Anesth Pain Med.
2023 Jul;18(3):296-301. 10.17085/apm.22261.
Sudden mode change of permanent pacemaker during living donor liver transplantation - A case report -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2547039
- DOI: http://doi.org/10.17085/apm.22261
Abstract
- Background
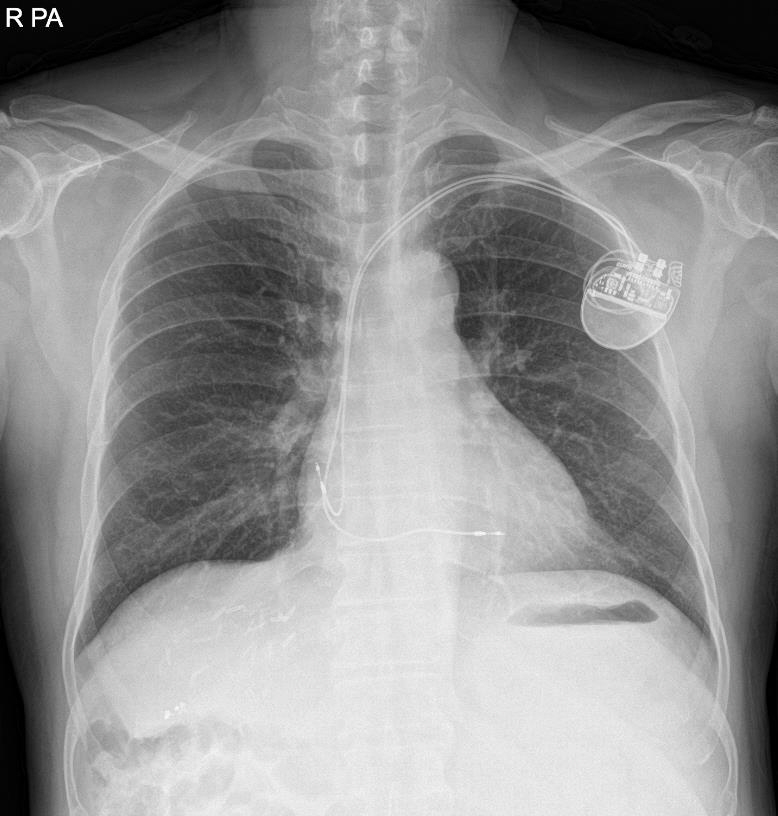
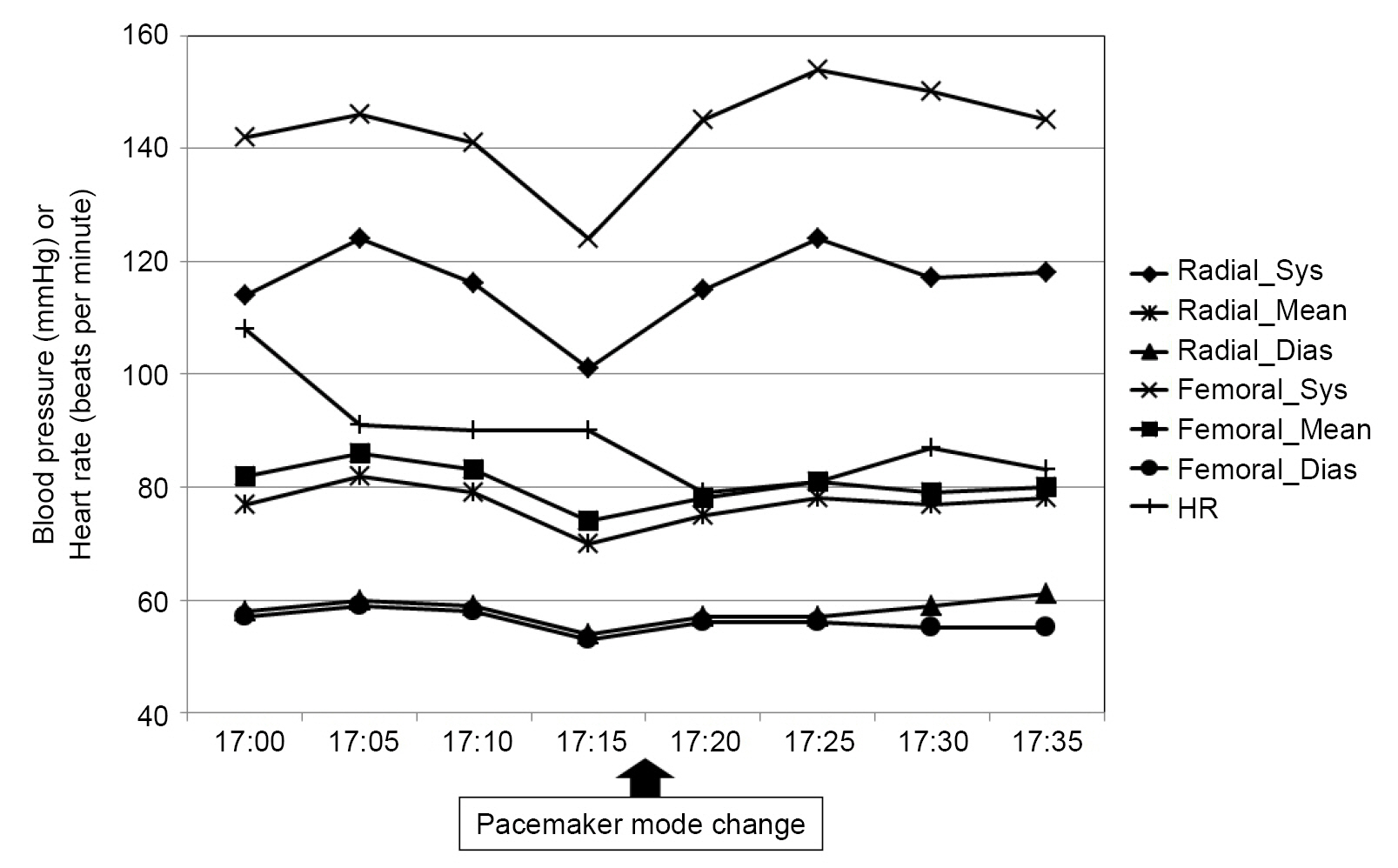
Pacemakers assist circulation by generating electrical impulses. Patients with pacemakers scheduled to undergo surgery are vulnerable to device-related complications. Therefore, careful perioperative management is required to prevent undesirable events. Case: A 66-year-old man with alcohol-related hepatocellular carcinoma was referred for liver transplantation. The pacemaker was inserted preoperatively to manage sick sinus syndrome and paroxysmal atrial fibrillation. Overall liver transplantation was performed without any adverse events. However, the pacemaker suddenly failed to provide regular pacing rhythm during abdominal closure. Fortunately, the native heart rate was maintained above 70 beats per minute and blood pressure did not fluctuate after pacing failure. After retrospective analysis, the duration setting of preoperative pacemaker reprogramming (24 h) was revealed as the cause of unexpected pacing failure.
Conclusions
Anesthesiologists should be alert in patients with pacemakers because minor errors may lead to inadvertent failure of pacing or severe hemodynamic instability.
Figure
Reference
-
1. Bae MH. Cardiac implantable electronic device therapy in Korea: increasing but still quite low. Korean Circ J. 2019; 49:853–5.
Article2. Practice advisory for the perioperative management of patients with cardiac implantable electronic devices: pacemakers and implantable cardioverter-defibrillators 2020: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with cardiac implantable electronic devices: erratum. Anesthesiology 2020; 132: 938. Erratum for: Anesthesiology. 2020; 132:225–52.3. Bang SR, Ahn HJ, Kim GS, Yang M, Gwak MS, Ko JS, et al. Predictors of high intraoperative blood loss derived by simple and objective method in adult living donor liver transplantation. Transplant Proc. 2010; 42:4148–50.
Article4. Mulpuru SK, Madhavan M, McLeod CJ, Cha YM, Friedman PA. Cardiac pacemakers: function, troubleshooting, and management: part 1 of a 2-part series. J Am Coll Cardiol. 2017; 69:189–210.5. Aquilina O. A brief history of cardiac pacing. Images Paediatr Cardiol. 2006; 8:17–81.6. Madhavan M, Mulpuru SK, McLeod CJ, Cha YM, Friedman PA. Advances and future directions in cardiac pacemakers: part 2 of a 2-part series. J Am Coll Cardiol. 2017; 69:211–35.7. Boston Scientific. ACCOLADE MRI pacemaker spec sheet. Scientific [Internet]. 2016 [updated 2020; cited 2022 Oct 20]. Available from https://www.bostonscientific.com/content/dam/bostonscientific/ep/general/CRM-324101-AE_ACCOLADEMRI%20Pacemaker%20SpecSheet-FINAL.pdf.8. Stone ME, Salter B, Fischer A. Perioperative management of patients with cardiac implantable electronic devices. Br J Anaesth. 2011; 107 Suppl 1:i16–26.
Article9. Schulman PM, Rozner MA. Case report: use caution when applying magnets to pacemakers or defibrillators for surgery. Anesth Analg. 2013; 117:422–7.10. Kitajima A, Nakatomi T, Otsuka Y, Sanui M, Lefor AK. Cardiac arrest due to failed pacemaker capture after peripheral nerve blockade with levobupivacaine: a case report. A A Pract. 2021; 15:e01445.
Article11. Umei TC, Awaya T, Okazaki O, Hara H, Hiroi Y. Pacemaker malfunction after acute myocardial infarction in a patient with wrap-around left anterior descending artery supplying the right ventricular apex. J Cardiol Cases. 2018; 18:9–12.
Article12. Bready LL, Dillman D, Noorily SH. Decision making in anesthesiology. 4th ed. Philadelphia (PA);Mosby: 2007.13. Lam C. Permanent cardiac pacemaker: an emergency perspective. Hong Kong J Emerg Med. 2001; 8:169–75.
Article14. Mozos I. Arrhythmia risk in liver cirrhosis. World J Hepatol. 2015; 7:662–72.
Article15. De Maria S Jr, Nürnberg J, Lin HM, Contreras-Saldivar AG, Levin M, Flax K, et al. Association of intraoperative blood pressure instability with adverse outcomes after liver transplantation. Minerva Anestesiol. 2013; 79:604–16.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver retransplantation for adult recipients
- Permanent Pacemaker for Syncope after Heart Transplantation with Bicaval Technique
- Portal vein fenestration: a case report of an unusual portal vein developmental anomaly
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture