J Korean Neurosurg Soc.
2023 Nov;66(6):726-734. 10.3340/jkns.2023.0115.
Balancing Bleeding Risk and Thromboembolic Complications in Elderly Chronic Subdural Hematoma Patients Undergoing Burr Hole Trephination : A Multicenter Retrospective Cohort Study and Literature Review
- Affiliations
-
- 1Department of Neurosurgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Neurosurgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Neurosurgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Neurosurgery, Yeouido St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Neurosurgery, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2547466
- DOI: http://doi.org/10.3340/jkns.2023.0115
Abstract
Objective
: Chronic subdural hematoma (CSDH) patients using antithrombotic agents (AT) at high risk for cardiovascular disease are increasing. The authors aimed to analyze the factors influencing outcome by targeting patients using AT and to establish a desirable treatment strategy.
Methods
: A retrospective analysis was performed on data from 462 patients who underwent burr hole trephination (BHT) surgery for CSDH at five hospitals from March 2010 to June 2021. Outcomes included incidence of postoperative acute bleeding, recurrence rate, and morbidity or mortality rate. Patients were divided into the following four groups based on their history of AT use : no AT. Only antiplatelet agents (AP), only anticoagulants (AC), both of AP and AC. In addition, a concurrent literature review was conducted alongside our cohort study.
Results
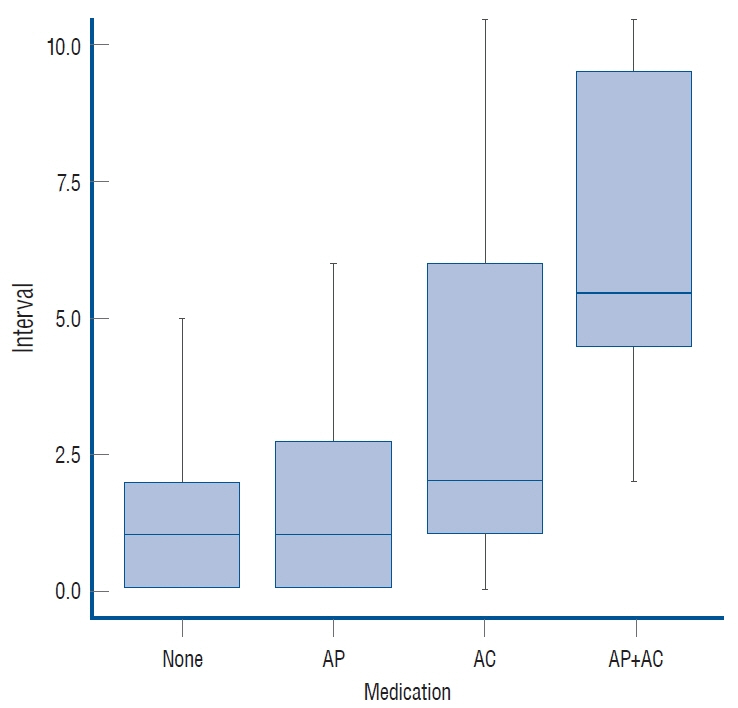
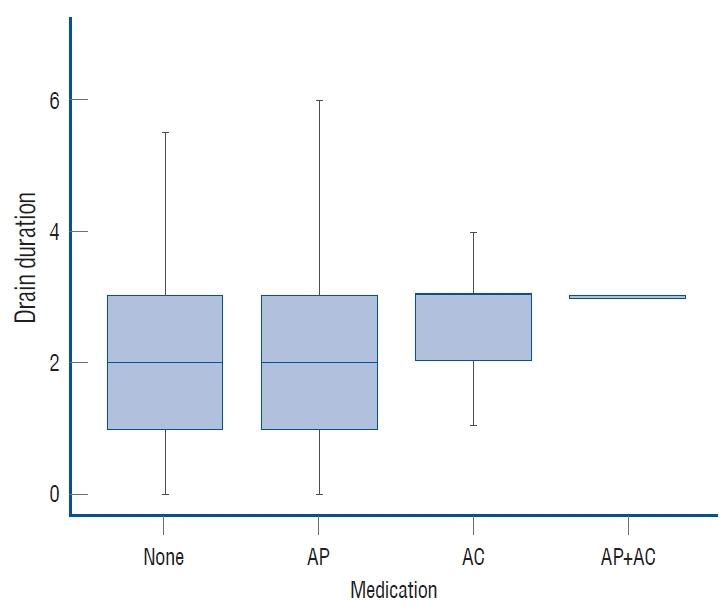
: Of 462 patients, 119 (119/462, 25.76%) were using AT. AP prescription did not significantly delay surgery (p=0.318), but AC prescription led to a significant increase in the time interval from admission to operation (p=0.048). After BHT, AP or AC intake significantly increased the period required for an in-dwelling drain (p=0.026 and p=0.037). The use of AC was significantly related to acute bleeding (p=0.044), while the use of AP was not (p=0.808). Use of AP or AC had no significant effect on CSDH recurrence (p=0.517 and p=1.000) or reoperation (p=0.924 and p=1.000). Morbidity was not statistically correlated with use of either AP or AC (p=0.795 and p=0.557, respectively), and there was no significant correlation with mortality for use of these medications (p=0.470 and p=1.000).
Conclusion
: Elderly CSDH patients may benefit from maintenance of AT therapy during BHT due to reduced thromboembolic risk. However, the use of AC necessitates individualized due to potential postoperative bleeding. Careful post-operative monitoring could mitigate prognosis and recurrence impacts.
Keyword
Figure
Cited by 1 articles
-
Editors’ Pick in November 2023
Moonyoung Chung
J Korean Neurosurg Soc. 2023;66(6):609-610. doi: 10.3340/jkns.2023.0218.
Reference
-
References
1. Abboud T, Dührsen L, Gibbert C, Westphal M, Martens T. Influence of antithrombotic agents on recurrence rate and clinical outcome in patients operated for chronic subdural hematoma. Neurocirugia (Astur : Engl Ed). 29:86–92. 2018.
Article2. Amano T, Takahara K, Maehara N, Shimogawa T, Mukae N, Sayama T, et al. Optimal perioperative management of antithrombotic agents in patients with chronic subdural hematoma. Clin Neurol Neurosurg. 151:43–50. 2016.
Article3. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation. 140:e596–e646. 2019.4. Chan YH, See LC, Tu HT, Yeh YH, Chang SH, Wu LS, et al. Efficacy and safety of apixaban, dabigatran, rivaroxaban, and warfarin in asians with nonvalvular atrial fibrillation. J Am Heart Assoc. 7:e008150. 2018.
Article5. Choi J, Pyen J, Cho S, Kim J, Koo Y, Whang K. Influence of antithrombotic medication on the risk of chronic subdural hematoma recurrence after burr-hole surgery. J Korean Neurosurg Soc. 63:513–518. 2020.
Article6. Ducruet AF, Grobelny BT, Zacharia BE, Hickman ZL, DeRosa PL, Andersen KN, et al. The surgical management of chronic subdural hematoma. Neurosurg Rev. 35:155–169. discussion 169. 2012.
Article7. Fornebo I, Sjåvik K, Alibeck M, Kristiansson H, Ståhl F, Förander P, et al. Role of antithrombotic therapy in the risk of hematoma recurrence and thromboembolism after chronic subdural hematoma evacuation: a population-based consecutive cohort study. Acta Neurochir (Wien). 159:2045–2052. 2017.
Article8. Gaist D, García Rodríguez LA, Hellfritzsch M, Poulsen FR, Halle B, Hallas J, et al. Association of antithrombotic drug use with subdural hematoma risk. JAMA. 317:836–846. 2017.
Article9. Gerstein NS, Albrechtsen CL, Mercado N, Cigarroa JE, Schulman PM. A comprehensive update on aspirin management during noncardiac surgery. Anesth Analg. 131:1111–1123. 2020.
Article10. Guha D, Coyne S, Macdonald RL. Timing of the resumption of antithrombotic agents following surgical evacuation of chronic subdural hematomas: a retrospective cohort study. J Neurosurg. 124:750–759. 2016.
Article11. Hamou HA, Clusmann H, Schulz JB, Wiesmann M, Altiok E, Höllig A. Chronic subdural hematoma. Dtsch Arztebl Int. 119:208–213. 2022.12. Holl DC, Volovici V, Dirven CMF, Peul WC, van Kooten F, Jellema K, et al. Pathophysiology and nonsurgical treatment of chronic subdural hematoma: from past to present to future. World Neurosurg. 116:402–411.e2. 2018.
Article13. Kawakami Y, Chikama M, Tamiya T, Shimamura Y. Coagulation and fibrinolysis in chronic subdural hematoma. Neurosurgery. 25:25–29. 1989.
Article14. Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 45:2160–2236. 2014.
Article15. Kerttula S, Huttunen J, Leinonen V, Kämäräinen OP, Danner N. The effect of antithrombotic therapy on the recurrence and outcome of chronic subdural hematoma after burr-hole craniostomy in a population-based cohort. Acta Neurochir (Wien). 164:2699–2708. 2022.
Article16. Lewis SR, Pritchard MW, Schofield-Robinson OJ, Alderson P, Smith AF. Continuation versus discontinuation of antiplatelet therapy for bleeding and ischaemic events in adults undergoing non-cardiac surgery. Cochrane Database Syst Rev. 7:CD012584. 2018.
Article17. Mehta V, Harward SC, Sankey EW, Nayar G, Codd PJ. Evidence based diagnosis and management of chronic subdural hematoma: a review of the literature. J Clin Neurosci. 50:7–15. 2018.
Article18. Moster M, Bolliger D. Perioperative guidelines on antiplatelet and anticoagulant agents: 2022 update. Curr Anesthesiol Rep. 12:286–296. 2022.
Article19. Scerrati A, Germanò A, Trevisi G, Visani J, Lofrese G, D’Angelo L, et al. Timing of low-dose aspirin discontinuation and the influence on clinical outcome of patients undergoing surgery for chronic subdural hematoma. World Neurosurg. 129:e695–e699. 2019.
Article20. Sim YW, Min KS, Lee MS, Kim YG, Kim DH. Recent changes in risk factors of chronic subdural hematoma. J Korean Neurosurg Soc. 52:234–239. 2012.
Article21. Wada M, Yamakami I, Higuchi Y, Tanaka M, Suda S, Ono J, et al. Influence of antiplatelet therapy on postoperative recurrence of chronic subdural hematoma: a multicenter retrospective study in 719 patients. Clin Neurol Neurosurg. 120:49–54. 2014.
Article22. Weigel R, Schmiedek P, Krauss JK. Outcome of contemporary surgery for chronic subdural haematoma: evidence based review. J Neurol Neurosurg Psychiatry. 74:937–943. 2003.
Article23. Weir B. Oncotic pressure of subdural fluids. J Neurosurg. 53:512–515. 1980.
Article24. Younsi A, Riemann L, Habel C, Fischer J, Beynon C, Unterberg AW, et al. Relevance of comorbidities and antithrombotic medication as risk factors for reoperation in patients with chronic subdural hematoma. Neurosurg Rev. 45:729–739. 2022.
Article25. Yuksel MO, Cevik S, Erdogan B, Tunckale T, Katar S, Isik S, et al. Effect of antithrombotic therapy on development of acute subdural hematoma after burr hole drainage of chronic subdural hematoma. Turk Neurosurg. 30:758–762. 2020.26. Zhang JJY, Aw NMY, Tan CH, Lee KS, Chen VHE, Wang S, et al. Impact of time to resumption of antithrombotic therapy on outcomes after surgical evacuation of chronic subdural hematoma: a multicenter cohort study. J Clin Neurosci. 89:389–396. 2021.
Article27. Zhang P, Li Y, Huang J, Zhang H, Wang X, Dong L, et al. Chronic subdural haematoma in antithrombotic cohorts: characteristics, surgical outcomes, and recurrence. Br J Neurosurg. 34:408–415. 2020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting the Reaccumulation of Chronic Subdural Hematoma after Burr-hole Trephination and Closed-system Drainage
- Remote Hemorrhage after Burr Hole Drainage of Chronic Subdural Hematoma
- Usefulness of Allogenic Acellular Dermal Matrix for Prevention of Scalp Depressio
- Delayed Multiple Intracerebral Hemorrhage After Burr Hole Drainage of Chronic Subdural Hematoma During Failure of Warfarin Resumption in Atrial Fibrillation
- Recurrence of the Chronic Subdural Hematoma after Burr-Hole Drainage with or without Intraoperative Saline Irrigation