Ann Surg Treat Res.
2023 Oct;105(4):188-197. 10.4174/astr.2023.105.4.188.
Specialty impact on residents’ perceived quality of life, stress, and job satisfaction: a comparative study
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- 2Department of Plastic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Division of Acute Care Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 4Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 5Department of Medical Education, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2546781
- DOI: http://doi.org/10.4174/astr.2023.105.4.188
Abstract
- Purpose
Specialty choice in residency training has a significant impact on an individual’s career and satisfaction, as well as the supply-demand imbalance in the healthcare system. The current study aimed to investigate the quality of life (QOL), stress, self-confidence, and job satisfaction of residents, and to explore factors associated with such variables, including postgraduate year, sex, and especially specialty, through a cross-sectional survey.
Methods
An online survey was administered to residents at 2 affiliated teaching hospitals. The survey had a total of 46 items encompassing overall residency life such as workload, QOL, stress, confidence, relationship, harassment, and satisfaction. Related survey items were then reconstructed into 4 key categories through exploratory factor analysis for comparison according to group classification.
Results
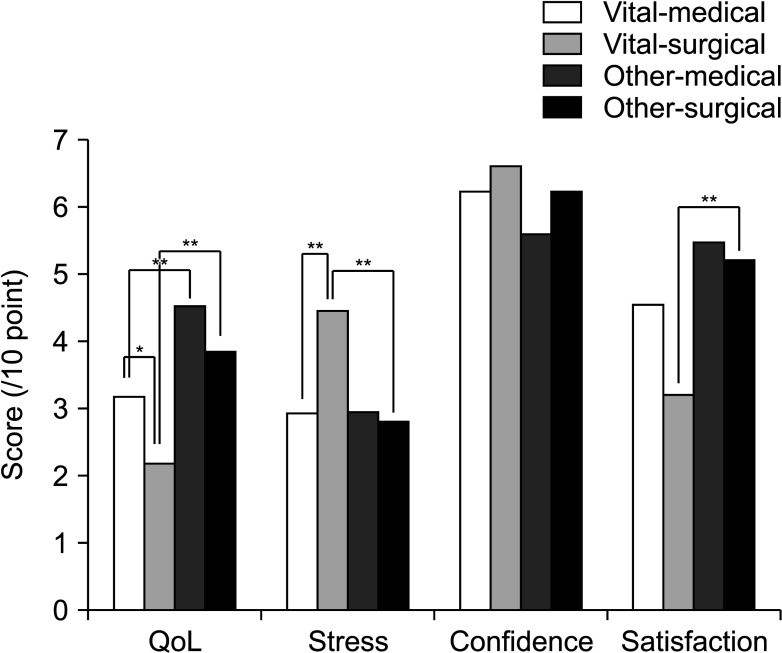
The weekly work hours of residents in vital and other specialties were similar, but residents in vital specialties had significantly more on-call days per month. Residents in vital specialties had significantly lower scores for QOL and satisfaction. Specifically, vital-surgical residents had significantly lower QOL scores and higher stress scores than the other specialty groups. Satisfaction scores were also lowest among vital-surgical residents, with a marginal difference from vital-medical, and a significant difference from other-surgical residents. Female residents had significantly lower satisfaction scores than their male counterparts.
Conclusion
Residents in vital specialties, particularly vital-surgical specialties, experience significantly worse working conditions across multiple dimensions. It is necessary to improve not only the quantity but also the quality of the system in terms of resource allocation and prioritization.
Figure
Reference
-
1. Levinson DJ. A conception of adult development. Am Psychol. 1986; 41:3–13.
Article2. Korean Intern Resident Association (KIRA). Press release from the KIRA 20230126: KIRA, announcement of the 2022 major survey results [Internet]. KIRA;2023. cited 2023 May 15. Available from: http://youngmd.org/155/?idx=14000754&bmode=view .3. Cohen JS, Patten S. Well-being in residency training: a survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Med Educ. 2005; 5:21. PMID: 15972100.
Article4. Raj KS. Well-being in residency: a systematic review. J Grad Med Educ. 2016; 8:674–684. PMID: 28018531.
Article5. Rothenberger DA. Physician burnout and well-being: a systematic review and framework for action. Dis Colon Rectum. 2017; 60:567–576. PMID: 28481850.
Article6. Vo A, McLean L, McInnes MD. Medical specialty preferences in early medical school training in Canada. Int J Med Educ. 2017; 8:400–407. PMID: 29140793.
Article7. Hohf-Nova M, Hun-Pacheco R, Muñoz-Bustos D, Soto-Carriel A, Pérez-Villalobos C. When it is time to decide: factors associated to the choice of a medical specialty. Rev Med Chil. 2021; 149:1352–1359. PMID: 35319690.
Article8. Research Institute for Healthcare Policy (RHIP), Korea Medical Association (KMA). Research Report: 2017 Survey on major training and working environments [Internet]. RHIP, KMA;2017. cited 2023 May 15. Available from: https://www.rihp.re.kr/bbs/board.php?bo_table=research_report&wr_id=264&sst=wr_datetime&sod=desc&sop=and&page=3 .9. Schwartz RW, Haley JV, Williams C, Jarecky RK, Strodel WE, Young B, et al. The controllable lifestyle factor and students’ attitudes about specialty selection. Acad Med. 1990; 65:207–210. PMID: 2306321.
Article10. Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA. 2003; 290:1173–1178. PMID: 12952999.
Article11. Sobhonslidsuk A, Thakkinstian A, Satitpornkul P. Health-related quality of life and happiness within an internal medicine residency training program: a longitudinal follow-up study. J Educ Eval Health Prof. 2015; 12:3. PMID: 25748482.
Article12. Choi SM, Park YS, Yoo JH, Kim GY. Occupational stress and physical symptoms among family medicine residents. Korean J Fam Med. 2013; 34:49–57. PMID: 23372906.
Article13. Shiga T, Hifumi T, Hagiwara Y, Otani N, Tanaka H, Nakano M, et al. Career satisfaction among acute care resident physicians in Japan. Acute Med Surg. 2022; 9:e779. PMID: 36051448.
Article14. Lebares CC, Guvva EV, Ascher NL, O’Sullivan PS, Harris HW, Epel ES. Burnout and stress among us surgery residents: psychological distress and resilience. J Am Coll Surg. 2018; 226:80–90. PMID: 29107117.
Article15. Kim YG, Ryoo HW, Seo KS, Park JB, Chung JM, Kim JK, et al. Job stress, job satisfaction of emergency residents and its related factors. J Korean Soc Emerg Med. 2008; 19:749–759.16. Ha GQ, Go JT, Murayama KM, Steinemann S. Identifying sources of stress across years of general surgery residency. Hawaii J Health Soc Welf. 2020; 79:75–81. PMID: 32190839.17. Cohen JS, Leung Y, Fahey M, Hoyt L, Sinha R, Cailler L, et al. The happy docs study: a Canadian Association of Internes and Residents well-being survey examining resident physician health and satisfaction within and outside of residency training in Canada. BMC Res Notes. 2008; 1:105. PMID: 18957136.
Article18. Gavinski K, Cleveland E, Didwania AK, Feinglass JM, Sulistio MS. Relationship between confidence, gender, and career choice in internal medicine. J Gen Intern Med. 2021; 36:662–667. PMID: 32989713.
Article19. Ahn JS, Cho S, Park WJ. Changes in the health indicators of hospital medical residents during the four-year training period in Korea. J Korean Med Sci. 2022; 37:e202. PMID: 35762145.
Article20. Kwon OY, Park SY. Specialty choice preference of medical students according to personality traits by Five-Factor Model. Korean J Med Educ. 2016; 28:95–102. PMID: 26838573.
Article21. Lee CW. Gender difference and specialty preference in medical career choice. Korean J Med Educ. 2013; 25:15–21. PMID: 25804649.
Article22. Ariely D, Lanier WL. Disturbing trends in physician burnout and satisfaction with work-life balance: dealing with malady among the nation’s healers. Mayo Clin Proc. 2015; 90:1593–1596. PMID: 26653295.
Article23. Mitsouras K, Dong F, Safaoui MN, Helf SC. Student academic performance factors affecting matching into first-choice residency and competitive specialties. BMC Med Educ. 2019; 19:241. PMID: 31262294.
Article24. Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, et al. Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS One. 2018; 13:e0206840. PMID: 30418984.
Article25. Kassam A, Horton J, Shoimer I, Patten S. Predictors of well-being in resident physicians: a descriptive and psychometric study. J Grad Med Educ. 2015; 7:70–74. PMID: 26217426.
Article26. Lambert EM, Holmboe ES. The relationship between specialty choice and gender of U.S. medical students, 1990-2003. Acad Med. 2005; 80:797–802. PMID: 16123456.
Article27. Holmboe ES, Huot SJ, Brienza RS, Hawkins RE. The association of faculty and residents’ gender on faculty evaluations of internal medicine residents in 16 residencies. Acad Med. 2009; 84:381–384. PMID: 19240452.
Article28. Gong D, Winn BJ, Beal CJ, Blomquist PH, Chen RW, Culican SM, et al. Gender differences in case volume among ophthalmology residents. JAMA Ophthalmol. 2019; 137:1015–1020. PMID: 31318390.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Job Stress, Depression and Perceived Health Status on Job Satisfaction among Child Care Teachers
- The Moderating Effect of the Leisure Satisfaction in the Job Stress on Job Satisfaction of Nurses on Shift Work
- Differences in Job Stress, and Job Satisfaction according to Teaching Style, and Personality of Preceptors
- School Nurses’ Perception of Job Performance Difficulties, Job Stress, Job Identity and Job Satisfaction
- Job Stress, Job Satisfaction of Emergency Residents and Its Related Factors