Acute Crit Care.
2023 Aug;38(3):261-270. 10.4266/acc.2023.00640.
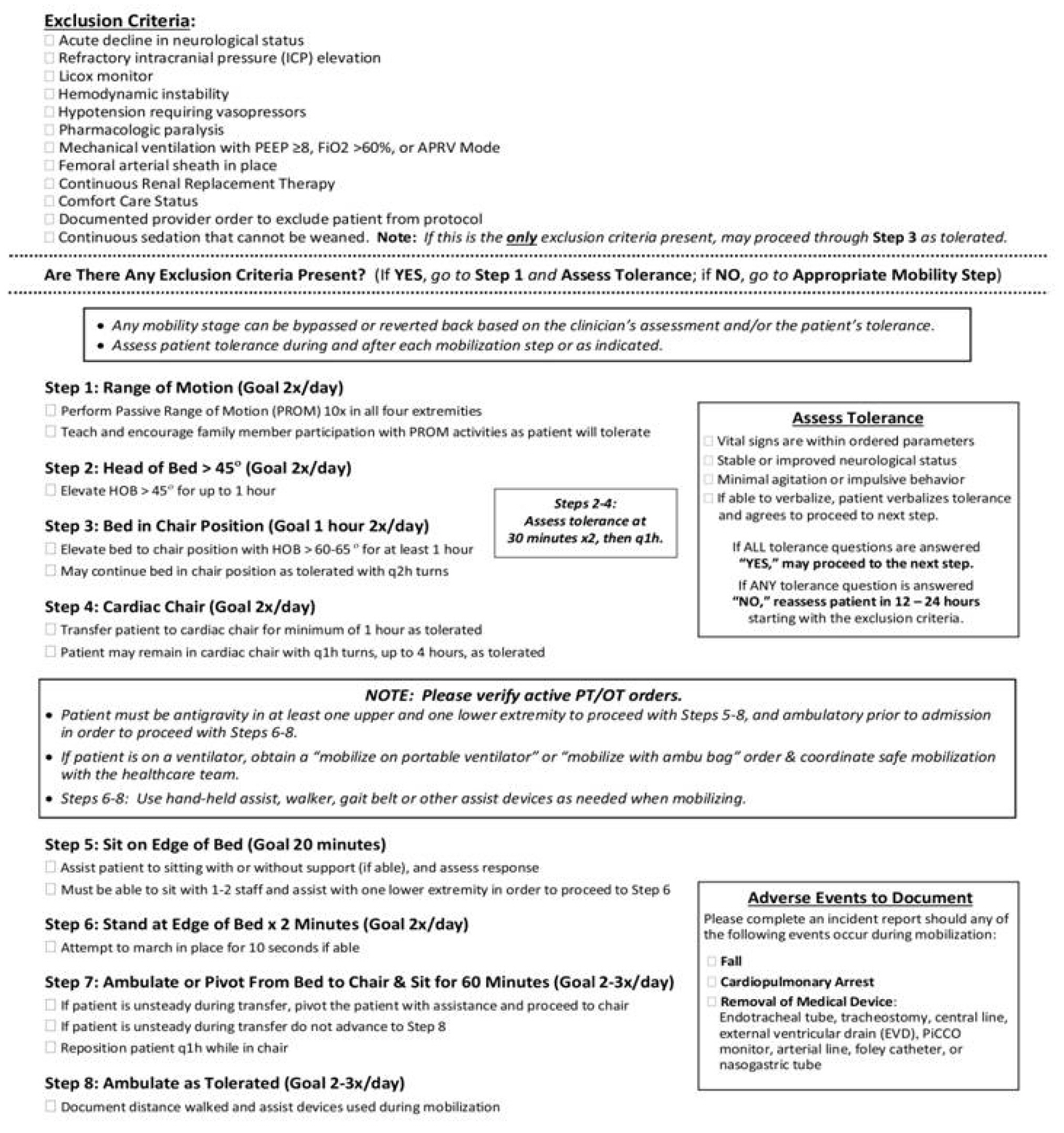
Mobilization phases in traumatic brain injury
- Affiliations
-
- 1Division of Neurosurgery, Department of Surgery, Brawijaya University/Saiful Anwar Hospital Malang, East Java, Indonesia
- 2Department of Physical Medicine and Rehabilitation, Brawijaya University/Saiful Anwar Hospital Malang, East Java, Indonesia
- KMID: 2547019
- DOI: http://doi.org/10.4266/acc.2023.00640
Abstract
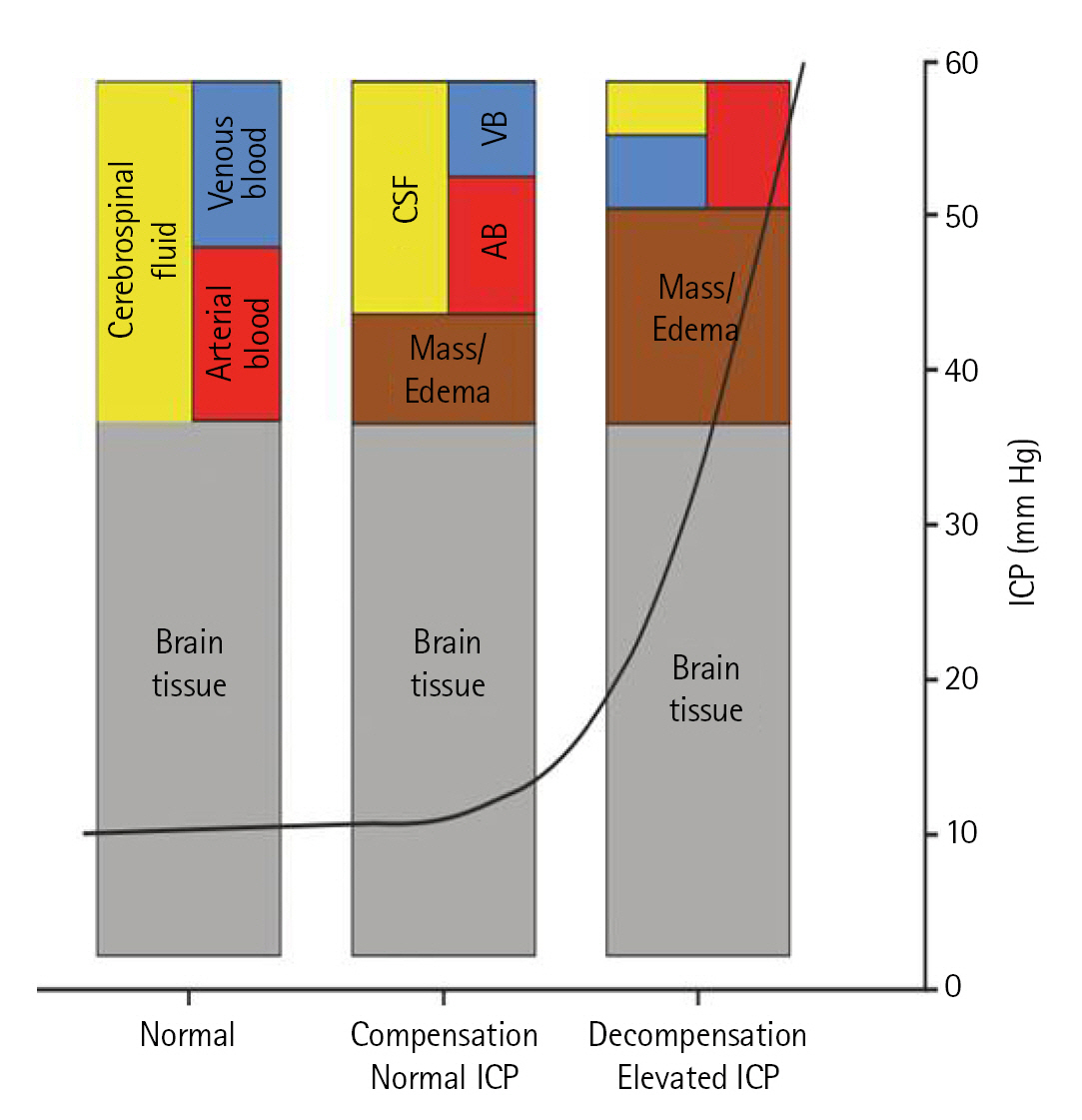
- Mobilization in traumatic brain injury (TBI) have shown the improvement of length of stay, infection, long term weakness, and disability. Primary damage as a result of trauma’s direct effect (skull fracture, hematoma, contusion, laceration, and nerve damage) and secondary damage caused by trauma’s indirect effect (microvasculature damage and pro-inflammatory cytokine) result in reduced tissue perfusion & edema. These can be facilitated through mobilization, but several precautions must be recognized as mobilization itself may further deteriorate patient’s condition. Very few studies have discussed in detail regarding mobilizing patients in TBI cases. Therefore, the scope of this review covers the detail of physiological effects, guideline, precautions, and technique of mobilization in patients with TBI.
Figure
Reference
-
1. Ai W, Venkatachalam L, Molawi SA, Kuwari FA. Traumatic brain injury rehabilitation: an overview. In : Farid Sadaka, editor. Traumatic brain injury. InTech;2014.2. Brissie MA, Zomorodi M, Soares-Sardinha S, Jordan JD. Development of a neuroearly mobilisation protocol for use in a neuroscience intensive care unit. Intensive Crit Care Nurs. 2017; 42:30–5.3. Altun Uğraş G, Yüksel S, Temiz Z, Eroğlu S, Şirin K, Turan Y. Effects of different head-of-bed elevations and body positions on intracranial pressure and cerebral perfusion pressure in neurosurgical patients. J Neurosci Nurs. 2018; 50:247–51.
Article4. Gaspari CH, Lafayette S, Jaccoud AC, Kurtz P, Lavradas LA Jr, Cavalcanti DD. Safety and feasibility of out-of-bed mobilization for patients with external ventricular drains in a neurosurgical intensive care unit. J Acute Care Phys Ther. 2018; 9:171–8.
Article5. Kawoos U, McCarron RM, Auker CR, Chavko M. Advances in intracranial pressuremonitoring and its significance in managing traumatic brain injury. Int J Mol Sci. 2015; 16:28979–97.6. Thal SC. Intensive care management of head-injured patient. In : Prabhakar H, Ali Z, editors. Textbook of neuroanesthesia and neurocritical care. Springer Singapore;2019. p. 157–65.7. Petersen LG, Petersen JC, Andresen M, Secher NH, Juhler M. Posturalinfluence on intracranial and cerebral perfusion pressure in ambulatoryneurosurgical patients. Am J Physiol Regul Integr Comp Physiol. 2016; 310:R100–4.8. Chitteti P, George AS, Nair S, Karuppasamy R, Joseph M. Adherence to head-of-bed elevation in traumatic brain injury: an audit. J Neuroanaesthesiol Crit Care. 2022; 9:177–82.
Article9. Sattur MG, Patel SJ, Helke KL, Donohoe M, Spiotta AM. Head elevation, cerebral venous system, and intracranial pressure: review and hypothesis. Stroke Vasc Interv Neurol. 2022; 3:e000522.
Article10. Mahfoud F, Beck J, Raabe A. Intracranial pressure pulse amplitude duringchanges in head elevation: a new parameter for determining optimum cerebralperfusion pressure? Acta Neurochir (Wien). 2010; 152:443–50.11. Mitchell PH, Kirkness C, Blissitt PA. Chapter 5 cerebral perfusion pressureand intracranial pressure in traumatic brain injury. Annu Rev Nurs Res. 2015; 33:111–83.
Article12. Sands E, Wong L, Lam MY, Panerai RB, Robinson TG, Minhas JS. The effects ofgradual change in head positioning on the relationship between systemic andcerebral haemodynamic parameters in healthy controls and acute ischaemic strokepatients. Brain Sci. 2020; 10:582.
Article13. Nagarathinam V, Muthusamy R, Ramachandran S. Effectiveness of mobilization to sitting in improving arousal at various durations in traumatic brain injury patients. Indian J Public Health Res Dev. 2019; 10:399–404.
Article14. Young B, Moyer M, Pino W, Kung D, Zager E, Kumar MA. Safety and feasibilityof early mobilization in patients with subarachnoid hemorrhage and externalventricular drain. Neurocrit Care. 2019; 31:88–96.
Article15. Borges LF, Fraga Righetti R, de Souza Francisco D, Pereira Yamaguti W. Hemodynamic impact of early mobilization in critical patients receivingvasoactive drugs: a prospective cohort study. PLoS One. 2022; 17:e0279269.16. Tipping CJ, Bailey MJ, Bellomo R, Berney S, Buhr H, Denehy L, et al. The ICU Mobility Scale has constructand predictive validity and is responsive: a multicenter observational study. Ann Am Thorac Soc. 2016; 13:887–93.17. Sommers J, Engelbert RH, Dettling-Ihnenfeldt D, Gosselink R, Spronk PE, Nollet F, et al. Physiotherapy in the intensive care unit: anevidence-based, expert driven, practical statement and rehabilitationrecommendations. Clin Rehabil. 2015; 29:1051–63.
Article18. Kisner C, Colby LA, Borstad J. Therapeutic exercise: foundations and techniques. 7th ed. F. A. Davis Company;2018.19. Seo B, Shin WS. Effects of functional training on strength, function level, and quality of life of persons in intensive care units. Phys Ther Rehabil Sci. 2019; 8:134–40.
Article20. Kocan MJ, Lietz H. Special considerations for mobilizing patients in the neurointensive care unit. Crit Care Nurs Q. 2013; 36:50–5.
Article21. Monaghan HM, McWilliams D, Cook S, Klein LM, Kumble KS, Friedman M, et al. Early mobility. Int J Safe Patient Handl Mov. 2022; special issue:SI–35.22. Kubota S, Endo Y, Kubota M, Ishizuka Y, Furudate T. Effects of trunk posturein Fowler’s position on hemodynamics. Auton Neurosci. 2015; 189:56–9.23. Vatwani A. Caregiver guide and instructions for safe bed mobility. Arch PhysMed Rehabil. 2017; 98:1907–10.
Article24. Cifu DX, Johns JS. Braddom’s physical medicine and rehabilitation. 6th ed. Elsevier;2021.25. Sharma B, Allison D, Tucker P, Mabbott D, Timmons BW. Cognitive and neuraleffects of exercise following traumatic brain injury: a systematic review ofrandomized and controlled clinical trials. Brain Inj. 2020; 34:149–59.26. Dresen E, Weißbrich C, Fimmers R, Putensen C, Stehle P. Medical high-proteinnutrition therapy and loss of muscle mass in adult ICU patients: a randomizedcontrolled trial. Clin Nutr. 2021; 40:1562–70.27. Bear DE, Puthucheary Z. Potential nutritional strategies to reduce muscle wasting in early critical illnes. ICU Manag Pract. 2016; 16:109–11.28. Zhou W, Yu L, Fan Y, Shi B, Wang X, Chen T, et al. Effect of early mobilization combined with early nutrition on acquired weakness in critically ill patients (EMAS): a dual-center, randomized controlled trial. PLoS One. 2022; 17:e0268599.
Article29. Chapple LS, Parry SM, Schaller SJ. Attenuating muscle mass loss in criticalillness: the role of nutrition and exercise. Curr Osteoporos Rep. 2022; 20:290–308.
Article