Obstet Gynecol Sci.
2023 Nov;66(6):545-561. 10.5468/ogs.23208.
Incidence and survival of gynecologic cancer including cervical, uterine, ovarian, vaginal, vulvar cancer and gestational trophoblastic neoplasia in Korea, 1999-2019: Korea Central Cancer Registry
- Affiliations
-
- 1Department of Obstetrics and Gynecology, CHA Ilsan Medical Center, CHA University School of Medicine, Goyang, Korea
- 2Korea Central Cancer Registry, National Cancer Center, Goyang, Korea
- 3Division of Cancer Registration and Surveillance, National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 4Department of Obstetrics and Gynecology, Institute of Women’s Life Medical Science, Yonsei University College of Medicine, Seoul, Korea
- 5Department of Obstetrics and Gynecology, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
- 6Department of Obstetrics and Gynecology, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul, Korea
- 7Department of Obstetrics and Gynecology,, National Rehabilitation Center, Ministry of Health and Welfare, Seoul, Korea
- 8Department of Obstetrics and Gynecology, Ewha Woman’s University College of Medicine, Seoul, Korea
- KMID: 2547856
- DOI: http://doi.org/10.5468/ogs.23208
Abstract
Objective
To investigate the incidence, trends, and survival rates of all gynecologic cancers using the Korea Central Cancer Registry (KCCR) database from 1999-2019.
Methods
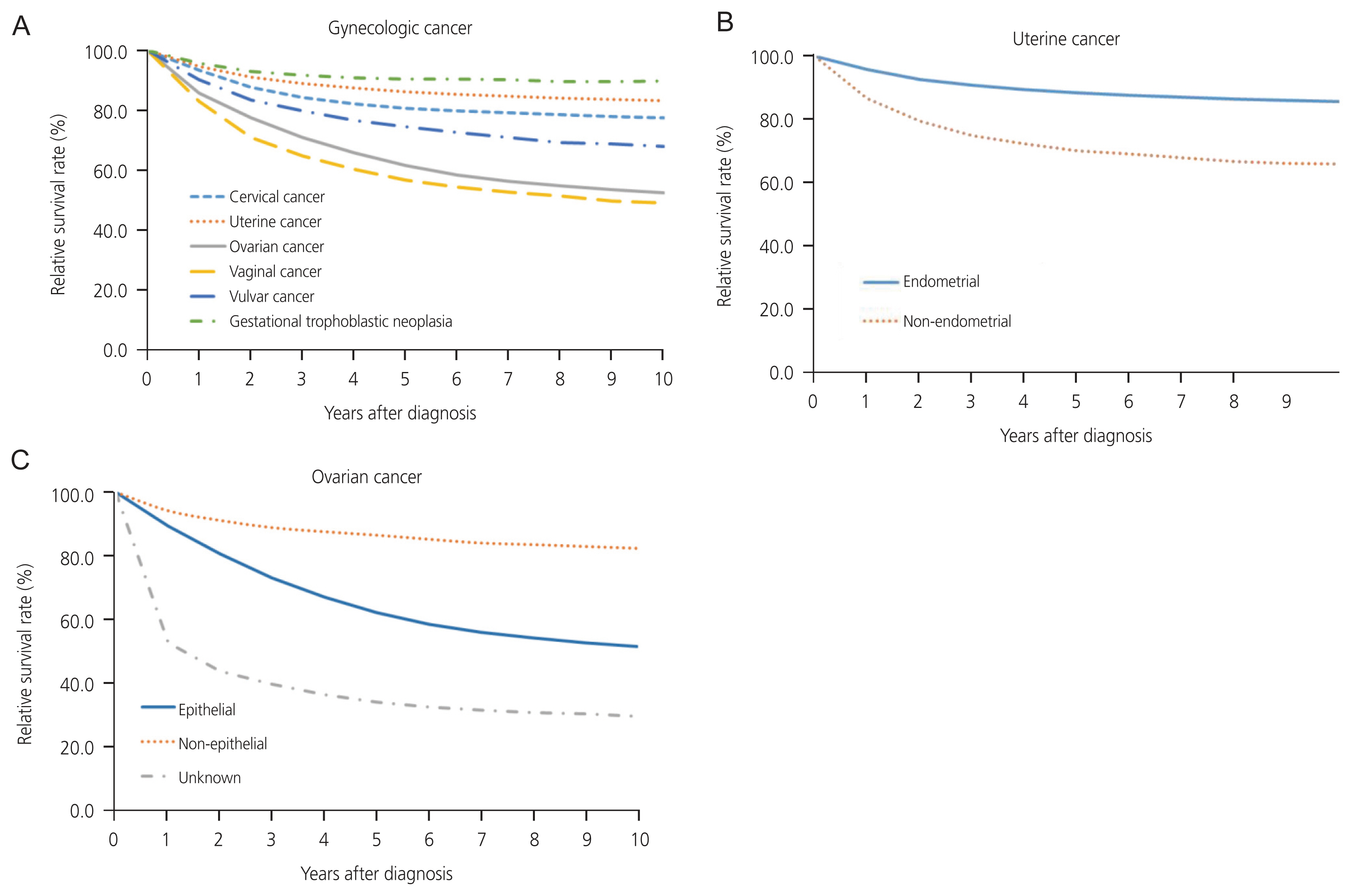
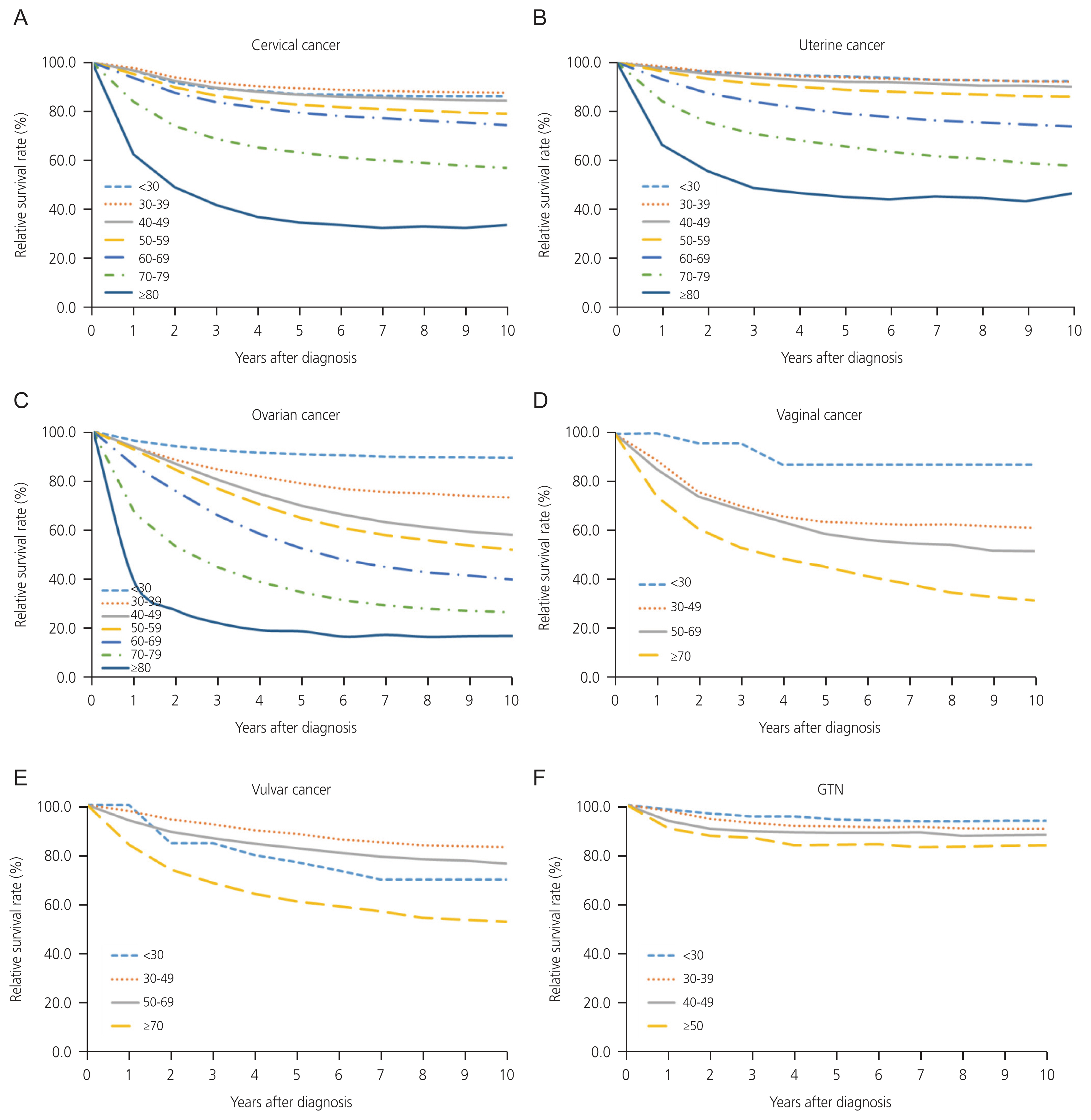
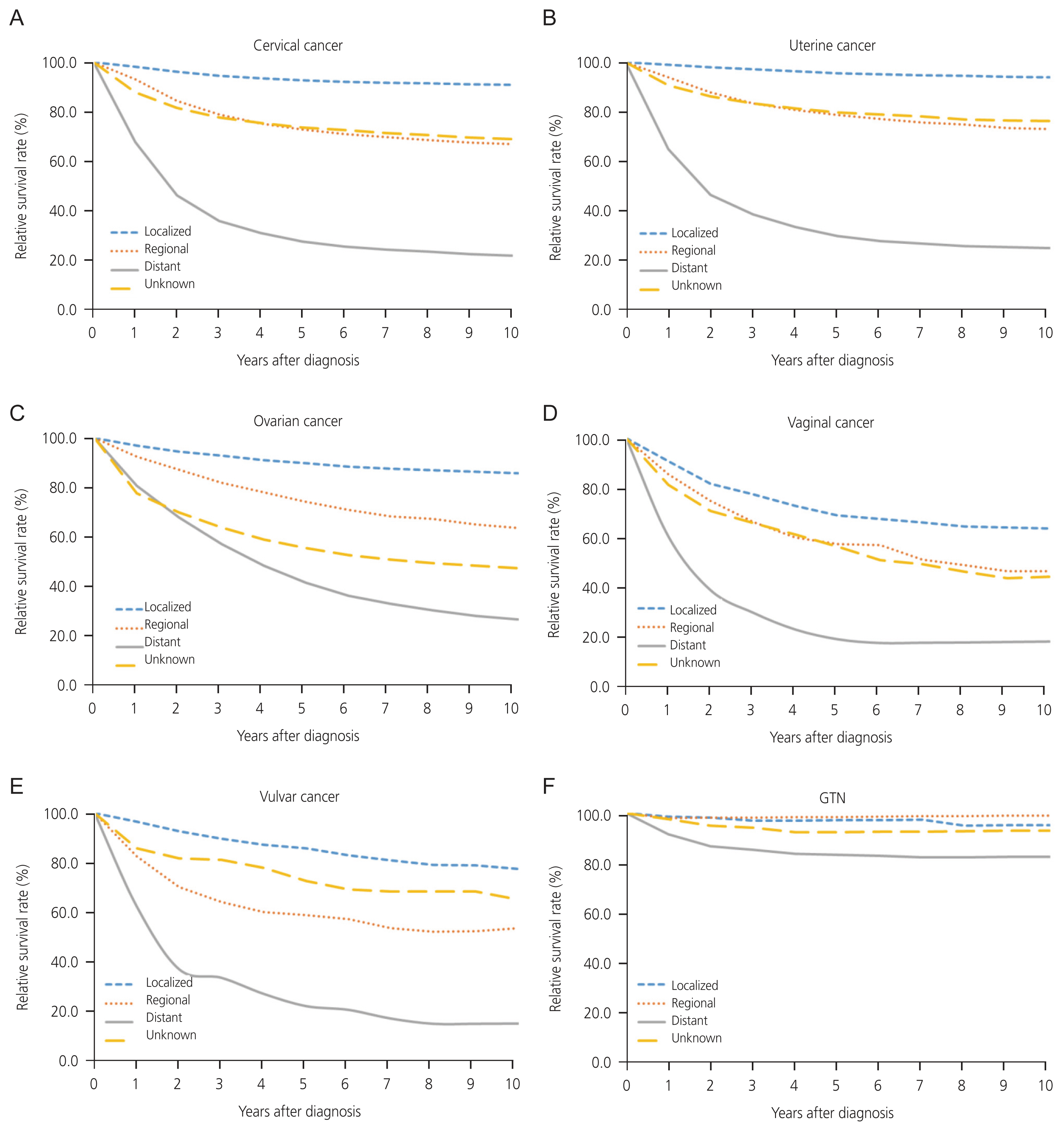
Gynecologic cancer data were obtained from the KCCR database between 1999 and 2019. Age-standardized incidence rates (ASRs), annual percentage changes, and average annual percentage changes (AAPCs) were calculated. The relative survival rate (RSR) was reported by age group, stage, and 6-year period (I: 1999-2005, II: 2006-2012, III: 2013- 2019).
Results
The gynecologic cancer ASRs were 26.2 and 24.9 per 100,000 individuals in 1999 and 2019, respectively. Trends of incidence in gynecologic cancer revealed a decrease in cervical cancer and gestational trophoblastic neoplasia (GTN) with AAPCs of -3.4 and -4.3, respectively. Conversely, the incidence of uterine, ovarian, and vulvar cancers increased with AAPCs of 4.7, 2.3, and 2.1, respectively. AAPC for vaginal cancer showed no change. The 5-year survival rate was highest for GTN (90.5%) and lowest for vaginal cancer (56.6%). An increase in age was correlated with poorer survival rates across all gynecologic cancers, excluding vaginal cancer. For all gynecologic cancer types, the prognosis deteriorates with advancing cancer stages. The RSR of uterine cancer improved consistently across all periods. The ovarian cancer RSR improved more in period III than in periods I or II. Additionally, the vulvar cancer RSR improved more in periods II and III than in period I.
Conclusion
In Korea, the incidence of cervical cancer and GTN decreased, whereas the incidence of uterine, ovarian, and vulvar cancer increased from 1999 to 2019. The RSR for uterine, ovarian, and vulvar cancers showed consistent improvements over different periods. Effective screening programs and the adoption of advanced treatments may be necessary to further reduce the burden of gynecologic cancer.
Figure
Cited by 2 articles
-
Cervical cancer in Thailand: 2023 update
Mayuree Wongpratate, Sureewan Bumrungthai
Obstet Gynecol Sci. 2024;67(3):261-269. doi: 10.5468/ogs.23277.Basic knowledge for counseling patients undergoing risk-reducing salpingo-oophorectomy
Jihye Kim, Chel Hun Choi
Obstet Gynecol Sci. 2024;67(4):343-355. doi: 10.5468/ogs.24054.
Reference
-
References
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–49.
Article2. Statistics Korea. Annual report on the causes of death statistics [Internet]. Daejeon: Statistics Korea;c2020. [cited 2022 Feb 13]. Available from: https://kosis.kr/index/index.do.3. Kang MJ, Jung KW, Bang SH, Choi SH, Park EH, Yun EH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2020. Cancer Res Treat. 2023; 55:385–99.
Article4. Lim MC, Won YJ, Ko MJ, Kim M, Shim SH, Suh DH, et al. Incidence of cervical, endometrial, and ovarian cancer in Korea during 1999–2015. J Gynecol Oncol. 2019; 30:e38.
Article5. Ha HI, Chang HK, Park SJ, Lim J, Won YJ, Lim MC. The incidence and survival of cervical, ovarian, and endometrial cancer in Korea, 1999–2017: Korea Central Cancer Registry. Obstet Gynecol Sci. 2021; 64:444–53.
Article6. Shin W, Won YJ, Yoo CW, Lim J, Lim MC. Incidence trends for epithelial peritoneal, ovarian, and fallopian tube cancer during 1999–2016: a retrospective study based on the Korean National Cancer Incidence database. J Gynecol Oncol. 2020; 31:e56.
Article7. Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, et al. International classification of diseases for oncology. 3rd ed. Geneva: World Health Organization;2013.8. Young JL Jr, Roffers SD, Ries LA, Fritz AG, Hurlbut AA. SEER summary staging manual 2000: codes and coding instructions. 1st ed. Bethesda (MD): National Cancer Institute;2001. p. 4969.9. World Health Organization. ICD-10: international statistical classification of diseases and related health problems [Internet]. Geneva: World Health Organization;c2010. [cited 2012 Mar 23]. Available from: https://icd.who.int/browse10/2010/en.10. Matz M, Coleman MP, Sant M, Chirlaque MD, Visser O, Gore M, et al. The histology of ovarian cancer: worldwide distribution and implications for international survival comparisons (CONCORD-2). Gynecol Oncol. 2017; 144:405–13.11. Segi M, Fujisaku S. Cancer mortality for selected sites in 24 countries 1950–1957. 1st ed. Sendai: Tohoku University School of Medicine;1960.12. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000; 19:335–51.
Article13. Ederer F, Heise H. Instructions to IBM 650 programmers in processing survival computations. 10th ed. Bethesda (MD): National Cancer Institute;1959.14. Dickman Paul. Strs - estimating and modelling relative/net survival [Internet]. Stockholm: Paul Dickman;2016. [cited 2023 Feb 6]. Available from: https://www.pauldickman.com/software/strs/#introduction-and-features.15. Shim SH, Kim H, Sohn IS, Hwang HS, Kwon HS, Lee SJ, et al. Nationwide cervical cancer screening in Korea: data from the National Health Insurance Service Cancer Screening Program and National Cancer Screening Program, 2009–2014. J Gynecol Oncol. 2017; 28:e63.
Article16. Kim YT. Current status of cervical cancer and HPV infection in Korea. J Gynecol Oncol. 2009; 20:1–7.
Article17. Oh CM, Jung KW, Won YJ, Shin A, Kong HJ, Jun JK, et al. Trends in the incidence of in situ and invasive cervical cancer by age group and histological type in Korea from 1993 to 2009. PLoS One. 2013; 8:e72012.
Article18. Gravdal BH, Lönnberg S, Skare GB, Sulo G, Bjørge T. Cervical cancer in women under 30 years of age in Norway: a population-based cohort study. BMC Womens Health. 2021; 21:110.19. Castanon A, Leung VM, Landy R, Lim AW, Sasieni P. Characteristics and screening history of women diagnosed with cervical cancer aged 20–29 years. Br J Cancer. 2013; 109:35–41.
Article20. Raglan O, Kalliala I, Markozannes G, Cividini S, Gunter MJ, Nautiyal J, et al. Risk factors for endometrial cancer: an umbrella review of the literature. Int J Cancer. 2019; 145:1719–30.
Article21. Jo H, Kim SI, Wang W, Seol A, Han Y, Kim J, et al. Metabolic syndrome as a risk factor of endometrial cancer: a nationwide population-based cohort study of 2.8 million women in South Korea. Front Oncol. 2022; 12:872995.
Article22. Kim JH, Lim JS. Prevalence trends of metabolic syndrome among Korean children and adolescents from a population-based cross-sectional survey. Life (Basel). 2022; 12:1404.
Article23. Statistics Korea. Birth statistics in 2022 [Internet]. Daejeon: Statistics Korea;c2023. [2023 Aug 30]. Available from: https://kostat.go.kr/board.es?mid=a20108100000&bid=11773.24. Kato H. Total fertility rate, economic-social conditions, and public policies in OECD countries. Kato H, editor. Macro-econometric analysis on determinants of fertility behavior. New York: Springer;2021. p. 51–76.
Article25. Chang SJ, Kim WY, Yoon JH, Yoo SC, Chang KH, Ryu HS. Para-aortic lymphadenectomy improves survival in patients with intermediate to high-risk endometrial carcinoma. Acta Obstet Gynecol Scand. 2008; 87:1361–9.
Article26. Gordhandas S, Zammarrelli WA, Rios-Doria EV, Green AK, Makker V. Current evidence-based systemic therapy for advanced and recurrent endometrial cancer. J Natl Compr Canc Netw. 2023; 21:217–26.
Article27. de Boer SM, Powell ME, Mileshkin L, Katsaros D, Bessette P, Haie-Meder C, et al. Adjuvant chemoradiotherapy versus radiotherapy alone for women with high-risk endometrial cancer (PORTEC-3): final results of an international, open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2018; 19:295–309.28. Yagi A, Ueda Y, Ikeda S, Miyoshi A, Nakagawa S, Hiramatsu K, et al. Improved long-term survival of corpus cancer in Japan: a 40-year population-based analysis. Int J Cancer. 2022; 150:232–42.
Article29. Park M, Lim J, Lee JA, Park HJ, Park BK, Lim MC, et al. Incidence and outcomes of malignant ovarian germ cell tumors in Korea, 1999–2017. Gynecol Oncol. 2021; 163:79–84.
Article30. Doubeni CA, Doubeni AR, Myers AE. Diagnosis and management of ovarian cancer. Am Fam Physician. 2016; 93:937–44.31. Chang SJ, Bristow RE, Ryu HS. Impact of complete cytoreduction leaving no gross residual disease associated with radical cytoreductive surgical procedures on survival in advanced ovarian cancer. Ann Surg Oncol. 2012; 19:4059–67.
Article32. Perren TJ, Swart AM, Pfisterer J, Ledermann JA, Pujade-Lauraine E, Kristensen G, et al. A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med. 2011; 365:2484–96.
Article33. Moore K, Colombo N, Scambia G, Kim BG, Oaknin A, Friedlander M, et al. Maintenance olaparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med. 2018; 379:2495–505.
Article34. Chen W, Xia C, Zheng R, Zhou M, Lin C, Zeng H, et al. Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: a comparative risk assessment. Lancet Glob Health. 2019; 7:e257–69.
Article35. Lai J, Elleray R, Nordin A, Hirschowitz L, Rous B, Gildea C, et al. Vulval cancer incidence, mortality and survival in England: age-related trends. BJOG. 2014; 121:728–38. discussion 739.
Article36. Meltzer-Gunnes CJ, Småstuen MC, Kristensen GB, Tropé CG, Lie AK, Vistad I. Vulvar carcinoma in Norway: a 50-year perspective on trends in incidence, treatment and survival. Gynecol Oncol. 2017; 145:543–8.
Article37. Trétarre B, Dantony E, Coureau G, Defossez G, Guizard AV, Delafosse P, et al. Trends in incidence of invasive vaginal cancer in France from 1990 to 2018 and survival of recently diagnosed women - a population-based study. Eur J Obstet Gynecol Reprod Biol. 2023; 283:125–9.
Article38. Gadducci A, Cosio S, Fanucchi A, Tana R, Manacorda S, Pistolesi S, et al. Prognosis of patients with gestational trophoblastic neoplasia and obstetric outcomes of those conceiving after chemotherapy. Anticancer Res. 2016; 36:3477–82.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The role of positron emission tomography in the diagnosis and management of gynecologic malignancies
- Incidence of cervical, endometrial, and ovarian cancer in Korea, 1999-2010
- The incidence and survival of cervical, ovarian, and endometrial cancer in Korea, 1999-2017: Korea Central Cancer Registry
- Annual report of gynecologic cancer registry program in Korea: 1991~2004
- The Changing Trends of the Incidence and Histopathology of the Female Genital Malignancies in Keimyung University Dongsan Medical Center Between 1975 and 1994