Healthc Inform Res.
2023 Jul;29(3):256-268. 10.4258/hir.2023.29.3.256.
Need for Information and Communication Technology during COVID-19: An Exploratory Study Using Nurses’ Activity Diaries
- Affiliations
-
- 1College of Nursing, Gachon University, Incheon, Korea
- 2Gachon University Gil Medical Center, Incheon, Korea
- 3Maria Fertility Hospital, Seoul, Korea
- KMID: 2544877
- DOI: http://doi.org/10.4258/hir.2023.29.3.256
Abstract
Objectives
The coronavirus disease 2019 (COVID-19) pandemic has led to high levels of burnout among nurses. Information and communication technology (ICT) may offer a solution to prevent a potential collapse in healthcare. The aim of this study was to identify areas where ICT could provide support, by analyzing the work of nurses during the COVID-19 pandemic.
Methods
This retrospective exploratory descriptive study analyzed qualitative data from the activity diaries of seven nurses working in COVID-19 wards or intensive care units.
Results
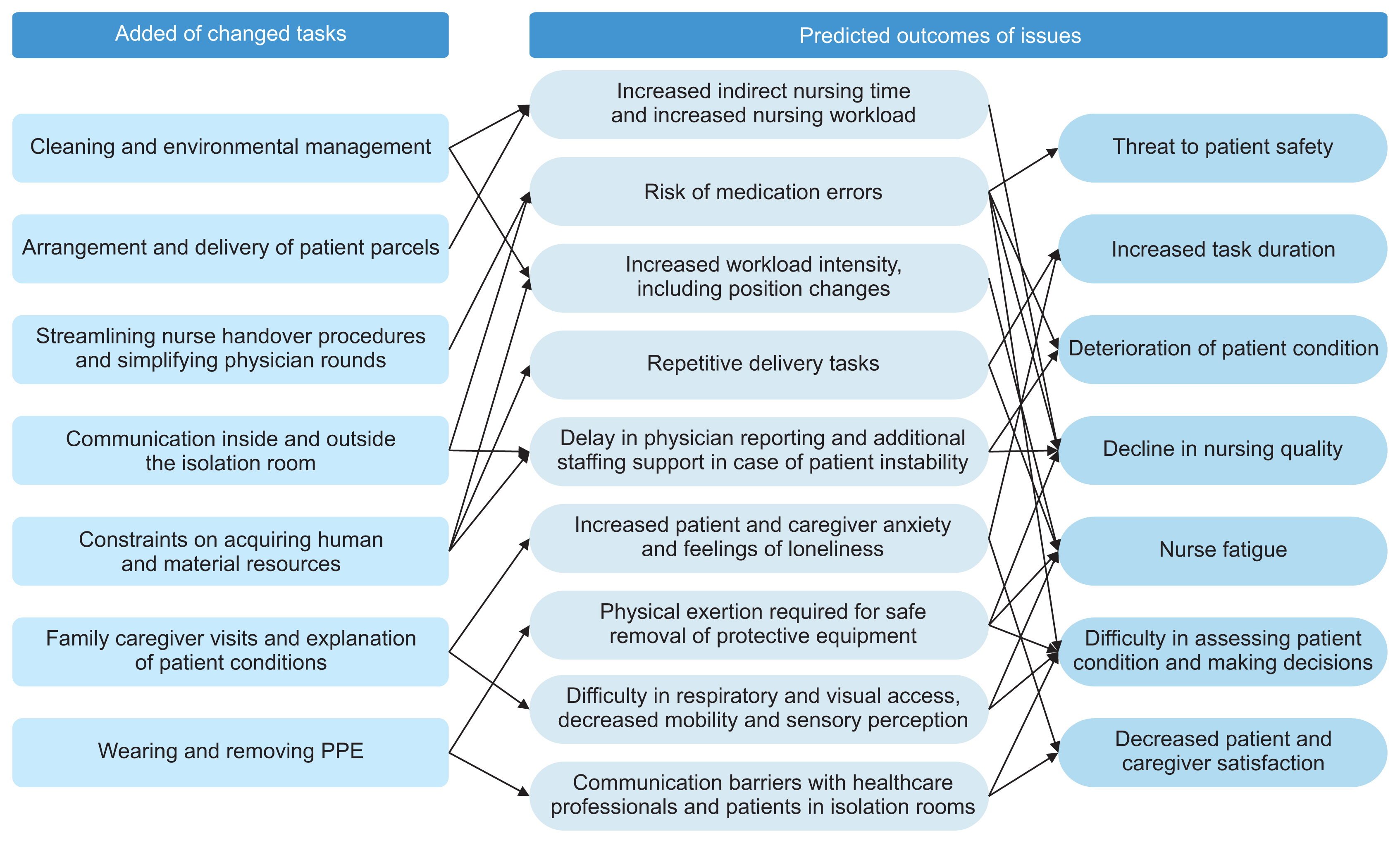
The nursing work process during COVID-19 involved “added tasks,” “changed tasks,” and “reduced tasks” compared to the pre-COVID-19 situation. Nurses reported difficulties in communicating with other healthcare professionals both inside and outside the isolation room, as well as with patients. The use of various ICT solutions, such as real-time video-conferencing systems or mobile robots, could enhance patient monitoring in the isolation room and improve the quality and efficiency of communication.
Conclusions
The changes in work tasks not only led to nurse exhaustion but also negatively impacted the quality of care. ICT solutions should be explored to minimize the time spent in the isolation room, thereby reducing the risk of infection spread. This could also enhance communication among patients, family caregivers, and healthcare professionals.
Figure
Reference
-
References
1. World Health Organization. Coronavirus (COVID-19) dashboard [Internet]. Geneva, Switzerland: World Health Organization;c2023. [cited at 2023 Jul 22]. Available from: https://covid19.who.int.2. Pan Y, Guan H, Zhou S, Wang Y, Li Q, Zhu T, et al. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020; 30(6):3306–9. https://doi.org/10.1007/s00330-020-06731-x.
Article3. Nayna Schwerdtle P, Connell CJ, Lee S, Plummer V, Russo PL, Endacott R, et al. Nurse expertise: a critical resource in the COVID-19 pandemic response. Ann Glob Health. 2020; 86(1):49. https://doi.org/10.5334/aogh.2898.
Article4. Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020; 48(6):592–8. https://doi.org/10.1016/j.ajic.2020.03.018.
Article5. Lucchini A, Iozzo P, Bambi S. Nursing workload in the COVID-19 era. Intensive Crit Care Nurs. 2020; 61:102929. https://doi.org/10.1016/j.iccn.2020.102929.
Article6. Mo Y, Deng L, Zhang L, Lang Q, Liao C, Wang N, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag. 2020; 28(5):1002–9. https://doi.org/10.1111/jonm.13014.
Article7. Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. 2021; 77(8):3286–302. https://doi.org/10.1111/jan.14839.
Article8. Liu X, Chen J, Wang D, Li X, Wang E, Jin Y, et al. COVID-19 outbreak can change the job burnout in health care professionals. Front Psychiatry. 2020; 11:563781. https://doi.org/10.3389/fpsyt.2020.563781.
Article9. Nishimura Y, Miyoshi T, Hagiya H, Kosaki Y, Otsuka F. Burnout of healthcare workers amid the COVID-19 pandemic: a Japanese cross-sectional survey. Int J Environ Res Public Health. 2021; 18(5):2434. https://doi.org/10.3390/ijerph18052434.
Article10. Loh TP, Horvath AR, Wang CB, Koch D, Adeli K, Mancini N, et al. Operational considerations and challenges of biochemistry laboratories during the COVID-19 outbreak: an IFCC global survey. Clin Chem Lab Med. 2020; 58(9):1441–9. https://doi.org/10.1515/cclm-2020-0710.
Article11. Rouleau G, Gagnon MP, Cote J, Payne-Gagnon J, Hudson E, Dubois CA. Impact of information and communication technologies on nursing care: results of an overview of systematic reviews. J Med Internet Res. 2017; 19(4):e122. https://doi.org/10.2196/jmir.6686.
Article12. Dykes S, Chu CH. Now more than ever, nurses need to be involved in technology design: lessons from the COVID-19 pandemic. J Clin Nurs. 2021; 30(7–8):e25–8. https://doi.org/10.1111/jocn.15581.
Article13. Oddsdottir EJ, Sveinsdottir H. The content of the work of clinical nurse specialists described by use of daily activity diaries. J Clin Nurs. 2011; 20(9–10):1393–404. https://doi.org/10.1111/j.1365-2702.2010.03652.x.
Article14. Humphreys A, Richardson J, Stenhouse E, Watkins M. Assessing the impact of nurse and allied health professional consultants: developing an activity diary. J Clin Nurs. 2010; 19(17–18):2565–73. https://doi.org/10.1111/j.1365-2702.2009.03022.x.
Article15. Gibson V. An analysis of the use of diaries as a data collection method. Nurse Res. 1995; 3(1):66–73. https://doi.org/10.7748/nr.3.1.66.s8.
Article16. Goemaes R, Lernout E, Goossens S, Decoene E, Verhaeghe S, Beeckman D, et al. Time use of advanced practice nurses in hospitals: a cross-sectional study. J Adv Nurs. 2019; 75(12):3588–601. https://doi.org/10.1111/jan.14198.
Article17. Sveinsdottir H, Blondal K, Jonsdottir HH, Bragadottir H. The content of nurse unit managers’ work: a descriptive study using daily activity diaries. Scand J Caring Sci. 2018; 32(2):861–70. https://doi.org/10.1111/scs.12517.
Article18. Jin D, Lee G. Experiences of nurses at a general hospital in Seoul which is temporarily closed due to COVID-19. J Korean Acad Soc Nurs Educ. 2020; 26(4):412–22. https://doi.org/10.5977/jkasne.2020.26.4.412.
Article19. Kim K, Lee O. Knowledge, attitudes and perceptions of nurses on personal protective equipment: response to the middle east respiratory syndrome coronavirus. J Korean Acad Fundam Nurs. 2016; 23(4):402–10. https://doi.org/10.7739/jkafn.2016.23.4.402.
Article20. Noh EY, Chai YJ, Kim HJ, Kim E, Park YH. Nurses’ experience with caring for COVID-19 patients in a negative pressure room amid the pandemic situation. J Korean Acad Nurs. 2021; 51(5):585–96. https://doi.org/10.4040/jkan.21148.
Article21. Xia W, Fu L, Liao H, Yang C, Guo H, Bian Z. The physical and psychological effects of personal protective equipment on health care workers in Wuhan, China: a cross-sectional survey study. J Emerg Nurs. 2020; 46(6):791–801. https://doi.org/10.1016/j.jen.2020.08.004.
Article22. Hayes LJ, O’Brien-Pallas L, Duffield C, Shamian J, Buchan J, Hughes F, et al. Nurse turnover: a literature review: an update. Int J Nurs Stud. 2012; 49(7):887–905. https://doi.org/10.1016/j.ijnurstu.2011.10.001.
Article23. Cho SH, Kim YS, Yeon KN, You SJ, Lee ID. Effects of increasing nurse staffing on missed nursing care. Int Nurs Rev. 2015; 62(2):267–74. https://doi.org/10.1111/inr.12173.
Article24. Seidita V, Lanza F, Pipitone A, Chella A. Robots as intelligent assistants to face COVID-19 pandemic. Brief Bioinform. 2021; 22(2):823–31. https://doi.org/10.1093/bib/bbaa361.
Article25. Randmaa M, Martensson G, Leo Swenne C, Engstrom M. SBAR improves communication and safety climate and decreases incident reports due to communication errors in an anaesthetic clinic: a prospective intervention study. BMJ Open. 2014; 4(1):e004268. https://doi.org/10.1136/bmjopen-2013-004268.
Article26. Lee H, Kim J, Kim S, Kong HJ, Ryu H. Investigating the need for point-of-care robots to support teleconsultation. Telemed J E Health. 2019; 25(12):1165–73. https://doi.org/10.1089/tmj.2018.0255.
Article27. Ajami S. Use of speech-to-text technology for documentation by healthcare providers. Natl Med J India. 2016; 29(3):148–52.28. Naylor MD, Shaid EC, Carpenter D, Gass B, Levine C, Li J, et al. Components of comprehensive and effective transitional care. J Am Geriatr Soc. 2017; 65(6):1119–25. https://doi.org/10.1111/jgs.14782.
Article29. Woo D, Yu H, Kim HJ, Choi M, Kim DH. Untact visit service development based on an application reflecting the circumstances during COVID-19: focusing on utilization in the pediatric intensive care units. J Korean Acad Nurs. 2021; 51(5):573–84. https://doi.org/10.4040/jkan.21143.
Article30. Walton V, Hogden A, Long JC, Johnson J, Greenfield D. Clinicians’ perceptions of rounding processes and effectiveness of clinical communication. J Eval Clin Pract. 2020; 26(3):801–11. https://doi.org/10.1111/jep.13248.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Influence of Infection Control Fatigue and Compassion Competence on Disaster Nursing Core Competencies of Nurses at COVID-19 Designated Hospitals
- An Exploratory Study on Current Nursing Issues in the COVID-19 era through Newspaper Articles: The Application of Text Network Analysis
- Factors Influencing the COVID-19 Vaccination Intentions in Nurses: Korea, February 2021
- Influence of COVID-19-related Nursing Experience on Job Stress of Nurses
- The Influence of Long-term Care Hospital Nurses' Nursing Professionalism and Knowledge of COVID-19 on Nursing Intentions for COVID-19 Patients