Pediatr Emerg Med J.
2023 Oct;10(4):169-174. 10.22470/pemj.2023.00801.
A pediatric case of portosystemic shunt presenting hypoxemia with brain abscess in an emergency department
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center Children’s Hospital, Ulsan University College of Medicine, Seoul, Republic of Korea
- KMID: 2546293
- DOI: http://doi.org/10.22470/pemj.2023.00801
Abstract
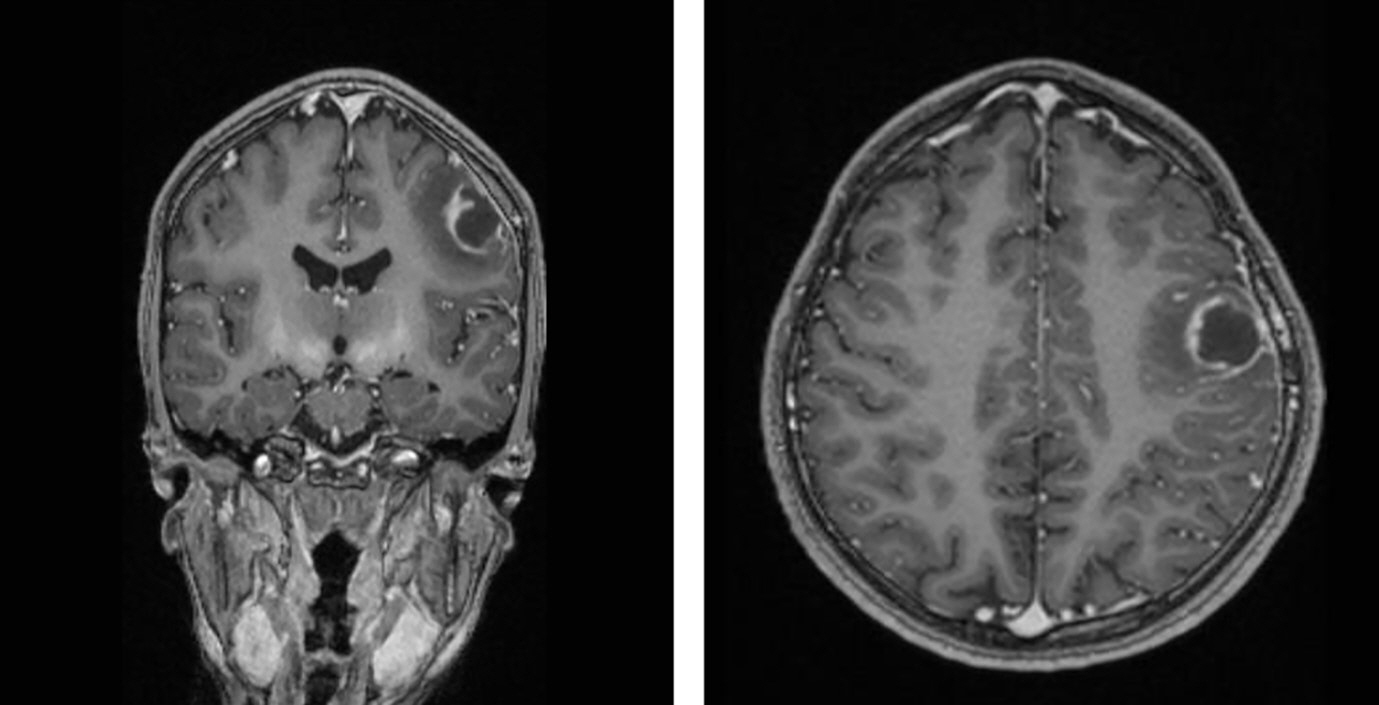
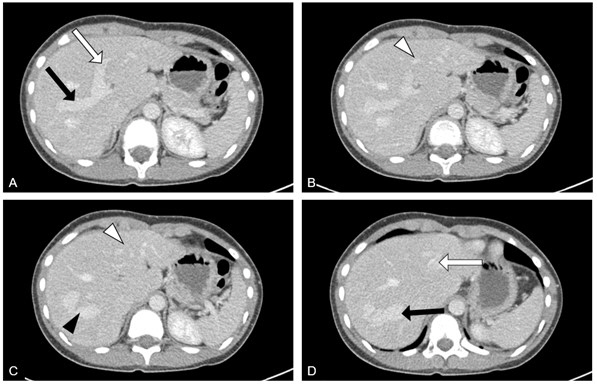
- Portosystemic shunt is a rare congenital vascular anomaly. The shunt is hard to clinically suspect because its symptoms develop insidiously and affect various systems at different time points. We report a case of an 11-year-old girl who presented with brain abscess and hypoxemia without respiratory distress. No abnormality related to the hypoxemia, such as intracardiac shunt, was found on the initial chest radiograph and echocardiogram. However, computed tomography showed a portosystemic shunt. An intrapulmonary shunt was demonstrated by bubble contrast echocardiography, indicating a grade 2 hepatopulmonary syndrome, a complication of portosystemic shunt. This case describes the diagnostic process of an unusual case presenting neurological abnormalities and hypoxemia without respiratory distress. Portosystemic shunt with hepatopulmonary syndrome should be considered in the differential diagnosis of unexplained hypoxemia.
Keyword
Figure
Reference
-
References
1. Bernard O, Franchi-Abella S, Branchereau S, Pariente D, Gauthier F, Jacquemin E. Congenital portosystemic shunts in children: recognition, evaluation, and management. Semin Liver Dis. 2012; 32:273–87.2. Lambert V, Ladarre D, Fortas F, Durand P, Herve P, Gonzales E, et al. Cardiovascular disorders in patients with congenital portosystemic shunts: 23 years of experience in a tertiary referral centre. Arch Cardiovasc Dis. 2021; 114:221–31.3. Bahadori A, Kuhlmann B, Debray D, Franchi-Abella S, Wacker J, Beghetti M, et al. Presentation of congenital portosystemic shunts in children. Children (Basel). 2022; 9:243.4. Sokollik C, Bandsma RH, Gana JC, van den Heuvel M, Ling SC. Congenital portosystemic shunt: characterization of a multisystem disease. J Pediatr Gastroenterol Nutr. 2013; 56:675–81.5. McLin VA, Franchi Abella S, Debray D, Guerin F, Beghetti M, Savale L, et al. Congenital portosystemic shunts: current diagnosis and management. J Pediatr Gastroenterol Nutr. 2019; 68:615–22.6. Bernard S, Churchill TW, Namasivayam M, Bertrand PB. Agitated saline contrast echocardiography in the identification of intra- and extracardiac shunts: connecting the dots. J Am Soc Echocardiogr. 2020 Oct 23 [Epub]. https://doi.org/10.1016/j.echo.2020.09.013.7. Bhargava P, Vaidya S, Kolokythas O, Katz DS, Dighe M. Pictorial review. Hepatic vascular shunts: embryology and imaging appearances. Br J Radiol. 2011; 84:1142–52.8. McLin V, Franchi-Abella S, Debray D, Korff S, Casotti V, Colledan M, et al. FRI-436-Congenital porto-systemic shunts in children: preliminary results from the IRCPSS [poster]. In: Proceedings of 52nd Annual Meeting ESPGHAN (European Society for Pediatric Gastroenterology, Hepatology and Nutrition); 2019 Jun 5-8; Glasgow, Scotland. ESPGHAN; http://hdl.handle.net/2078.1/216438.9. Papamichail M, Pizanias M, Heaton N. Congenital portosystemic venous shunt. Eur J Pediatr. 2018; 177:285–94.10. Lv Y, Fan D. Hepatopulmonary syndrome. Dig Dis Sci. 2015; 60:1914–23.11. Zhang J, Fallon MB. Hepatopulmonary syndrome: update on pathogenesis and clinical features. Nat Rev Gastroenterol Hepatol. 2012; 9:539–49.12. Boother EJ, Brownlow S, Tighe HC, Bamford KB, Jackson JE, Shovlin CL. Cerebral abscess associated with odontogenic bacteremias, hypoxemia, and iron loading in immunocompetent patients with right-to-left shunting through pulmonary arteriovenous malformations. Clin Infect Dis. 2017; 65:595–603.13. Bodilsen J, Dalager-Pedersen M, van de Beek D, Brouwer MC, Nielsen H. Risk factors for brain abscess: a nationwide, population-based, nested case-control study. Clin Infect Dis. 2020; 71:1040–6.14. Aggarwal V, Khan DM, Rhodes JF. Pulmonary arteriovenous malformation causing systemic hypoxemia in early infancy. Case Rep Pediatr. 2017; 2017:2841720.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intrahepatic Portosystemic Venous Shunt Presenting as a Cystic Mass in a Patient without Liver Cirrhosis: A Case Report
- Congenital Absence of the Portal Vein in an Adult Man Presenting with Portosystemic Encephalopathy: A Case Report
- A Case of Combined Intrahepatic Portosystemic Shunt, Midgut Malrotation, and Renal Rotational Anomaly in an Adult Patient
- Non-cirrhotic Hyperammonemic Encephalopathy with Portosystemic Shunt
- Delayed Cerebral Abscess as a Shunt Complication and Endoscopic Removal of the Ventricular Catheter and Abscess