Obstet Gynecol Sci.
2023 Nov;66(6):529-536. 10.5468/ogs.23108.
Fetal growth changes and prediction of selective fetal growth restriction following fetoscopic laser coagulation in twin-to-twin transfusion syndrome
- Affiliations
-
- 1Department of Obstetrics and Gynecology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Asan Medical Center, Seoul, Korea
- KMID: 2547854
- DOI: http://doi.org/10.5468/ogs.23108
Abstract
Objective
To investigate fetal growth changes and predictive factors for selective fetal growth restriction (sFGR) in patients with twin-to-twin transfusion syndrome (TTTS) after fetoscopic laser coagulation (FLC).
Methods
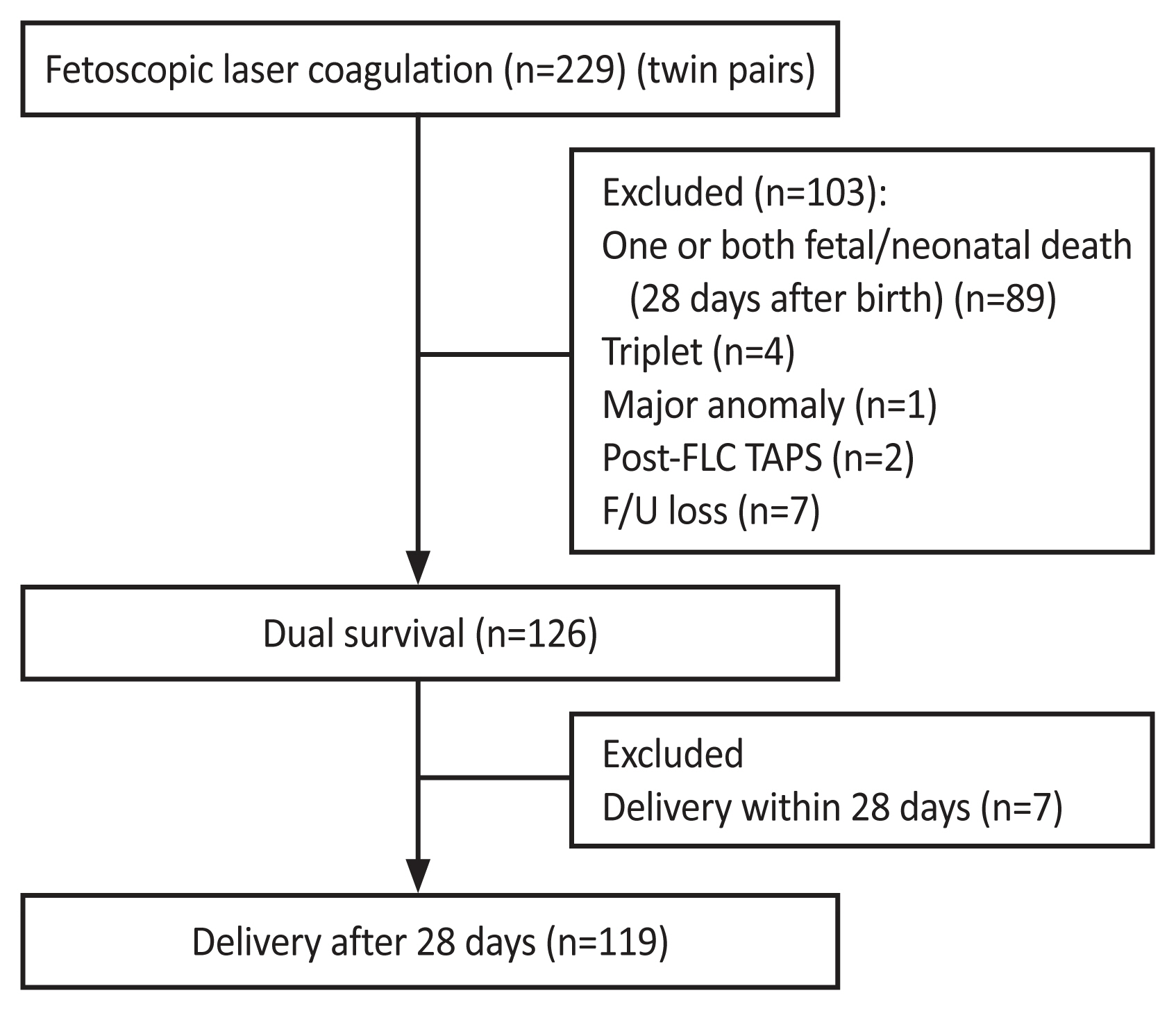
This retrospective study included twin-pregnant women with fetal TTTS who underwent FLC at our institution between 2011 and 2020. Twin pairs who survived at least 28 days after FLC and at least 28 days after birth were included. A paired t-test was used to compare the mean discordance between the estimated fetal weights at the FLC and the birth weights. The predictive factors for sFGR after FLC were evaluated using univariate and multivariate logistic regression analyses.
Results
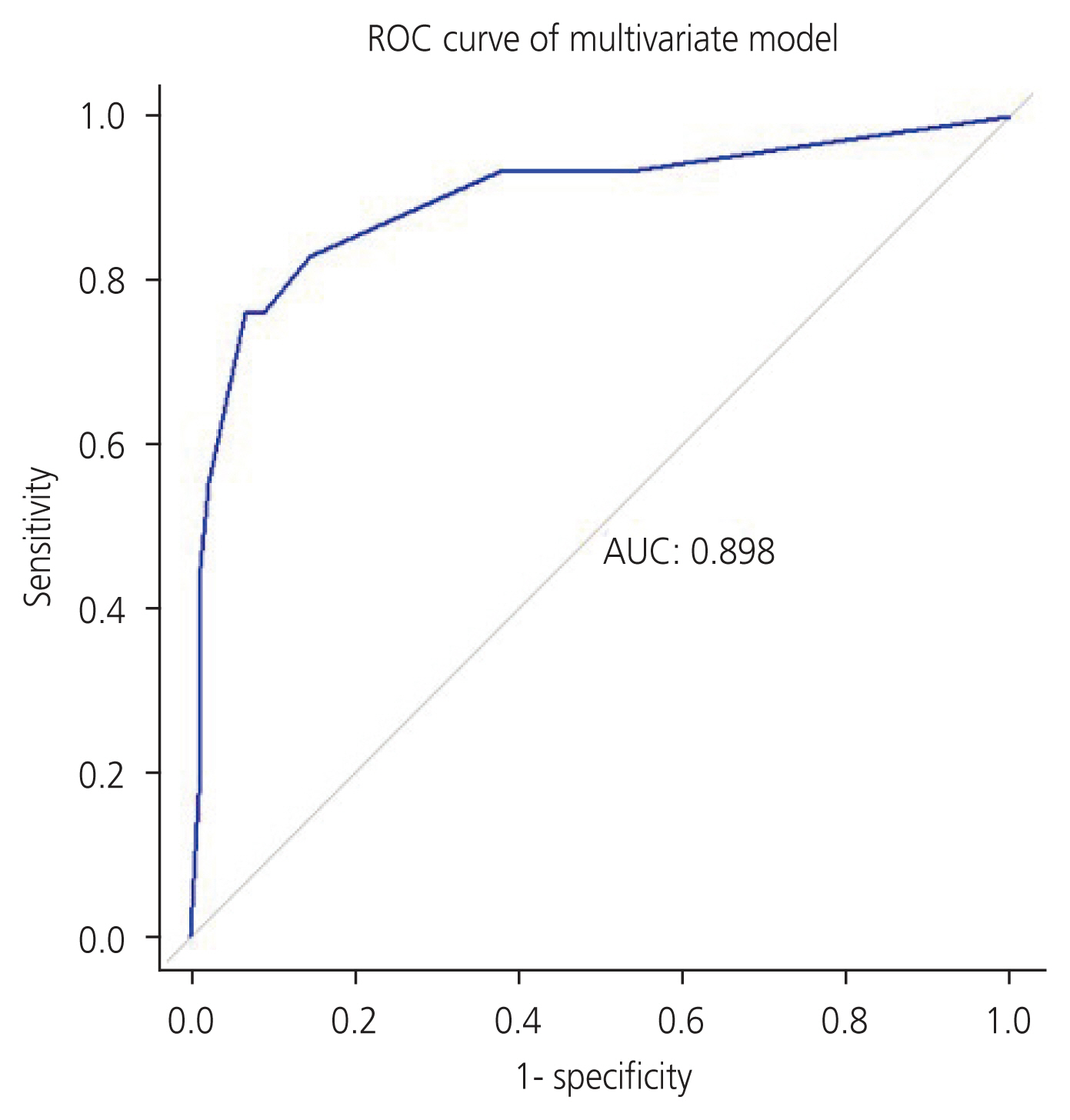
A total of 119 eligible pairs of patients who underwent FLC were analyzed. The weight percentile at birth significantly decreased after FLC in the recipients (53.7±30.4 percentile vs. 43.7±28.0 percentile; P<0.001), but increased in the donors (11.5±17.1 percentile vs. 20.7±22.8 percentile; P<0.001). Additionally, the mean weight discordance of twin pairs significantly decreased after FLC (23.9%±12.7% vs. 17.3%±15.7%; P<0.001). After FLC, Quintero stage ≥3, pre-FLC sFGR, abnormal cord insertion, and post-FLC abnormal umbilical artery Doppler (UAD) were all significantly higher in the sFGR group than the non-sFGR group. The prediction model using these variables indicated that the area under the receiver operating characteristic curve was 0.898.
Conclusion
The recipient weight percentile decreased, whereas donor growth increased, resulting in reduced weight discordance after FLC. The Quintero stage, pre-FLC sFGR, and post-FLC abnormal UAD were useful predictors of sFGR after FLC in TTTS.
Keyword
Figure
Reference
-
Reference
1. Chmait RH, Chon AH, Schrager SM, Kontopoulos EV, Quintero RA, Vanderbilt DL. Donor catch-up growth after laser surgery for twin-twin transfusion syndrome. Early Hum Dev. 2015; 91:751–4.
Article2. Bamberg C, Hecher K. Update on twin-to-twin transfusion syndrome. Best Pract Res Clin Obstet Gynaecol. 2019; 58:55–65.
Article3. Sago H, Wada S. Fetal therapies as standard prenatal care in Japan. Obstet Gynecol Sci. 2020; 63:108–16.
Article4. Roberts D, Neilson JP, Kilby MD, Gates S. Interventions for the treatment of twin-twin transfusion syndrome. Cochrane Database Syst Rev. 2014; (1):CD002073.
Article5. Wang X, Li L, Yuan P, Zhao Y, Wei Y. Comparison of placental characteristics of twin-twin transfusion syndrome with and without selective intrauterine growth restriction. J Matern Fetal Neonatal Med. 2022; 35:4306–11.
Article6. Groene SG, Tollenaar LSA, van Klink JMM, Haak MC, Klumper FJCM, Middeldorp JM, et al. Twin-twin transfusion syndrome with and without selective fetal growth restriction prior to fetoscopic laser surgery: short and long-term outcome. J Clin Med. 2019; 8:969.
Article7. Chmait RH, Korst LM, Bornick PW, Allen MH, Quintero RA. Fetal growth after laser therapy for twin-twin transfusion syndrome. Am J Obstet Gynecol. 2008; 199:47.e1–6.
Article8. Townsend R, Khalil A. Fetal growth restriction in twins. Best Pract Res Clin Obstet Gynaecol. 2018; 49:79–88.
Article9. Bennasar M, Eixarch E, Martinez JM, Gratacós E. Selective intrauterine growth restriction in monochorionic diamniotic twin pregnancies. Semin Fetal Neonatal Med. 2017; 22:376–82.
Article10. Townsend R, Khalil A. Twin pregnancy complicated by selective growth restriction. Curr Opin Obstet Gynecol. 2016; 28:485–91.
Article11. Jee J, Hong SJ, Ha S, Kim HY, Ahn KH, Hong SC, et al. Pregnancy outcomes in twin pregnancies over 10 years. Obstet Gynecol Sci. 2022; 66:20–5.
Article12. Townsend R, D’Antonio F, Sileo FG, Kumbay H, Thilaganathan B, Khalil A. Perinatal outcome of monochorionic twin pregnancy complicated by selective fetal growth restriction according to management: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2019; 53:36–46.
Article13. Maulik D, Mundy D, Heitmann E, Maulik D. Umbilical artery Doppler in the assessment of fetal growth restriction. Clin Perinatol. 2011; 38:65–82. vi
Article14. Moreira de Sa RA, Salomon LJ, Takahashi Y, Yamamoto M, Ville Y. Analysis of fetal growth after laser therapy in twin-to-twin transfusion syndrome. J Ultrasound Med. 2005; 24:1213–9. quiz 1220–1.
Article15. Maschke C, Franz AR, Ellenrieder B, Hecher K, Diemert A, Bartmann P. Growth after intrauterine laser coagulation for twin-twin transfusion syndrome. Arch Dis Child Fetal Neonatal Ed. 2010; 95:F115–7.
Article16. Akkermans J, Peeters SH, Klumper FJ, Lopriore E, Middeldorp JM, Oepkes D. Twenty-five years of fetoscopic laser coagulation in twin-twin transfusion syndrome: a systematic review. Fetal Diagn Ther. 2015; 38:241–53.
Article17. Kim R, Lee MY, Won HS, Kim JM, Lee YJ, Jeong BD, et al. Perinatal outcomes and factors affecting the survival rate of fetuses with twin-to-twin transfusion syndrome treated with fetoscopic laser coagulation: a single-center seven-year experience. J Matern Fetal Neonatal Med. 2022; 35:5595–606.
Article18. Quintero RA, Morales WJ, Allen MH, Bornick PW, Johnson PK, Kruger M. Staging of twin-twin transfusion syndrome. J Perinatol. 1999; 19:550–5.
Article19. Society for Maternal-Fetal Medicine, Simpson LL. Twin-twin transfusion syndrome. Am J Obstet Gynecol. 2013; 208:3–18.
Article20. Khalil A, Rodgers M, Baschat A, Bhide A, Gratacos E, Hecher K, et al. ISUOG practice guidelines: role of ultrasound in twin pregnancy. Ultrasound Obstet Gynecol. 2016; 47:247–63.
Article21. Kiserud T, Piaggio G, Carroli G, Widmer M, Carvalho J, Neerup Jensen L, et al. The World Health Organization fetal growth charts: a multinational longitudinal study of ultrasound biometric measurements and estimated fetal weight. PLoS Med. 2017; 14:e1002220.
Article22. Kalafat E, Thilaganathan B, Papageorghiou A, Bhide A, Khalil A. Significance of placental cord insertion site in twin pregnancy. Ultrasound Obstet Gynecol. 2018; 52:378–84.
Article23. Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011; 12:77.
Article24. Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. 2nd ed. New York (NY): Springer;2001.25. Panteghini M, Tonni G, Mansournia MA. To move beyond statistical significance and consider clinical relevance. Clin Oncol (R Coll Radiol). 2022; 34:e315.
Article26. Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, et al. Williams obstetrics. 25th ed. New York (NY): McGraw-Hill Medical;2014.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fetal Survival Immediate after Fetoscopic Laser Ablation in Twin to Twin Transfusion Syndrome
- Management of discordant twin
- Feasibility of fetoscopic laser coagulation in triplet pregnancy
- Three cases of Twin-to-Twin Transfusion Syndrome which were managed with maternal digitalization
- A Clinical Study of Twin Pregnancies with One Fetal Demise