J Korean Med Sci.
2023 Oct;38(39):e303. 10.3346/jkms.2023.38.e303.
Patient Anxiety and Communication Experience in the Emergency Department: A Mobile, Web-Based, Mixed-Methods Study on Patient Isolation During the COVID-19 Pandemic
- Affiliations
-
- 1Department of Digital Health, Samsung Advanced Institute for Health Science & Technology (SAIHST), Sungkyunkwan University, Seoul, Korea
- 2Department of Emergency Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Digital Innovation Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2546928
- DOI: http://doi.org/10.3346/jkms.2023.38.e303
Abstract
- Background
Anxiety and communication difficulties in the emergency department (ED) may increase for various reasons, including isolation due to coronavirus disease 2019 (COVID-19). However, little research on anxiety and communication in EDs exists. This study explored the isolation-related anxiety and communication experiences of ED patients during the COVID-19 pandemic.
Methods
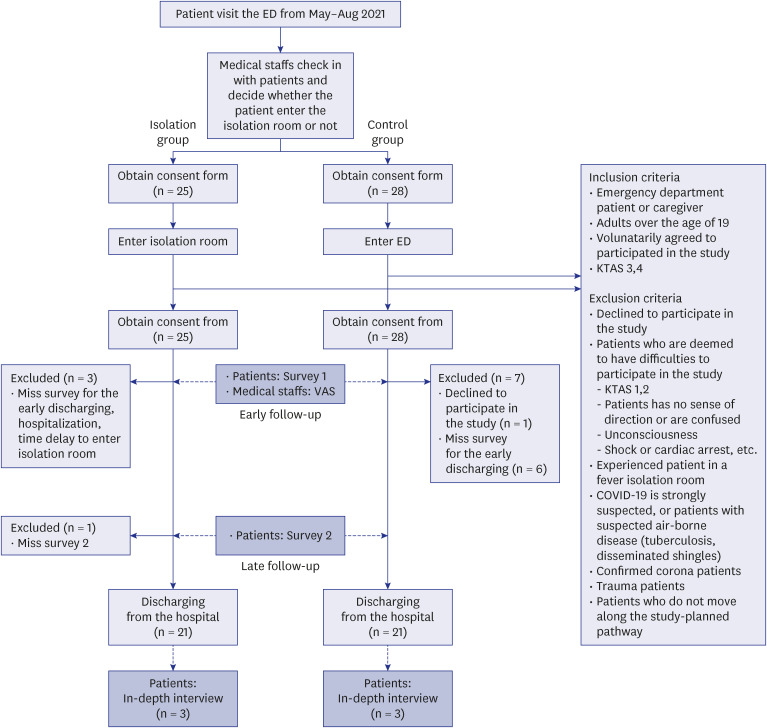
A prospective mixed-methods study was conducted from May to August 2021 at the Samsung Medical Center ED, Seoul. There were two patient groups: isolation and control. Patients measured their anxiety using the State-Trait Anxiety Inventory (STAI X1) at two time points, and we surveyed patients at two time points about factors contributing to their anxiety and communication experiences. These were measured through a mobile web-based survey. Researchers interviewed patients after their discharge.
Results
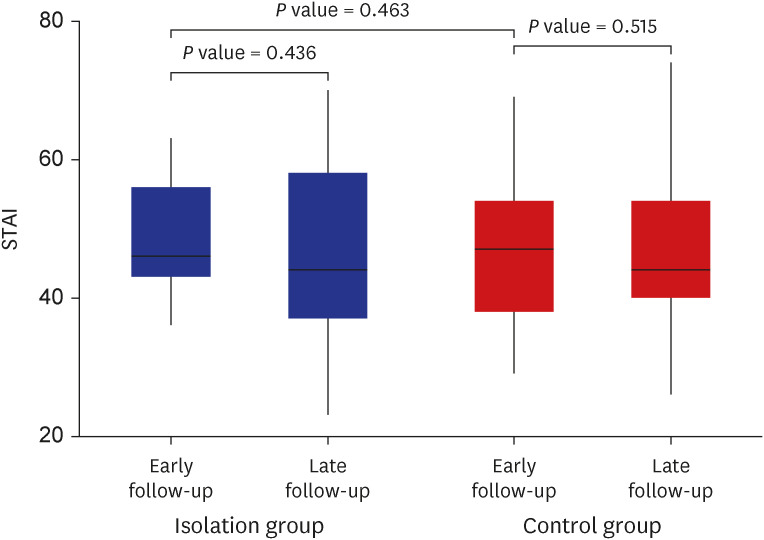
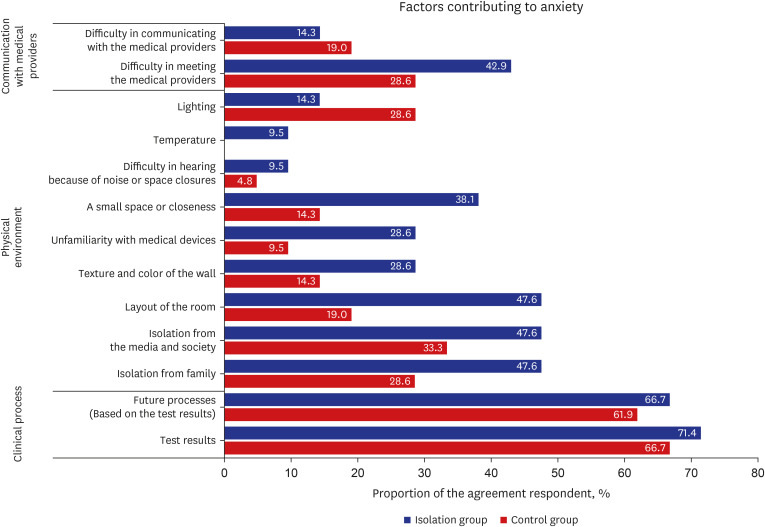
ED patients were not anxious regardless of isolation, and there was no statistical significance between each group at the two time points. STAI X1 was 48.4 (standard deviation [SD], 8.0) and 47.3 (SD, 10.9) for early follow-up and 46.3 (SD, 13.0) and 46.2 (SD, 13.6) for late follow-up for the isolation and control groups, respectively. The clinical process was the greatest factor contributing to anxiety as opposed to the physical environment or communication. Communication was satisfactory in 71.4% of the isolation group and 66.7% of the control group. The most important aspects of communication were information about the clinical process and patient status.
Conclusion
ED patients were not anxious and were generally satisfied with medical providers’ communication regardless of their isolation status. However, patients need clinical process information for anxiety reduction and better communication.
Figure
Reference
-
1. Rajendran N, Mitra TP, Shahrestani S, Coggins A. Randomized controlled trial of adult therapeutic coloring for the management of significant anxiety in the emergency department. Acad Emerg Med. 2020; 27(2):92–99. PMID: 31957143.2. Marchesi C, Brusamonti E, Borghi C, Giannini A, Di Ruvo R, Minneo F, et al. Anxiety and depressive disorders in an emergency department ward of a general hospital: a control study. Emerg Med J. 2004; 21(2):175–179. PMID: 14988342.3. Shdaifat SA, Al Qadire M. Anxiety and depression among patients admitted to intensive care. Nurs Crit Care. 2022; 27(1):106–112. PMID: 32844542.4. Yang I, Kim H, Jang Y, Kang YA. Associations among uncertainty, depression, and anxiety in isolated inpatients. J Korean Acad Psychiatr Ment Health Nurs. 2019; 28(3):216–225.5. Abar B, Holub A, Lee J, DeRienzo V, Nobay F. Depression and anxiety among emergency department patients: utilization and barriers to care. Acad Emerg Med. 2017; 24(10):1286–1289. PMID: 28741875.6. Nikumb VB, Banerjee A, Kaur G, Chaudhury S. Impact of doctor-patient communication on preoperative anxiety: study at industrial township, Pimpri, Pune. Ind Psychiatry J. 2009; 18(1):19–21. PMID: 21234156.7. Wittenberg E, Goldsmith JV, Chen C, Prince-Paul M, Johnson RR. Opportunities to improve COVID-19 provider communication resources: a systematic review. Patient Educ Couns. 2021; 104(3):438–451. PMID: 33455825.8. Blackburn J, Ousey K, Goodwin E. Information and communication in the emergency department. Int Emerg Nurs. 2019; 42:30–35. PMID: 30122462.9. Fang J, Liu YT, Lee EY, Yadav K. Telehealth solutions for in-hospital communication with patients under isolation during COVID-19. West J Emerg Med. 2020; 21(4):801–806. PMID: 32726245.10. Park J, Lim T. Korean triage and acuity scale (KTAS). J Korean Soc Emerg Med. 2017; 28(6):547–551.11. Kim D, Jung W, Yu JY, Chang H, Lee SU, Kim T, et al. Effect of fever or respiratory symptoms on leaving without being seen during the COVID-19 pandemic in South Korea. Clin Exp Emerg Med. 2022; 9(1):1–9. PMID: 35354228.12. Spielberger C, Gorsuch R, Lushene R. Manual for the State-Trait Anxiety, Inventory. Palo Alto, CA, USA: Consulting Psychologists Press;1970.13. Marshall GN, Hays RD. The Patient Satisfaction Questionnaire Short-Form (PSQ-18). Santa Monica, CA, USA: RAND;1994.14. Khan AH, Sultana MS, Hossain S, Hasan MT, Ahmed HU, Sikder MT. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. J Affect Disord. 2020; 277:121–128. PMID: 32818775.15. Khademi F, Rassouli M, Rafiei F, Moayedi S, Torres M, Marzban N, et al. The effect of mandala colouring on anxiety in hospitalized COVID-19 patients: a randomized controlled clinical trial. Int J Ment Health Nurs. 2021; 30(Suppl 1):Suppl 1. 1437–1444. PMID: 34143568.16. Sonis JD, Aaronson EL, Lee RY, Philpotts LL, White BA. Emergency department patient experience: a systematic review of the literature. J Patient Exp. 2018; 5(2):101–106. PMID: 29978025.17. Weinick RM, Becker K, Parast L, Stucky BD, Elliott MN, Mathews M, et al. Emergency department patient experience of care survey: development and field test. Rand Health Q. 2014; 4(3):5.18. Atrium Health Wake Forest Baptist. About the Press Ganey patient experience survey. Updated 2022. Accessed May 1, 2022. https://www.wakehealth.edu/About-Us/Quality-and-Awards/Quality-and-Safety-Measures/Patient-Experience/About-the-Press-Ganey-Patient-Experience-Survey .19. Ekwall A. Acuity and anxiety from the patient’s perspective in the emergency department. J Emerg Nurs. 2013; 39(6):534–538. PMID: 24209586.20. Huang YH, Sabljak LA, Puhala ZA. Emergency department patient experience and waiting time. Am J Emerg Med. 2018; 36(3):510–511. PMID: 28847627.21. Sonis JD, Aaronson EL, Castagna A, White B. A conceptual model for emergency department patient experience. J Patient Exp. 2019; 6(3):173–178. PMID: 31535004.22. Yuan K, Zheng YB, Wang YJ, Sun YK, Gong YM, Huang YT, et al. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: a call to action. Mol Psychiatry. 2022; 27(8):3214–3222. PMID: 35668158.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Mobile Web-Based COVID-19 Isolation Hospitalization Management Training on Patient Uncertainty, Anxiety and Nursing Education Satisfaction
- Need for Information and Communication Technology during COVID-19: An Exploratory Study Using Nurses’ Activity Diaries
- The impact of the COVID-19 pandemic on in-hospital mortality in patients admitted through the emergency department
- The effect of regional distribution of isolation rooms in emergency departments on ambulance travel time during the COVID-19 pandemic
- Assessment and Management of Dysphagia during the COVID-19 Pandemic