Korean J Gastroenterol.
2023 Sep;82(3):137-139. 10.4166/kjg.2023.068.
Case of Esophageal Actinomycosis Occurred after Endoscopic Mucosal Resection for Subepithelial Tumor
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, 19-8 Hospital, Hanoi, Vietnam
- 2Departments of Internal Medicine, Presbyterian Medical Center, Jeonju, Korea
- 3Departments of Pathology, Presbyterian Medical Center, Jeonju, Korea
- KMID: 2546515
- DOI: http://doi.org/10.4166/kjg.2023.068
Abstract
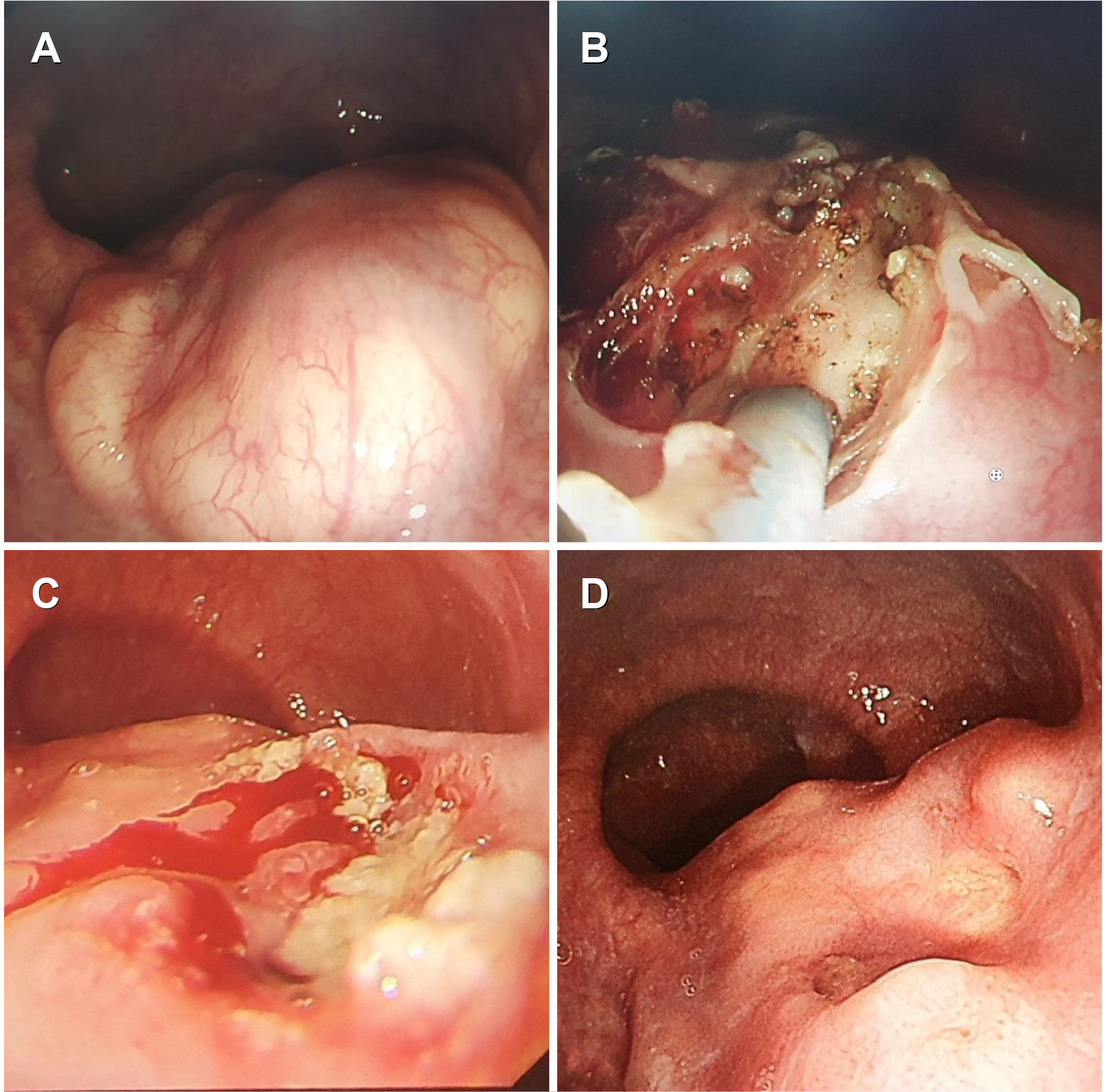
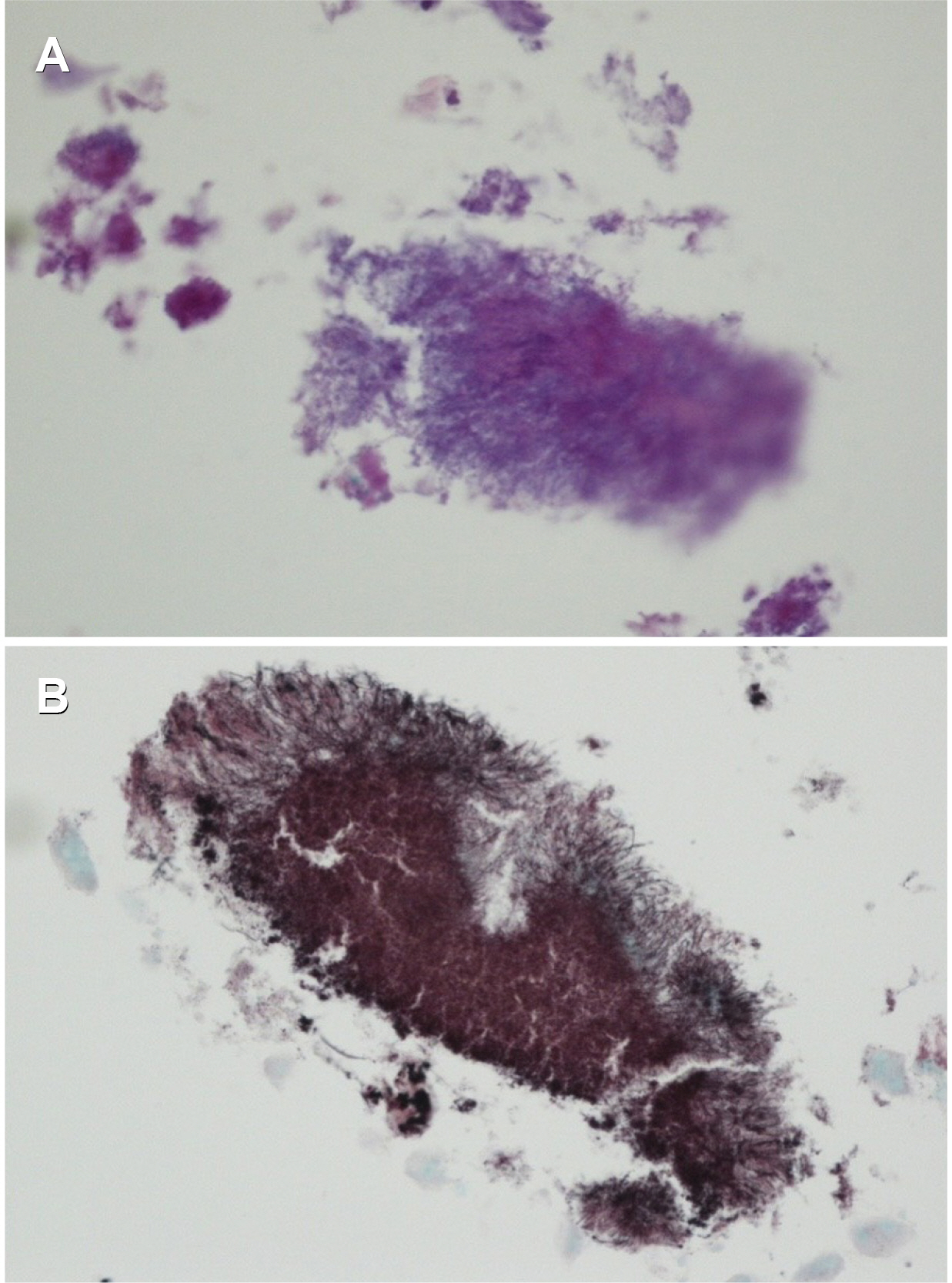
- Esophageal actinomycosis is a rare, chronic granulomatous disease caused by Actinomyces species. Endoscopy and biopsy are essential for making a diagnosis. This paper reports a case of esophageal actinomycosis that developed after an endoscopic mucosal resection (EMR) for a subepithelial tumor (SET). A 74-year-old male patient had a 3 cm flat, smooth elevation in the esophagus without symptoms. The SET was partially resected, and histology revealed “nonspecific degenerated mesenchymal tissue”. Three months later, the patient exhibited a persistently large ulceration at the EMR site, and a biopsy revealed actinomycosis. CT of the chest and abdomen revealed no abnormal findings. Ampicillin treatment was administered for six months, and the ulceration on the esophageal SET improved.
Figure
Reference
-
1. Valour F, Sénéchal A, Dupieux C, et al. 2014; Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 7:183–197. DOI: 10.2147/IDR.S39601. PMID: 25045274. PMCID: PMC4094581.2. Zhang AN, Guss D, Mohanty SR. 2019; Esophageal stricture caused by actinomyces in a patient with no apparent predisposing factors. Case Rep Gastrointest Med. 2019:7182976. DOI: 10.1155/2019/7182976. PMID: 30719360. PMCID: PMC6334373.3. Thota PN, Liu X, Sanaka MR. 2015; Dysphagia caused by esophageal actinomycosis. Clin Gastroenterol Hepatol. 13:A21–A22. DOI: 10.1016/j.cgh.2015.01.012. PMID: 25625626.4. Bonnefond S, Catroux M, Melenotte C, et al. 2016; Clinical features of actinomycosis: A retrospective, multicenter study of 28 cases of miscellaneous presentations. Medicine (Baltimore). 95:e3923. DOI: 10.1097/MD.0000000000003923. PMID: 27311002. PMCID: PMC4998488.5. Kim HS, Cheon JW, Kim MS, et al. 2013; [A case of esophageal actinomycosis in a patient with normal immunity]. Korean J Gastroenterol. 61:93–96. Korean. DOI: 10.4166/kjg.2013.61.2.93. PMID: 23458987.6. Murchan EM, Redelman-Sidi G, Patel M, Dimaio C, Seo SK. 2010; Esophageal actinomycosis in a fifty-three-year-old man with HIV: case report and review of the literature. AIDS Patient Care STDS. 24:73–78. DOI: 10.1089/apc.2009.0185. PMID: 20059353. PMCID: PMC9536338.7. Cintron JR, Del Pino A, Duarte B, Wood D. 1996; Abdominal actinomycosis. Dis Colon Rectum. 39:105–108. DOI: 10.1007/BF02048278. PMID: 8601346.8. Könönen E, Wade WG. 2015; Actinomyces and related organisms in human infections. Clin Microbiol Rev. 28:419–442. DOI: 10.1128/CMR.00100-14. PMID: 25788515. PMCID: PMC4402957.9. Alshati A, Appleton L, Maddux JT, Almohammedawi M, Dangerfield B. 2019; Esophageal actinomycosis presenting as an obstructive esophageal mass. ACG Case Rep J. 6:e00140. DOI: 10.14309/crj.0000000000000140. PMID: 31620537. PMCID: PMC6722377.10. Cho SR, Shin HW, Chang HK. 2000; Esophageal actinomycosis after insertion of esophageal stent: a case of surgical experience. Korean Thorac Cardiovasc Surg. 33:601–604.11. Weese WC, Smith IM. 1975; A study of 57 cases of actinomycosis over a 36-year period. A diagnostic 'failure' with good prognosis after treatment. Arch Intern Med. 135:1562–1568. DOI: 10.1001/archinte.1975.00330120040006. PMID: 1200725.12. Sung HY, Lee IS, Kim SI, et al. 2011; Clinical features of abdominal actinomycosis: a 15-year experience of a single institute. J Korean Med Sci. 26:932–937. DOI: 10.3346/jkms.2011.26.7.932. PMID: 21738348. PMCID: PMC3124725.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Endoscopic Mucosal Resection of a Low Esophageal Carcinoid Tumor
- Endoscopic Management of Gastric Subepithelial Tumor
- Esophageal Basaloid Squamous Carcinoma Treated by Endoscopic Resection and Radiation
- Advancements in Endoscopic Treatment for Gastric Subepithelial Tumors
- Tips and Tricks for Better Endoscopic Treatment of Colorectal Tumors: Usefulness of Cap and Band in Colorectal Endoscopic Mucosal Resection