Intest Res.
2023 Oct;21(4):481-492. 10.5217/ir.2023.00005.
Comparative outcomes of acute colonic diverticulitis in immunocompromised versus immunocompetent patients: a systematic review and meta-analysis
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea
- 2Division of Gastroenterology, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 3Department of Health Promotion Medicine, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, Seoul, Korea
- 4Division of Gastroenterology, Department of Internal Medicine, Jeju National University Hospital, Jeju National University College of Medicine, Jeju, Korea
- 5Digestive Disease Center, CHA Bundang Medica Center, CHA University, Seongnam, Korea
- 6Division of Gastroenterology, Department of Internal Medicine, Hallym University Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea
- 7Center for Colorectal Cancer, National Cancer Center, Goyang, Korea
- 8Division of Gastroenterology, Department of Internal Medicine, Daejeon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Daejeon, Korea
- 9Department of Radiology, Kyung Hee University Hospital, College of Medicine, Kyung Hee University, Seoul, Korea
- 10Division of Gastroenterology, Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2547198
- DOI: http://doi.org/10.5217/ir.2023.00005
Abstract
- Background/Aims
Immunocompromised patients with acute colonic diverticulitis are at high risk for complications and failure of non-surgical treatment. However, evidence on the comparative outcomes of immunocompromised and immunocompetent patients with diverticulitis is lacking. This systematic review and meta-analysis investigated the outcomes of medical treatment in immunocompromised and immunocompetent patients with diverticulitis.
Methods
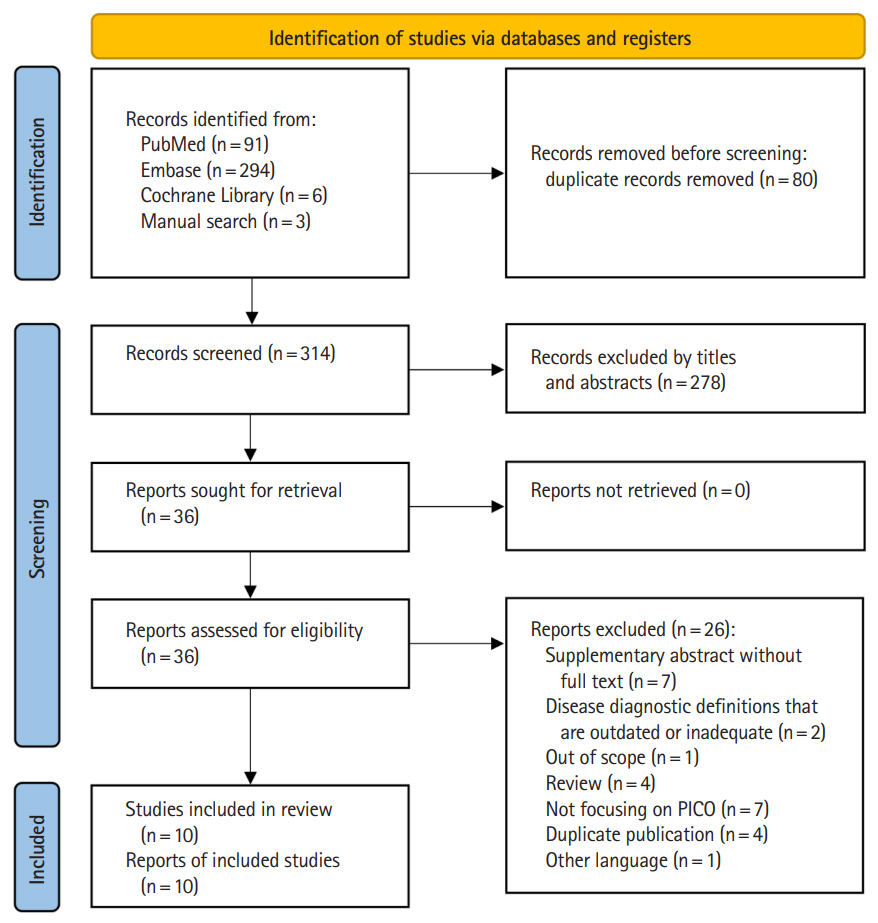
A comprehensive literature search was conducted in PubMed, Embase, and the Cochrane Library. Studies comparing the clinical outcomes of immunocompromised and immunocompetent patients with diverticulitis were included.
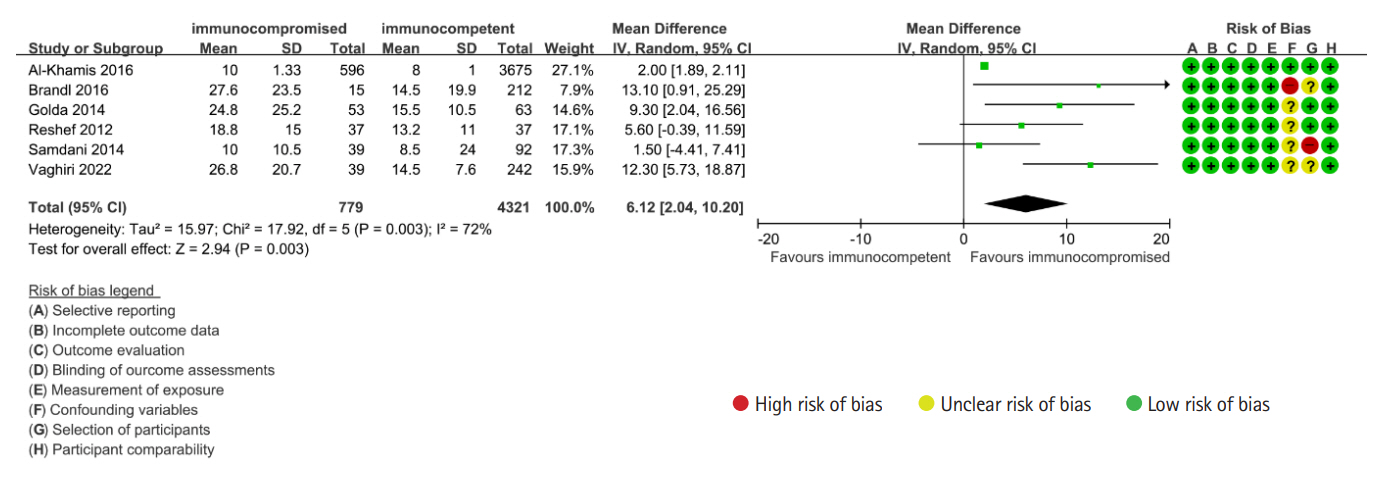
Results
A total of 10 studies with 1,946,461 subjects were included in the quantitative synthesis. The risk of emergency surgery and postoperative mortality after emergency surgery was significantly higher in immunocompromised patients than in immunocompetent patients with diverticulitis (risk ratio [RR], 1.76; 95% confidence interval [CI], 1.31–2.38 and RR, 3.05; 95% CI, 1.70–5.45, respectively). Overall risk of complications associated with diverticulitis was non-significantly higher in immunocompromised than in immunocompetent patients (RR, 1.24; 95% CI, 0.95–1.63). Overall mortality irrespective of surgery was significantly higher in immunocompromised than in immunocompetent patients with diverticulitis (RR, 3.65; 95% CI, 1.73–7.69). By contrast, postoperative mortality after elective surgery was not significantly different between immunocompromised and immunocompetent patients with diverticulitis. In subgroup analysis, the risk of emergency surgery and recurrence was significantly higher in immunocompromised patients with complicated diverticulitis, whereas no significant difference was shown in mild disease.
Conclusions
Immunocompromised patients with diverticulitis should be given the best medical treatment with multidisciplinary approach because they had increased risks of surgery, postoperative morbidity, and mortality than immunocompetent patients.
Figure
Cited by 1 articles
-
Not all acute colonic diverticulitis follows the same course: a potential risk for immunocompromised individuals
Yehyun Park
Intest Res. 2023;21(4):415-417. doi: 10.5217/ir.2023.00142.
Reference
-
1. Strate LL, Morris AM. Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology. 2019; 156:1282–1298.
Article2. Bharucha AE, Parthasarathy G, Ditah I, et al. Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am J Gastroenterol. 2015; 110:1589–1596.
Article3. Wheat CL, Strate LL. Trends in hospitalization for diverticulitis and diverticular bleeding in the United States from 2000 to 2010. Clin Gastroenterol Hepatol. 2016; 14:96–103.
Article4. Humes DJ, Solaymani-Dodaran M, Fleming KM, Simpson J, Spiller RC, West J. A population-based study of perforated diverticular disease incidence and associated mortality. Gastroenterology. 2009; 136:1198–1205.
Article5. Humes DJ, Fleming KM, Spiller RC, West J. Concurrent drug use and the risk of perforated colonic diverticular disease: a population-based case-control study. Gut. 2011; 60:219–224.
Article6. Broersen LHA, Horváth-Puhó E, Pereira AM, Erichsen R, Dekkers OM, Sørensen HT. Corticosteroid use and mortality risk in patients with perforated colonic diverticular disease: a population-based cohort study. BMJ Open Gastroenterol. 2017; 4:e000136.
Article7. Biondo S, Borao JL, Kreisler E, et al. Recurrence and virulence of colonic diverticulitis in immunocompromised patients. Am J Surg. 2012; 204:172–179.
Article8. Brandl A, Kratzer T, Kafka-Ritsch R, et al. Diverticulitis in immunosuppressed patients: a fatal outcome requiring a new approach? Can J Surg. 2016; 59:254–261.
Article9. Tyau ES, Prystowsky JB, Joehl RJ, Nahrwold DL. Acute diverticulitis: a complicated problem in the immunocompromised patient. Arch Surg. 1991; 126:855–858.10. Peery AF, Shaukat A, Strate LL. AGA clinical practice update on medical management of colonic diverticulitis: expert review. Gastroenterology. 2021; 160:906–911.
Article11. Nagata N, Ishii N, Manabe N, et al. Guidelines for colonic diverticular bleeding and colonic diverticulitis: Japan Gastroenterological Association. Digestion. 2019; 99 Suppl 1:1–26.
Article12. Sartelli M, Weber DG, Kluger Y, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020; 15:32.13. McKechnie T, Lee Y, Kruse C, et al. Operative management of colonic diverticular disease in the setting of immunosuppression: a systematic review and meta-analysis. Am J Surg. 2021; 221:72–85.
Article14. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA Statement. BMJ. 2009; 339–b2535.15. Kim SY, Park JE, Lee YJ, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013; 66:408–414.
Article16. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560.
Article17. Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022) [Internet]. c2022. [cited 2023 Mar 30]. www.training.cochrane.org/handbook.18. Reshef A, Stocchi L, Kiran RP, et al. Case-matched comparison of perioperative outcomes after surgical treatment of sigmoid diverticulitis in solid organ transplant recipients versus immunocompetent patients. Colorectal Dis. 2012; 14:1546–1552.
Article19. Cronley K, Wenzke J, Hussan H, et al. Diverticulitis in HIV-infected patients within the United States. HIV Med. 2016; 17:216–221.20. Golda T, Kreisler E, Mercader C, Frago R, Trenti L, Biondo S. Emergency surgery for perforated diverticulitis in the immunosuppressed patient. Colorectal Dis. 2014; 16:723–731.
Article21. Al-Khamis A, Abou Khalil J, Demian M, et al. Sigmoid colectomy for acute diverticulitis in immunosuppressed vs immunocompetent patients: outcomes from the ACS-NSQIP database. Dis Colon Rectum. 2016; 59:101–109.
Article22. Samdani T, Pieracci FM, Eachempati SR, et al. Colonic diverticulitis in chemotherapy patients: should operative indications change? A retrospective cohort study Int J Surg. 2014; 12:1489–1494.
Article23. Halabi WJ, Jafari MD, Nguyen VQ, et al. Colorectal surgery in kidney transplant recipients: a decade of trends and outcomes in the United States. Am Surg. 2013; 79:1026–1033.
Article24. Vaghiri S, Prassas D, Knoefel WT, Krieg A. Surgical management in immunosuppressed patients with sigmoid diverticulitis, still a challenge: a single-center observational study. Int J Colorectal Dis. 2022; 37:1909–1917.
Article25. Sugrue J, Lee J, Warner C, et al. Acute diverticulitis in renal transplant patients: should we treat them differently? Surgery. 2018; 163:857–865.
Article26. Chabok A, Påhlman L, Hjern F, Haapaniemi S, Smedh K; AVOD Study Group. Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg. 2012; 99:532–539.27. Daniels L, Ünlü Ç, de Korte N, et al. Randomized clinical trial of observational versus antibiotic treatment for a first episode of CT-proven uncomplicated acute diverticulitis. Br J Surg. 2017; 104:52–61.28. Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014; 57:284–294.
Article29. Hall J, Hardiman K, Lee S, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the treatment of left-sided colonic diverticulitis. Dis Colon Rectum. 2020; 63:728–747.
Article30. Francis NK, Sylla P, Abou-Khalil M, et al. EAES and SAGES 2018 consensus conference on acute diverticulitis management: evidence-based recommendations for clinical practice. Surg Endosc. 2019; 33:2726–2741.
Article31. Coccolini F, Improta M, Sartelli M, et al. Acute abdomen in the immunocompromised patient: WSES, SIS-E, WSIS, AAST, and GAIS guidelines. World J Emerg Surg. 2021; 16:40.
Article32. Bootun R. Effects of immunosuppressive therapy on wound healing. Int Wound J. 2013; 10:98–104.
Article33. Dean PG, Lund WJ, Larson TS, et al. Wound-healing complications after kidney transplantation: a prospective, randomized comparison of sirolimus and tacrolimus. Transplantation. 2004; 77:1555–1561.
Article34. Yamada E, Ohkubo H, Higurashi T, et al. Visceral obesity as a risk factor for left-sided diverticulitis in Japan: a multicenter retrospective study. Gut Liver. 2013; 7:532–538.
Article35. Kim MJ, Woo YS, Kim ER, et al. Is colonoscopy necessary after computed tomography diagnosis of acute diverticulitis? Intest Res. 2014; 12:221–228.
Article36. Oh HK, Han EC, Ha HK, et al. Surgical management of colonic diverticular disease: discrepancy between right- and left- sided diseases. World J Gastroenterol. 2014; 20:10115–10120.
Article37. Perkins JD, Shield CF 3rd, Chang FC, Farha GJ. Acute diverticulitis: comparison of treatment in immunocompromised and nonimmunocompromised patients. Am J Surg. 1984; 148:745–748.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Colon Cancer with Ovarian Metastasis Mimicking Acute Diverticulitis
- Clinical characteristics of right versus left colonic diverticulitis
- Not all acute colonic diverticulitis follows the same course: a potential risk for immunocompromised individuals
- Diagnosis and management of acute colonic diverticulitis: results of a survey among Korean gastroenterologists
- Diagnosis and Treatment of Colonic Diverticular Disease