Korean J Schizophr Res.
2023 Oct;26(2):61-69. 10.16946/kjsr.2023.26.2.61.
Perceptions of Coronavirus Disease 2019 (COVID-19) in Patients With Schizophrenia
- Affiliations
-
- 1Department of Psychiatry, Medical Foundation Yongin Mental Hospital, Yongin, Korea
- 2Department of Psychiatry, Seoul Bukbu Hospital, Seoul, Korea
- KMID: 2547423
- DOI: http://doi.org/10.16946/kjsr.2023.26.2.61
Abstract
Objectives
The aim of this study was to investigate whether patients with schizophrenia are aware of the current status and have accurate information about COVID-19.
Methods
The participants consisted of 161 inpatients and 117 outpatients with schizophrenia and 40 normal controls. The subjects completed self-report questionnaires measuring changes in their daily life, their perceptions of the current status of COVID-19 and their basic knowledge about the disease.
Results
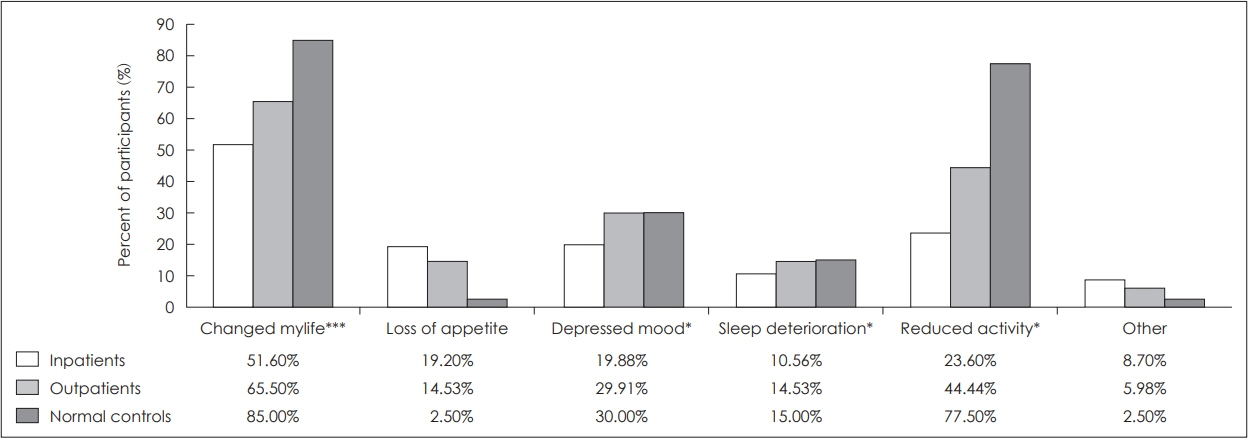
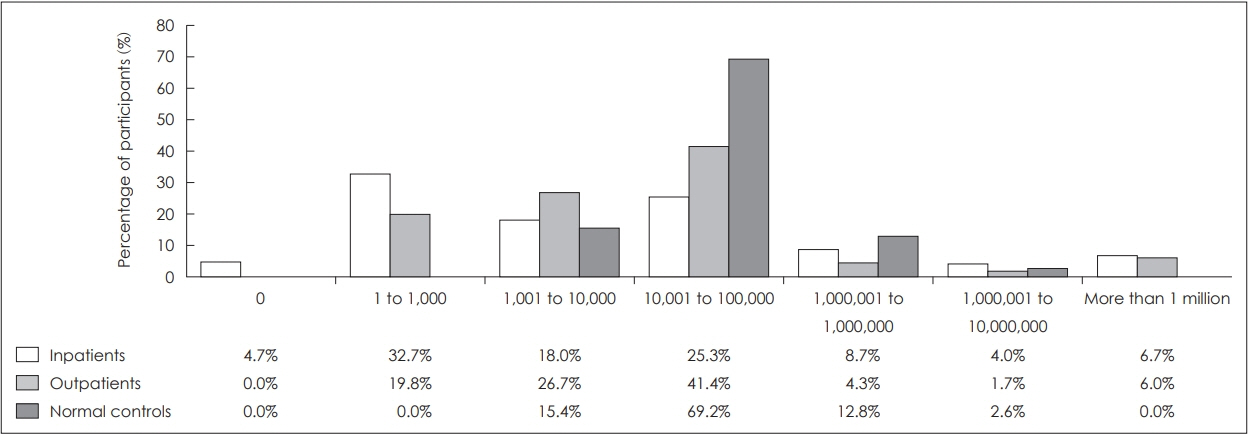
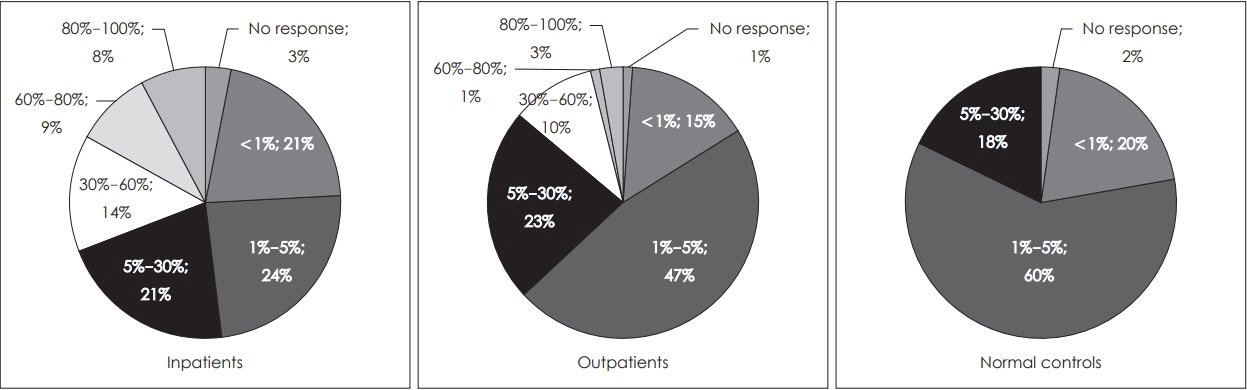
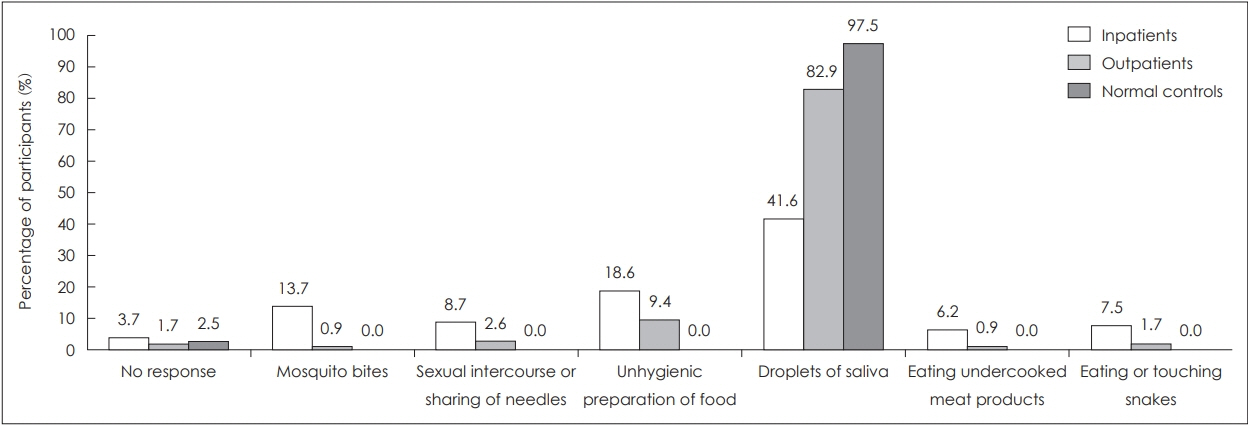
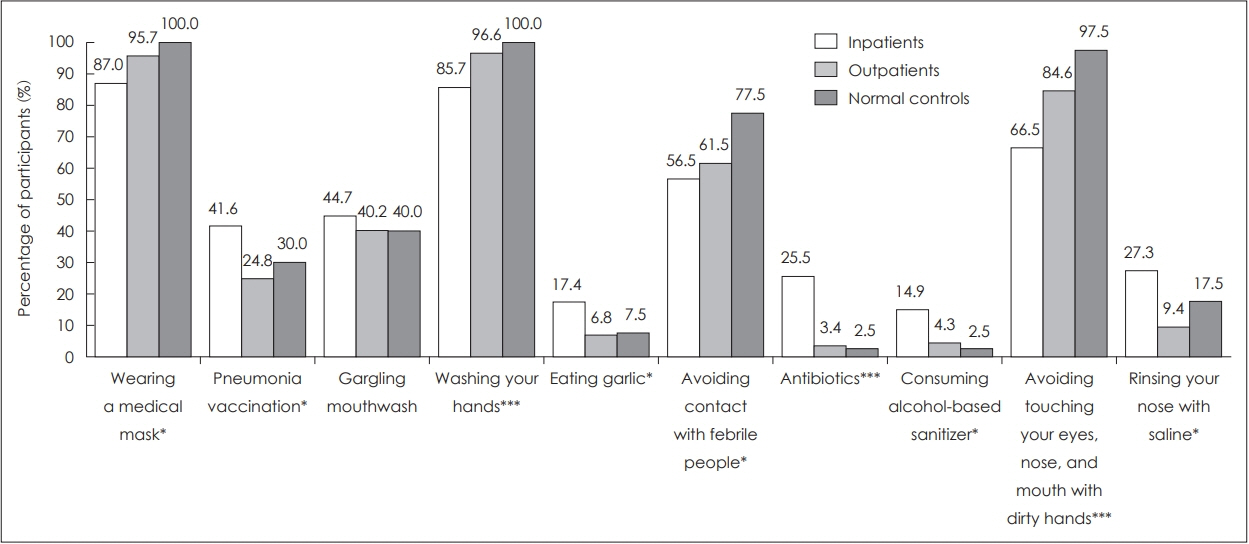
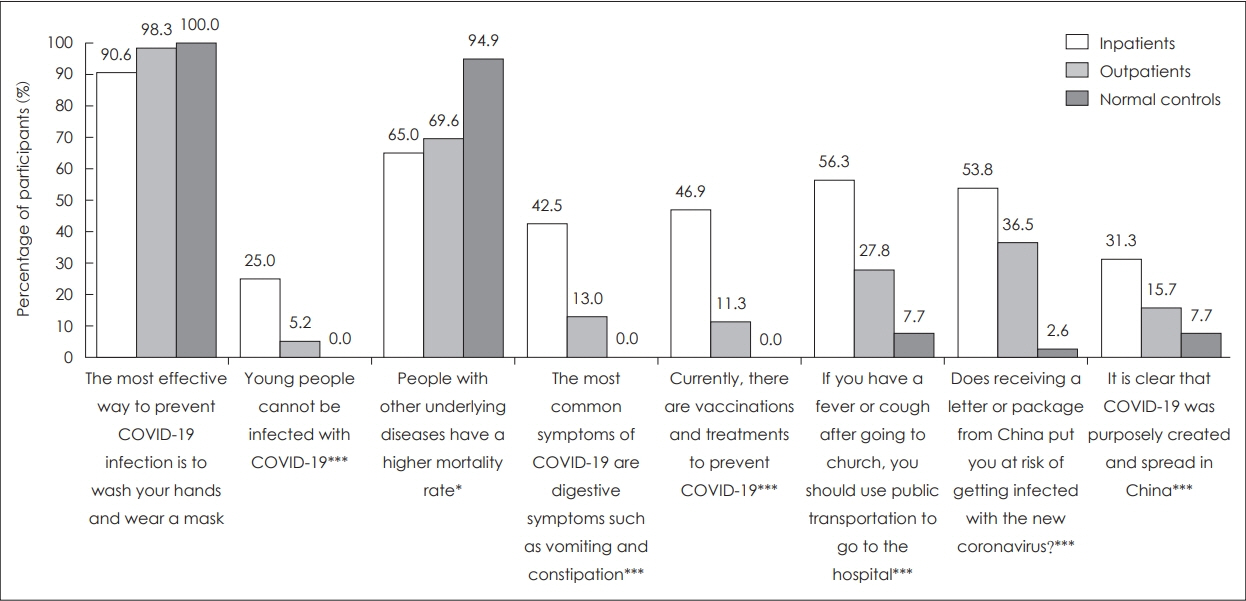
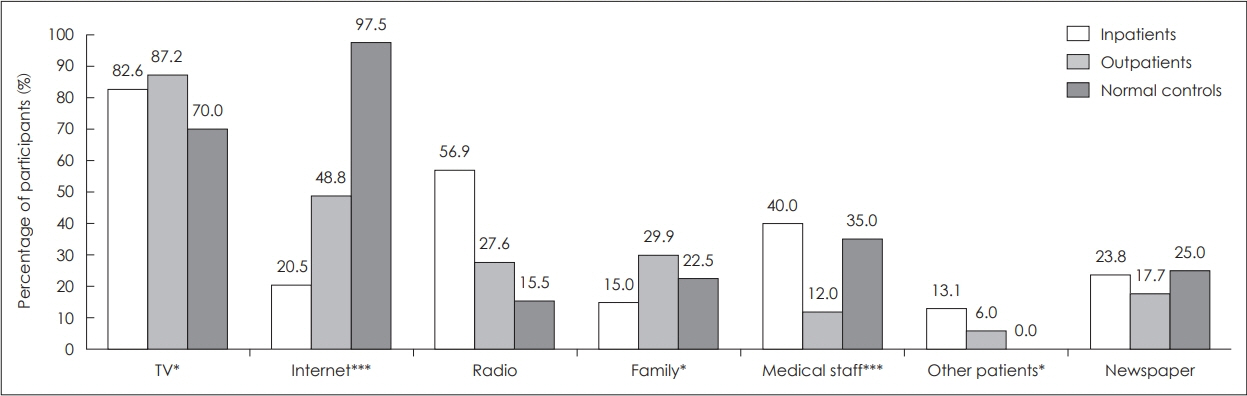
Compared to the normal control group, the inpatients and outpatients with schizophrenia underestimated the cumulative number of confirmed COVID-19 cases and overestimated the mortality rate of COVID-19. The mortality rates of COVID-19 and the common cold were higher in the order of inpatients, outpatients, and normal controls. The main route of SARS-CoV-2 infection and the main symptoms of COVID-19 were accurately recognized by more than 95% in the normal group and more than 80% in outpatients, but inpatients chose the correct answers at a lower rate. In the questions about misperceptions about COVID-19, the correct answer rate was high in the order of normal controls, outpatients, and inpatients. Most patients with schizophrenia obtained information about COVID-19 on TV, while most normal controls collected information through the internet.
Conclusion
This study showed that awareness of COVID-19 among patients with schizophrenia is insufficient. Additional measures are needed to provide accurate information and the current status of COVID-19 to patients with schizophrenia.
Keyword
Figure
Reference
-
1. WHO. WHO Coronavirus Disease (COVID-19) Dashboard 2022 Sep 14; Available from: https://covid19.who.int/.2. Jeon HL, Kwon JS, Park SH, Shin JY. Association of mental disorders with SARS-CoV-2 infection and severe health outcomes: nationwide cohort study. The British Journal of Psychiatry. 2021; 218:344–351.
Article3. Wang Q, Xu R, Volkow ND. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021; 20:124–130.
Article4. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020; 7:e21.
Article5. Larkin A, Hutton P. Systematic review and meta-analysis of factors that help or hinder treatment decision-making capacity in psychosis. The British Journal of Psychiatry. 2017; 211:205–215.
Article6. Maguire PA, Reay RE, Looi JC. Nothing to sneeze at–uptake of protective measures against an influenza pandemic by people with schizophrenia: willingness and perceived barriers. Australasian Psychiatry. 2019; 27:171–178.
Article7. Van Haaster I, Lesage A, Cyr M, Toupin J. Problems and needs for care of patients suffering from severe mental illness. Social psychiatry and psychiatric epidemiology. 1994; 29:141–148.
Article8. Fonseca L, Diniz E, Mendonca G, Malinowski F, Mari J, Gadelha A. Schizophrenia and COVID-19: risks and recommendations. Brazilian Journal of Psychiatry. 2020; 42:236–238.
Article9. Kozloff N, Mulsant BH, Stergiopoulos V, Voineskos AN. The COVID-19 Global Pandemic: Implications for People With Schizophrenia and Related Disorders. Schizophr Bull. 2020; 46:752–757.
Article10. Shinn AK, Viron M. Perspectives on the COVID-19 pandemic and individuals with serious mental illness. The Journal of Clinical Psychiatry. 2020; 81:14205.
Article11. Bradford DW, Kim MM, Braxton LE, Marx CE, Butterfield M, Elbogen EB. Access to medical care among persons with psychotic and major affective disorders. Psychiatric Services. 2008; 59:847–852.
Article12. Muruganandam P, Neelamegam S, Menon V, Alexander J, Chaturvedi SK. COVID-19 and severe mental illness: impact on patients and its relation with their awareness about COVID-19. Psychiatry research. 2020; 291:113265.
Article13. Thomson S, Doan T, Liu D, Schubert KO, Toh J, Boyd MA, et al. Supporting the vulnerable: developing a strategic community mental health response to the COVID-19 pandemic. Australas Psychiatry. 2020; 1039856220944701.
Article14. Geldsetzer P. Use of rapid online surveys to assess people’s perceptions during infectious disease outbreaks: a cross-sectional survey on COVID-19. J Med Internet Res. 2020; 22:e18790.
Article15. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2022; 20:1537–1545.16. Coronavirus Infectious Disease-19 Outbreak in Korea. 2020 Sep 29; Available from: http://ncov.mohw.go.kr/tcmBoardView.do?brdId=&brdGubun=&dataGubun=&ncvContSeq=360121&contSeq=360121&board_id=140&gubun=BDJ.17. Natale A, Concerto C, Rodolico A, Birgillito A, Bonelli M, Martinez M, et al. Risk perception among psychiatric patients during the COVID-19 pandemic. Int J Environ Res Public Health. 2022; 19:2620.
Article18. Teixeira AL, Krause TM, Ghosh L, Shahani L, Machado-Vieira R, Lane SD, et al. Analysis of COVID-19 infection and mortality among patients with psychiatric disorders, 2020. JAMA Netw Open. 2021; 4:e2134969.
Article19. Maguire PA, Looi JC. Vulnerability of people with schizophrenia to COVID-19. Aust N Z J Psychiatry. 2020; 54:1044.
Article20. Maguire PA, Reay RE, Looi JCL. Nothing to sneeze at–uptake of protective measures against an influenza pandemic by people with schizophrenia: willingness and perceived barriers. Australasian Psychiatry. 2018; 27:171–178.
Article21. Tzur Bitan D, Krieger I, Kridin K, Komantscher D, Scheinman Y, Weinstein O, et al. COVID-19 prevalence and mortality among schizophrenia patients: a large-scale retrospective cohort study. Schizophrenia Bulletin. 2021; 47:1211–1217.
Article22. Fond G, Nemani K, Etchecopar-Etchart D, Loundou A, Goff DC, Lee SW, et al. Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: a systematic review and meta-analysis. JAMA psychiatry. 2021; 78:1208–1217.
Article23. De Hert M, Mazereel V, Detraux J, Van Assche K. Prioritizing COVID-19 vaccination for people with severe mental illness. World Psychiatry. 2021; 20:54.
Article24. WHO. Coronavirus disease (COVID-19) advice for the public: Myth busters. 2020 Sep 29; Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters.25. Romm T. Millions of tweets peddled conspiracy theories about coronavirus in other countries, an unpublished U.S. report says. 2020; Available from: https://www.washingtonpost.com/technology/2020/02/29/.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of multi-professional simulation-based training on perceptions of safety and preparedness among health workers caring for coronavirus disease 2019 patients in Pakistan
- Supporting Patients With Schizophrenia in the Era of COVID-19
- Treatment for Immune Thrombocytopenia in Coronavirus Disease 2019 (COVID-19) Infection after COVID-19 Vaccination: A Case Report
- COVID-19 from the Perspective of a Gastroenterologist
- Perception Related to Coronavirus Disease-19 Induced Anxiety in Elderly