watts DC. Delayed polishing technique on glass–ionomer restorations. Jpn Dent Sci Rev. 2009; 45:14–22.
Article21. KEYENCE. VHX-1000 series digital microscope data sheet [Internet]. cited December 20, 2021. Available from: https://www.keyence.com/products/microscope/digital-microscope/vhx-1000/models/vhx-1000e/ .22. Aggarwal V, Singla M, Yadav S, Yadav H. Effect of flowable composite liner and glass ionomer liner on class II gingival marginal adaptation of direct composite restorations with different bonding strategies. J Dent. 2014; 42:619–625. PMID: 24631232.
Article23. Hickel R, Peschke A, Tyas M, Mjör I, Bayne S, Peters M, Hiller KA, Randall R, Vanherle G, Heintze SD. FDI World Dental Federation: clinical criteria for the evaluation of direct and indirect restorations-update and clinical examples. Clin Oral Investig. 2010; 14:349–366.
Article24. Cvar JF, Ryge G. Reprint of criteria for the clinical evaluation of dental restorative materials. 1971. Clin Oral Investig. 2005; 9:215–232.25. Ernst CP, Canbek K, Euler T, Willershausen B. In vivo validation of the historical in vitro thermocycling temperature range for dental materials testing. Clin Oral Investig. 2004; 8:130–138.26. Boussès Y, Brulat-Bouchard N, Tillier Y. Effects of ageing on glass-polymer dental composites. Comput Methods Biomech Biomed Engin. 2020; 23(Supplement 1):S47–S48.
Article27. Francois P, Vennat E, Le Goff S, Ruscassier N, Attal JP, Dursun E. Shear bond strength and interface analysis between a resin composite and a recent high-viscous glass ionomer cement bonded with various adhesive systems. Clin Oral Investig. 2019; 23:2599–2608.
Article28. Kandaswamy D, Rajan KJ, Venkateshbabu N, Porkodi I. Shear bond strength evaluation of resin composite bonded to glass-ionomer cement using self-etching bonding agents with different pH: In vitro study. J Conserv Dent. 2012; 15:27–31. PMID: 22368331.
Article29. Alqudaihi FS, Cook NB, Diefenderfer KE, Bottino MC, Platt JA. Comparison of internal adaptation of bulk-fill and increment-fill resin composite materials. Oper Dent. 2019; 44:E32–E44. PMID: 29856698.
Article30. Cavalcanti AN, Mitsui FH, Lima AF, Mathias P, Marchi GM. Evaluation of dentin hardness and bond strength at different walls of class II preparations. J Adhes Dent. 2010; 12:183–188. PMID: 20157677.31. Münevveroğlu AP, Ozsoy A, Ozcan M. Microleakage of high viscosity glass-ionomer and glass-carbomer with and without coating before and after hydrothermal aging. Braz Dent Sci. 2019; 22:79–87.
Article32. Aydın N, Karaoğlanoğlu S, Aybala-Oktay E, Çetinkaya S, Erdem O. Investigation of water sorption and aluminum releases from high viscosity and resin modified glass ionomer. J Clin Exp Dent. 2020; 12:e844–e851. PMID: 32994873.33. Troca VB, Fernandes KB, Terrile AE, Marcucci MC, Andrade FB, Wang L. Effect of green propolis addition to physical mechanical properties of glass ionomer cements. J Appl Oral Sci. 2011; 19:100–105. PMID: 21552709.
Article34. Pinto-Sinai G, Brewster J, Roberts H. Linear coefficient of thermal expansion evaluation of glass ionomer and resin-modified glass ionomer restorative materials. Oper Dent. 2018; 43:E266–E272. PMID: 29953342.
Article35. de Oliveira BM, Agostini IE, Baesso ML, Menezes-Silva R, Borges AF, Navarro MF, Nicholson JW, Sidhu SK, Pascotto RC. Influence of external energy sources on the dynamic setting process of glass-ionomer cements. Dent Mater. 2019; 35:450–456. PMID: 30709613.
Article36. Nicholson JW. Glass ionomer dental cements: update. Mater Technol. 2010; 25:8–13.
Article37. Sidhu SK, Nicholson JW. A review of glass-ionomer cements for clinical dentistry. J Funct Biomater. 2016; 7:16. PMID: 27367737.
Article38. Ngo H, Mount GJ, Peters MC. A study of glass-ionomer cement and its interface with enamel and dentin using a low-temperature, high-resolution scanning electron microscopic technique. Quintessence Int. 1997; 28:63–69. PMID: 10332357.39. Nicholson JW. Maturation processes in glass-ionomer dental cements. Acta Biomater Odontol Scand. 2018; 4:63–71. PMID: 30083577.
Article40. Buldur M, Sirin Karaarslan E. Microhardness of glass carbomer and high-viscous glass Ionomer cement in different thickness and thermo-light curing durations after thermocycling aging. BMC Oral Health. 2019; 19:273. PMID: 31801493.
Article41. Karadas M, Atıcı MG. Bond strength and adaptation of pulp capping materials to dentin. Microsc Res Tech. 2020; 83:514–522. PMID: 31912929.
Article42. Hoshika S, Ting S, Ahmed Z, Chen F, Toida Y, Sakaguchi N, Van Meerbeek B, Sano H, Sidhu SK. Effect of conditioning and 1\\xe2\\x80\\xafyear aging on the bond strength and interfacial morphology of glass-ionomer cement bonded to dentin. Dent Mater. 2021; 37:106–112. PMID: 33229039.
Article43. Garcia-Godoy F, Krämer N, Feilzer AJ, Frankenberger R. Long-term degradation of enamel and dentin bonds: 6-year results in vitro vs. in vivo. Dent Mater. 2010; 26:1113–1118. PMID: 20800270.
Article44. Bertoldi C, Monari E, Cortellini P, Generali L, Lucchi A, Spinato S, Zaffe D. Clinical and histological reaction of periodontal tissues to subgingival resin composite restorations. Clin Oral Investig. 2020; 24:1001–1011.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deep proximal margin rebuilding with direct esthetic restorations: a systematic review of marginal adaptation and bond strength
- Microleakage and marginal hybrid layer of dentin adhesives
- Effect of biscover on the marginal microleakage of composite resin restoration
- Marginal microleakage of single step adhesives
- COMPARISON OF SHEAR BOND STRENGTH AND MARGINAL LEAKAGE OF RESIN MODIFIED GLASS IONOMER CEMENTS